Most parents and even some adults panic when a rash shows up after starting an antibiotic. It’s common. It’s scary. And most of the time, it’s not a true allergy. But how do you know the difference? Stopping the antibiotic when you don’t need to can make the infection worse. Keeping it going when you should stop can be dangerous. This isn’t about guessing. It’s about recognizing clear signs - and knowing exactly when to act.
Most Antibiotic Rashes Aren’t Allergies
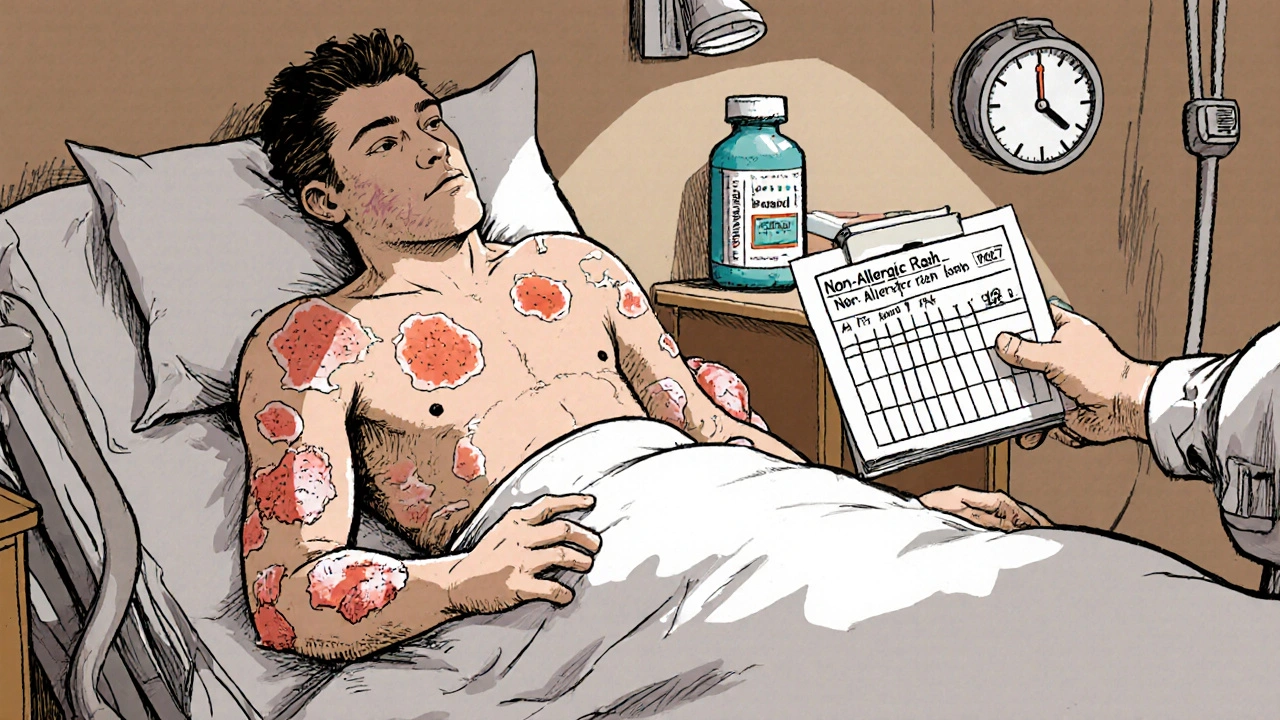
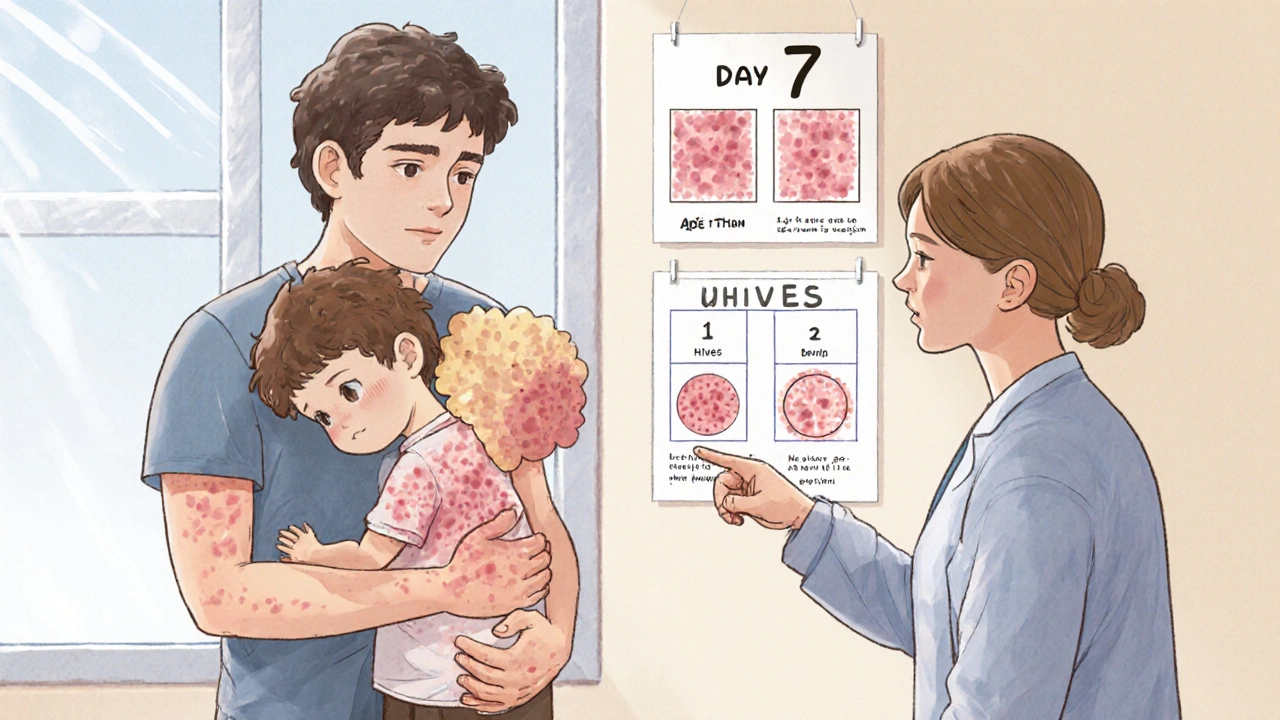
If you or your child gets a rash on day 5 or 6 of taking amoxicillin or another penicillin-based antibiotic, chances are it’s not an allergy. In fact, up to 90% of kids labeled as allergic to amoxicillin because of a rash turn out to be fine when tested properly. These rashes are called non-allergic drug eruptions. They’re common - happening in 5 to 10% of children on amoxicillin - but they’re not dangerous in themselves. These rashes usually look like small, flat, pink or red spots that spread across the chest, stomach, or back. They don’t itch much, if at all. They don’t move around. They don’t turn into big, swollen welts. And they show up late - typically between days 5 and 10 of treatment. That timing matters. True allergic reactions happen fast - within an hour of taking the pill. The rash isn’t your body rejecting the drug. It’s often linked to a virus you already have. Epstein-Barr virus (mono), colds, or other common infections can trigger this reaction when paired with amoxicillin. It’s not the antibiotic causing the problem - it’s the combo.What a True Allergic Reaction Looks Like
