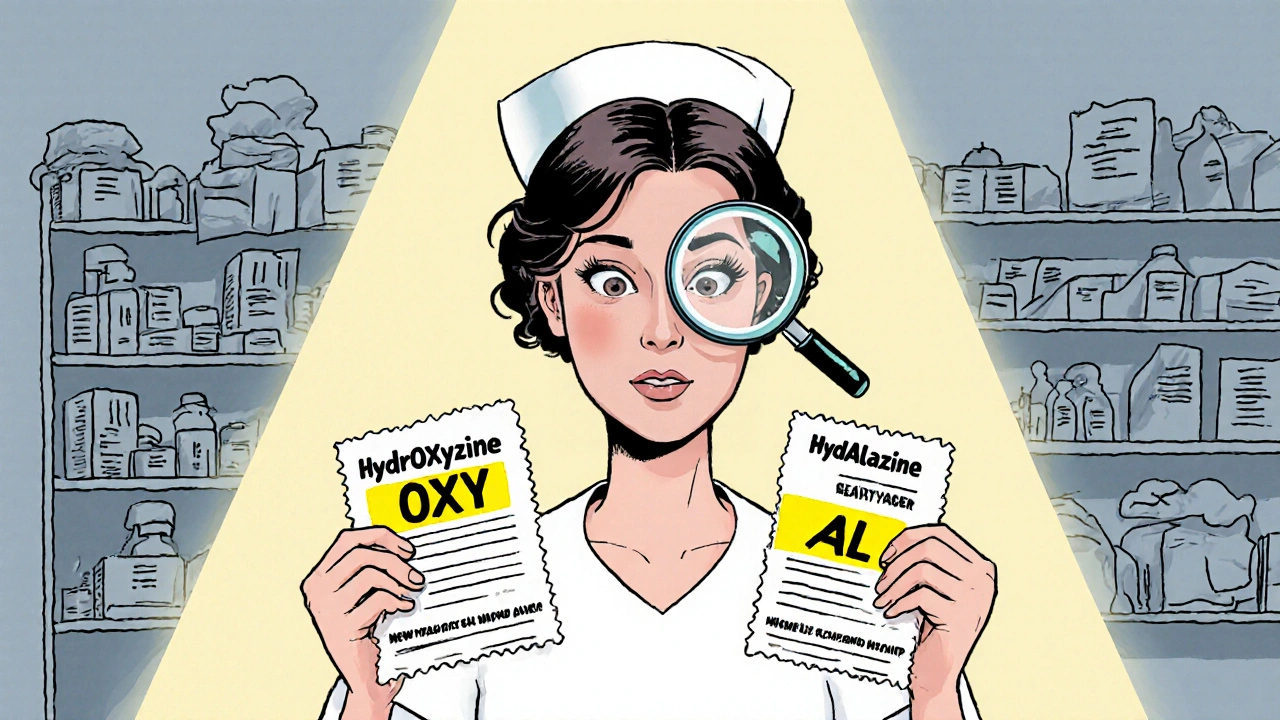
Every year, thousands of patients in the U.S. receive the wrong medication-not because of a mistake in dosage, but because two drug names look or sound almost identical. Look-alike and sound-alike (LASA) drug names are one of the most common causes of preventable medication errors. A single mix-up between hydroCODONE and hydroHYDRAZINE can lead to overdose, organ damage, or even death. The good news? There are clear, proven ways to spot these dangerous similarities before they cause harm.
What Makes Drug Names Look or Sound Alike?
Not all similar drug names are dangerous. But when two names share 60-80% of the same letters or syllables, the risk spikes. For example:- HydrOXYzine vs. HydrALazine
- DoXEpamine vs. DoBUTamine
- CISplatin vs. CARBOplatin
- Valtrex (valACYclovir) vs. Valcyte (valGANciclovir)
Tall Man Lettering: The Standard Visual Fix
The most widely used tool to fight LASA errors is tall man lettering (TML). This isn’t just capitalizing random letters-it’s a precise system. The FDA and ISMP recommend capitalizing the parts of the name that differ, making the distinction instantly visible.For example:
- HydrOXYzine
- HydrALazine
The capitalization draws the eye to the critical difference: “OXY” vs. “AL.” Studies show TML reduces visual confusion by 32%. But it only works if it’s applied consistently.
The FDA officially recommends TML for 35 high-risk drug pairs as of 2024, up from 23 in 2023. These include insulin brands like Humalog and Humulin, anticoagulants like Lovenox and Heparin, and sedatives like Ativan and Avinza. Every pharmacy label, EHR system, and automated dispensing cabinet should display these names in TML format.
Why TML Alone Isn’t Enough
Many hospitals think installing TML solves the problem. It doesn’t. A 2022 study in the Journal of Patient Safety found that TML alone cuts errors by only 32%. But when you add color coding, the jump is to 47%. Add the purpose of the medication-like “for anxiety” or “for blood pressure”-and effectiveness rises to 59%.Here’s why: TML helps you see the difference. But if you’re tired, distracted, or under time pressure, your brain still skips over details. That’s why the best systems combine three layers:
- Visual - Tall man lettering
- Color - Highlighting high-risk pairs in yellow or red
- Context - Adding the reason the drug is prescribed
At Johns Hopkins Hospital, combining all three cut LASA errors by 67% over two years. That’s not luck-it’s design.
