Prescription Safety: How to Avoid Dangerous Mistakes with Medications
When you take a prescription, a medication legally issued by a licensed provider to treat a specific condition. Also known as controlled drugs, these aren’t just pills—they’re powerful tools that can save your life or seriously harm you if used wrong. Most people assume their doctor or pharmacist has checked everything. But prescription safety isn’t just about following directions—it’s about asking the right questions, spotting hidden risks, and knowing when something doesn’t add up.
Drug interactions, when two or more medications react in ways that change their effect, are one of the biggest hidden dangers. For example, taking PDE5 inhibitors like Viagra with nitrates can drop your blood pressure to deadly levels. Or mixing trimethoprim (in Bactrim) with blood pressure meds can spike your potassium to dangerous levels. These aren’t rare cases—they happen every day because patients aren’t told what to watch for. Even generic drugs, which are often cheaper and just as effective, can carry risks if they’re made in poorly regulated factories. Some clinicians are seeing higher rates of side effects from overseas generics, especially older ones with thin profit margins.
Prescription safety also means knowing when to question a dose change. A simple typo—like 10mg instead of 1mg—can land you in the ER. That’s why tools like barcode scanning and the SBAR method (Situation, Background, Assessment, Recommendation) are used in hospitals: to catch errors before they happen. But you don’t need to be a nurse to protect yourself. Always double-check the label, ask your pharmacist why a new drug was prescribed, and never assume a generic is identical to your old brand if you notice new side effects. The FDA requires bioequivalence studies to prove generics work the same, but real-world results don’t always match the lab.
And then there’s the silent issue: misinformation. Many think an antibiotic rash means they’re allergic—when it’s often harmless. Or they keep using nasal sprays like oxymetazoline for weeks, triggering rebound congestion. Prescription safety isn’t just about avoiding poison—it’s about understanding what’s normal and what’s a warning sign. Fluoroquinolones can tear tendons. Iron pills can block thyroid meds. Energy drinks with Adderall can trigger heart problems. These aren’t conspiracy theories—they’re documented risks backed by FDA warnings and clinical data.
What you’ll find below isn’t a list of warnings—it’s a practical guide to staying safe. From how to time your iron with levothyroxine to why some generics cost 20x more than others, these posts cut through the noise. You’ll learn how to spot bad manufacturing, avoid deadly interactions, and speak up when something feels off. Prescription safety isn’t about fear. It’s about power—knowing enough to protect yourself before the next mistake happens.
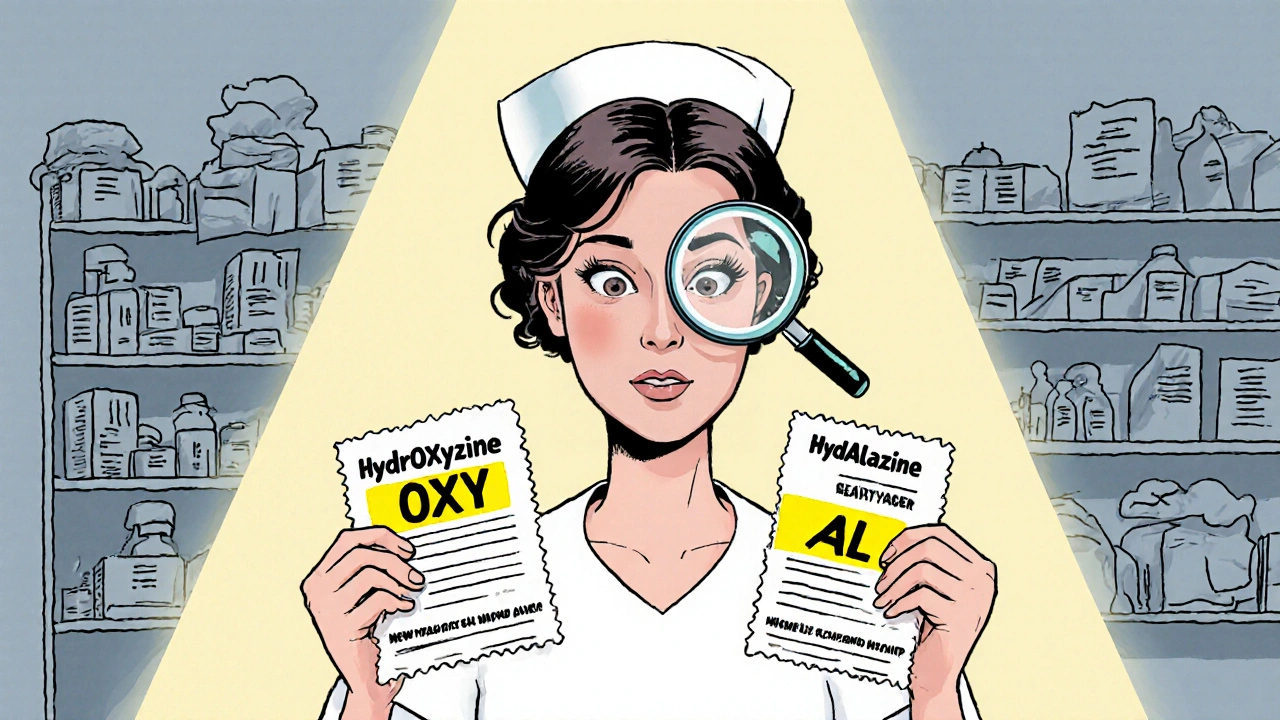
How to Identify Look-Alike Names on Prescription Labels
- Robin Tudge
- November 27, 2025
- 13 Comments
Learn how to spot dangerous look-alike drug names on prescription labels using tall man lettering, barcode scanning, and verification steps. Reduce medication errors with proven strategies used in U.S. hospitals.
read more