A real allergic reaction to antibiotics is different. It’s urgent. It’s noticeable. And it doesn’t wait. If you develop raised, red, itchy welts - like hives - within minutes to an hour after taking the antibiotic, that’s a red flag. These welts come and go. One moment they’re on your arm, the next they’re on your leg. They burn or sting. They might be accompanied by swelling around the lips, eyes, or throat. You could feel tightness in your chest, have trouble breathing, or feel dizzy. These are signs of anaphylaxis - a life-threatening reaction. You don’t wait. You stop the antibiotic immediately. You call 911 or go to the ER. If you have an epinephrine auto-injector (like an EpiPen), use it right away. Antihistamines like Benadryl help with mild itching, but they won’t stop anaphylaxis. Only epinephrine can.When a Rash Means Something Much Worse
Rare, but deadly, are severe cutaneous adverse reactions (SCARs) like Stevens-Johnson Syndrome (SJS) or toxic epidermal necrolysis (TEN). These are medical emergencies. They happen in about 1 to 6 cases per million antibiotic prescriptions - so they’re extremely rare. But if you see them, you need to act fast. These rashes start like a regular one but quickly turn into painful blisters. The skin begins to peel off in sheets, like a bad burn. You get a high fever - over 101.3°F. Your eyes, mouth, or genitals swell or develop sores. Your skin feels tender, like it’s sunburned. This isn’t a rash you treat at home. This needs hospitalization - often in a burn unit. Another rare but serious reaction is DRESS syndrome. It shows up later - around 2 to 6 weeks after starting the drug. You get a widespread rash, fever, swollen lymph nodes, and organ inflammation (like liver or kidney damage). If you have any of these symptoms, stop the antibiotic and get help immediately.