How Electronic Systems Can Help (and Hurt)
Your EHR system is supposed to protect you-but it can also cause confusion. Many systems still list similar drug names right next to each other in dropdown menus. If you’re typing “Hyd” and see “Hydroxyzine” and “Hydralazine” side by side, your finger might pick the wrong one.The Office of the National Coordinator for Health IT requires EHRs to prevent this. Confusing pairs must be separated by at least one other drug. That simple rule reduces selection errors by 41%.
Another rule: require at least five letters before showing drug options. This cuts down clutter and forces you to type more precisely. One hospital saw a 68% drop in error-prone dropdown lists after making this change.
But here’s the catch: alerts can backfire. Computer warnings for LASA pairs pop up constantly. Clinicians start ignoring them. A 2021 JAMA study found that 49% of LASA alerts are overridden-often because they’re too broad or appear for low-risk drugs. The fix? Only trigger alerts for the FDA’s official high-risk pairs. Done right, override rates drop from 73% to 31%.

What You Can Do: A 3-Step Verification Process
No matter how good the system is, humans still handle the drugs. That’s why the FDA and ISMP recommend a simple three-step check every time you handle a high-risk medication:- Read the full label before picking it up. Don’t just glance at the first few letters.
- Confirm with another person before handing it off. A second set of eyes catches 80% of mistakes.
- Read it again when giving it to the patient or placing it in the unit.
This process reduces errors by 52%. It takes less than 30 seconds. But in a busy clinic, it’s often skipped.
Handwritten Prescriptions Are Still a Big Problem
Even with all the tech, handwritten orders remain a major risk. A Reddit thread from 2023 with 87 pharmacy professionals found that 41% of LASA errors still came from poor handwriting. “I’ve seen ‘Hydroxyzine’ scribbled as ‘Hydralazine’ so badly that even the pharmacist couldn’t tell,” one user wrote.And if the label is printed on a low-quality printer? The tall man letters might blur together. The Joint Commission requires a minimum 12-point font and 4.5:1 color contrast on labels. If the print looks faded or smudged, don’t use it. Ask for a new one.
Barcode Scanning: The Gold Standard
The most effective way to prevent LASA errors? Barcode scanning. When you scan the patient’s wristband and the medication at the same time, the system checks for matches. If the drug doesn’t match the order, it won’t let you proceed.Barcode scanning reduces administration errors by 81%. But it’s expensive-about $153,000 per hospital to install. Still, hospitals that use it report 53% fewer LASA-related adverse events than those that don’t.
For smaller clinics, you don’t need the full system. Even a handheld scanner at the point of dispensing cuts errors by 86%. The key is using it at four critical points:
- Stocking meds in the pharmacy
- Dispensing to the nurse
- Refilling automated cabinets
- Before giving the drug to the patient
What’s Changing in 2025?
The FDA is expanding its list of TML-recommended drug names. By the end of 2024, all U.S. healthcare systems must use TML for the full 35 pairs. In 2025, the National Council for Prescription Drug Programs will roll out a new data standard that lets EHRs, pharmacies, and insurers share real-time LASA alerts.Artificial intelligence is stepping in too. Google Health’s Med-PaLM 2 can predict LASA confusion with 89% accuracy. But it’s not replacing humans-it’s helping them. AI flags potential issues during prescribing, so doctors can choose a less confusing name before it’s ever written.
Final Checklist: Spotting LASA Names Before It’s Too Late
Use this quick guide every time you handle a prescription:- Is the drug name on the FDA’s TML list? (Check ISMP or FDA websites)
- Are the different letters capitalized? (e.g., HydrOXYzine)
- Is the reason for use written on the label? (e.g., “for seizures”)
- Is the font at least 12-point and clearly printed?
- Did I read the full name aloud before giving it?
- Did I double-check with a colleague?
- Did I scan the barcode if available?
These aren’t extra steps. They’re safety nets. One extra second of checking can prevent a lifetime of regret.
What are the most common look-alike drug name pairs I should watch out for?
The FDA’s top 10 high-risk pairs include: HydrOXYzine vs. HydrALazine, DoXEPamine vs. DoBUTamine, CISplatin vs. CARBOplatin, Valtrex (valACYclovir) vs. Valcyte (valGANciclovir), Humalog vs. Humulin, Lovenox vs. Heparin, Ativan vs. Avinza, Clonidine vs. Clonazepam, Prednisone vs. Prednisolone, and Levothyroxine vs. Liothyronine. Always verify these names using tall man lettering and confirm the purpose of use.
Does tall man lettering work for non-English speakers?
