When to Stop Antibiotics: What Doctors Really Say
When you’re sick, antibiotics, medications used to treat bacterial infections. Also known as antibacterial drugs, they’re powerful—but only when used correctly. Too many people stop taking them as soon as they feel better. That’s a mistake. Too few people keep taking them long enough. That’s also a mistake. The goal isn’t to feel good—it’s to kill every last bacterium. If you don’t, the survivors become resistant. And that’s how superbugs start.
Antibiotic resistance isn’t a future threat—it’s happening now. The fluoroquinolones, a class of antibiotics including ciprofloxacin and levofloxacin, are linked to permanent nerve and tendon damage. Even common ones like trimethoprim, found in Bactrim, can raise potassium to dangerous levels in older adults or people on blood pressure meds. These aren’t side effects you can ignore. And they’re not rare. The FDA and CDC have issued warnings because these drugs are overused and misused.
There’s no one-size-fits-all answer to when to stop antibiotics. A sinus infection? Maybe 5 to 7 days. A urinary tract infection? Often just 3 days now. Pneumonia? Up to 10. It depends on the bug, your age, your immune system, and whether you’re improving. Your doctor should tell you the exact duration—not just say "take until it’s gone." If they don’t, ask. And if you start feeling worse after stopping, go back. Some infections come back harder the second time.
Don’t let old habits guide you. Ten years ago, doctors told you to finish the whole bottle. Now, science says that’s often unnecessary—and risky. Shorter courses reduce side effects, lower costs, and fight resistance. But you still need to take them exactly as prescribed. Skipping doses or sharing pills with someone else? That’s how resistant bacteria spread.
You’ll find posts here that break down what happens when antibiotics go wrong: from dangerous drug interactions with blood pressure meds to how generic manufacturing quality can affect outcomes. Some posts show how to spot look-alike drug names that cause mix-ups. Others explain why some antibiotics are being phased out entirely, like chloramphenicol, because safer options exist. This isn’t about fear. It’s about control. You have the right to know how long to take your medicine, what to watch for, and when to call your doctor. That’s what these articles are for.
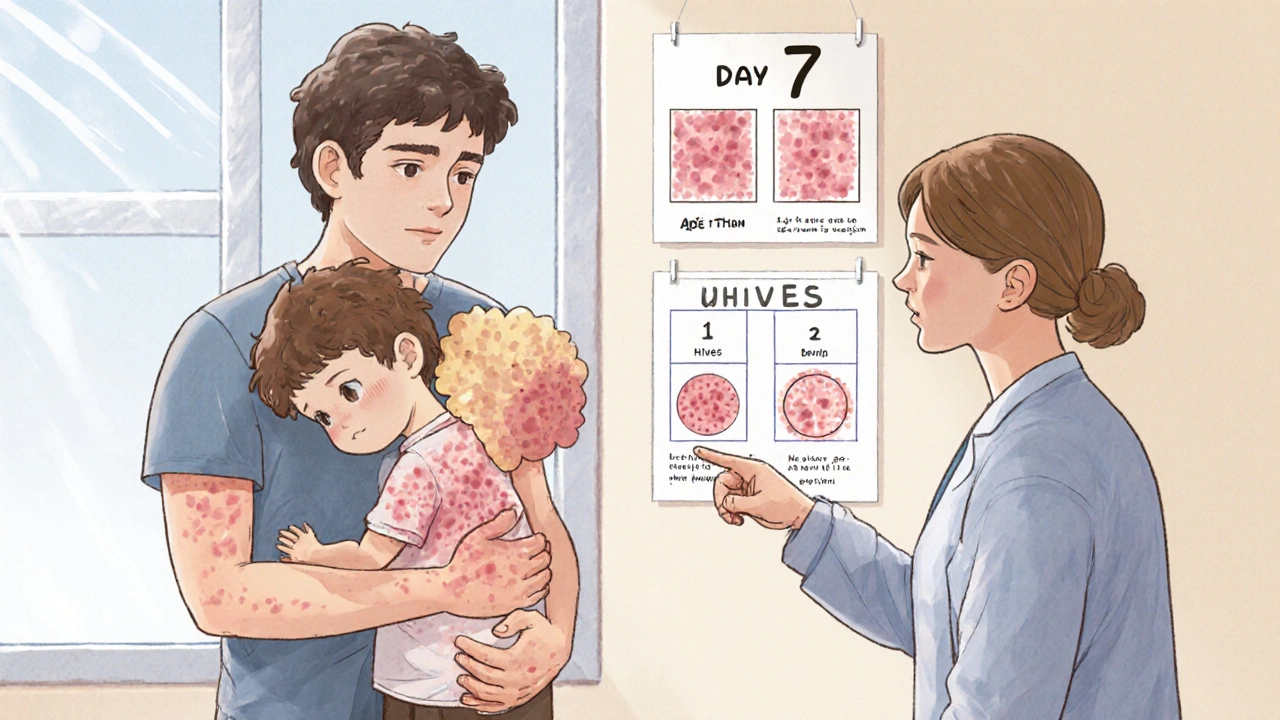
Antibiotic Rashes: When to Stop the Drug and Call the Doctor
- Robin Tudge
- November 26, 2025
- 8 Comments
Most antibiotic rashes aren’t allergies - but knowing the difference can prevent dangerous mistakes. Learn when to stop the drug and when to keep going, based on rash type, timing, and symptoms.
read more