When to Keep Taking the Antibiotic
If your rash is flat, non-itchy, appears after day 5, and you feel fine otherwise - no fever, no swelling, no trouble breathing - then you should keep taking the antibiotic. This is what most pediatricians and allergists now recommend. Stopping antibiotics unnecessarily does more harm than good. A 2023 study found that when parents stop amoxicillin because of a rash, their child is 37% more likely to have a treatment failure - meaning the infection comes back worse. That often means switching to a stronger, broader-spectrum antibiotic like clindamycin or azithromycin. Those drugs are more likely to cause severe diarrhea or even C. difficile infections - which can be life-threatening. The CDC and the American Academy of Allergy, Asthma & Immunology both say: if the rash is non-urticarial (not hives), non-pruritic (not itchy), and without systemic symptoms, continue the antibiotic. You can manage mild itching with over-the-counter cetirizine (Zyrtec) or famotidine (Pepcid), and apply hydrocortisone cream to the worst spots. The rash will fade on its own in 5 to 7 days.What to Do Right Now
Don’t guess. Don’t rely on internet advice. Don’t stop the antibiotic just because you’re scared. Here’s what to do:- Take a photo. Save it. Show it to your doctor.
- Check the timing. Did it start before day 5? That’s more likely to be an allergy.
- Check the look. Are the spots raised and itchy? That’s hives. Flat and not itchy? Probably not an allergy.
- Check for other symptoms. Fever? Swelling? Trouble breathing? Go to the ER.
- Call your doctor. Send them the photo and describe what you see. Don’t wait for an appointment.
Why Mislabeling Antibiotic Allergies Costs Lives
Labeling someone as allergic to penicillin based on a rash they had as a kid can have long-term consequences. People with that label are 69% more likely to get a different, less effective antibiotic. Those alternatives are more expensive, harder on the gut, and increase the risk of drug-resistant infections. The CDC estimates that unnecessary penicillin allergy labels cost the U.S. healthcare system $1.2 billion a year. They also lead to a 30% higher chance of getting a C. difficile infection - a severe, sometimes fatal diarrhea caused by antibiotic overuse. Here’s the good news: 92% of people who think they’re allergic to penicillin test negative when properly evaluated. That means most of those labels are wrong. But they stick. Because no one ever followed up.What Your Doctor Should Do Next
If you’ve had a rash on an antibiotic, your doctor should ask: Was it hives? Did it happen right after the dose? Were you sick with a virus? Did you have a fever or swelling? If the answer is no, they shouldn’t write "penicillin allergy" in your chart. They should write: "Maculopapular rash on day 7 of amoxicillin - non-allergic." Many hospitals now use electronic alerts to flag patients with old allergy labels and prompt doctors to consider testing. A new rapid test called PENtest can confirm or rule out penicillin allergy in just 15 minutes. More clinics are starting to offer it. If you’ve been told you’re allergic to penicillin because of a childhood rash, ask your doctor about getting tested. It’s safe. It’s quick. And it could save you from unnecessary antibiotics down the road.Bottom Line: Don’t Panic. Assess. Act.
A rash on an antibiotic doesn’t mean you’re allergic. Most aren’t. But some are. And some are deadly.- Stop the drug and call 911 if you have hives, swelling, trouble breathing, or a high fever.
- Call your doctor if you have a flat, non-itchy rash after day 5 - don’t stop the antibiotic on your own.
- Don’t label yourself as allergic based on a rash unless it was confirmed by testing.

All Comments
Allison Turner November 26, 2025
Ugh, another post telling us not to panic. Like that helps when your kid looks like a tomato and you’ve been up all night. I stopped the amoxicillin. So what? Better safe than sorry. Doctors don’t even know what they’re talking about half the time.
Also, why is everyone so quick to blame the virus? Maybe it’s the drug. Maybe it’s both. Who cares? I’m not giving my kid another round just because some study says it’s ‘probably fine’.
Darrel Smith November 28, 2025
Let me tell you something, folks. This whole ‘it’s not an allergy’ nonsense is a dangerous myth pushed by Big Pharma and lazy pediatricians who don’t want to deal with the paperwork. My niece got hives on day three, they told her it was ‘just a rash,’ and three days later she was in the ICU with swelling in her throat. That’s not a coincidence. That’s negligence. And now she’s labeled ‘penicillin allergic’ for life because no one had the guts to test her properly. We’re gambling with kids’ lives here, and it’s not even a close game.
Stop normalizing this. Stop trusting ‘studies.’ Stop trusting doctors who haven’t seen a real allergic reaction in ten years. If it looks weird, if it feels wrong - STOP THE DRUG. Then call 911. Then sue the hospital. I’m not joking.
Aishwarya Sivaraj November 29, 2025
as a mom of two and a nurse in delhi i’ve seen this so many times
the rash on day 7 with no fever no itching its almost always the virus not the antibiotic
my son got it on amoxi too we kept going and he was fine
but i also saw a girl in the ward with sjs from amoxicillin after being told it was just a rash
so its not black and white
photo the rash call your doc dont panic but dont ignore either
and if you can get pen test do it
so many people carry wrong labels like its a tattoo
but its just a mistake from years ago
we need more awareness not fear
and please stop blaming parents for stopping meds
they’re scared and no one taught them how to tell the difference
Iives Perl December 1, 2025
They’re hiding the truth. The rash is the immune system fighting the glyphosate in the antibiotic. The virus? A distraction. The CDC? In bed with Big Pharma. EpiPen? A placebo. Trust your gut. 🤔💉
steve stofelano, jr. December 2, 2025
Thank you for this meticulously researched and clinically grounded exposition. The distinction between non-allergic maculopapular eruptions and true IgE-mediated hypersensitivity is not merely academic - it is a matter of public health integrity. The over-labeling of penicillin allergy has profound downstream consequences, including increased antimicrobial resistance and higher rates of Clostridioides difficile infection. I commend the inclusion of the PENtest and the CDC’s updated guidelines, which reflect a paradigm shift toward evidence-based de-labeling. I urge all healthcare institutions to implement formal allergy reassessment protocols and to educate patients on the distinction between adverse reactions and true allergies. This is not just good medicine - it is ethical medicine.
Savakrit Singh December 3, 2025
This is why India needs better primary care. 90% of parents here stop antibiotics at first sign of rash. No testing. No follow-up. Just fear. And then they come back with C. diff or pneumonia because the first bug wasn’t killed. 🤦♂️💉 The government should make PENtest available in every PHC. And stop letting pharmacists give antibiotics without prescriptions. This isn’t just a US problem.
Cecily Bogsprocket December 5, 2025
I remember when my daughter broke out in that flat pink rash on day 6. I panicked. I called the doctor crying. She said, ‘That’s the Epstein-Barr. Not the amoxicillin. Keep going.’
It felt wrong to keep giving it. But I trusted her.
Two days later the spots faded. No fever. No swelling. Just a weird skin thing that looked scary but meant nothing.
Now I tell every mom I know: don’t assume the worst. Don’t stop because you’re scared. Don’t label your kid based on a rash that didn’t itch.
But also - don’t ignore the signs that really matter. Hives? Swelling? Trouble breathing? That’s your signal.
Most rashes are just noise. But you have to learn how to listen for the signal.
It’s not about being brave. It’s about being informed.
And you’re not alone in being scared. You’re just supposed to be smart about it.
Miriam Lohrum December 7, 2025
It’s fascinating how we treat medical knowledge like a mythos - something to be feared or revered, but rarely questioned. We assign moral weight to ‘stopping’ or ‘continuing’ as if it’s a choice between virtue and vice. But medicine isn’t about virtue. It’s about probability, timing, and context. A rash on day 7 is statistically unlikely to be an allergy. That’s not comforting. It’s just data.
And yet, we cling to stories - the one about the kid who got hives, the one about the aunt who died from penicillin, the one about the doctor who missed it.
Those stories are real. But they’re outliers. And outliers shouldn’t dictate policy for millions.
Maybe the real problem isn’t the rash.
It’s our fear of uncertainty.