Tall man lettering was designed for English, and its effectiveness drops to about 62% in Spanish-speaking settings because phonetic similarities change. For example, “Hydroxyzine” and “Hydralazine” sound more alike in Spanish than in English. In multilingual environments, adding the purpose of use (“for allergies” vs. “for high blood pressure”) becomes even more critical than capitalization alone.
Can I rely on electronic alerts to catch all LASA errors?
No. Clinicians override nearly half of all LASA alerts because they’re too frequent or poorly targeted. Alerts should only trigger for the FDA’s official high-risk pairs. Even then, they’re a backup-not a replacement-for human verification. Always read the label yourself, even if the system says it’s safe.
Why do some pharmacies still use non-TML labels?
Some older systems, handwritten orders, or low-cost label printers don’t support tall man lettering. Also, some generic manufacturers skip TML because it’s not always legally required for off-label or compounded drugs. If you see a label without TML for a high-risk drug, treat it as suspect. Verify with the prescriber or pharmacist before giving it.
Is there a list I can print and keep at my station?
Yes. The Institute for Safe Medication Practices (ISMP) publishes a free, downloadable list of all FDA-recommended tall man lettering pairs. You can also find color-coded versions from the FDA’s Division of Medication Error Prevention. Print it, laminate it, and hang it near your dispensing area. Review it monthly-it’s one of the simplest ways to stay alert.
What to Do Next
If you’re a clinician: Start using the 3-step verification process today. Even if your system doesn’t force it, make it a habit. One extra check can save a life.If you’re a pharmacy manager: Audit your labels. Are all high-risk drugs using TML? Are barcode scanners working at every critical point? If not, prioritize fixing those gaps.
If you’re a patient: Always ask, “What is this medicine for?” If the label doesn’t say, ask again. Don’t assume the name is correct. You’re your own best safety net.
Medication safety isn’t about perfection. It’s about layers. TML, scanning, alerts, and human checks-each one catches what the others miss. When they all work together, errors drop. When even one fails, the risk rises. Don’t wait for a system to fix itself. Be the one who checks.

All Comments
king tekken 6 November 28, 2025
yo i just saw a script that said 'Hydroxyzine' but the bottle was 'Hydralazine' and i thought my eyes were glitchin' 😅 turns out i'm not the only one. TML is a lifesaver but honestly? i still mix em up sometimes. we need like, voice alerts or somethin'.
DIVYA YADAV November 28, 2025
This is just another way the American pharmaceutical industry controls us. Why do we even have these confusing names? It's deliberate. They want us to make mistakes so they can sell more drugs. In India, we don't have this mess. Our doctors write clearly and patients know what they're taking. This is capitalism poisoning healthcare.
Kim Clapper November 30, 2025
I must say, while I appreciate the thoroughness of this piece, I find it deeply concerning that the FDA has only mandated tall man lettering for 35 pairs. That is a woefully inadequate number. The entire system is a facade of safety. The real issue? The unchecked power of Big Pharma lobbying. If you look at the FDA's funding sources, you'll see the same corporations that profit from these naming ambiguities are the ones shaping policy. This is not an error-it's engineered negligence.
Bruce Hennen November 30, 2025
Tall man lettering is not a solution-it's a band-aid. The real problem is the lack of standardized nomenclature in pharmacology. The FDA should have mandated unique, non-ambiguous naming conventions from day one. The fact that we're still capitalizing random letters in 2024 is a systemic failure of linguistic governance. Also, 'DoXEPamine' is misspelled. It's Doxepin. Fix your facts before preaching safety.
Jake Ruhl December 1, 2025
Okay but let’s be real-this whole thing is a scam. I work in a clinic and the barcode scanners don’t even work half the time. And the alerts? They beep like a broken microwave. Everyone just clicks 'ignore'. And don’t get me started on the nurses who don’t read labels because they’re on their 12th shift this week. This isn’t about lettering. It’s about burnout. We’re drowning and they’re giving us flashcards. The system is broken. Someone needs to burn it down and start over.
Chuckie Parker December 1, 2025
Barcode scanning works. End of story. If your hospital doesn't have it you're not trying. I've seen pharmacies skip scanning because it 'takes too long'. Bullshit. It takes 3 seconds. 3 seconds to not kill someone. Stop making excuses. The data is clear. No scanning = higher death rate. Period.
George Hook December 2, 2025
I've been a pharmacist for 27 years. I've seen the evolution from handwritten scripts to EHRs. What hasn't changed is the human element. No system replaces double-checking. I still read every label aloud-even if I've given the same drug a hundred times. That one extra second? It's the difference between going home and going to court. I wish every new tech was paired with a mandatory 10-minute safety huddle. Simple. Effective. Human.
jaya sreeraagam December 4, 2025
This is so important! I work in a rural clinic in India and we don't always have TML labels, but we do have community health workers who double-check every prescription with the patient. We say the name, we say the reason, we even ask the patient to repeat it back. It’s not fancy tech, but it works. And when patients feel heard, they speak up if something feels off. That’s the real safety net. Keep sharing these stories-they matter.
Katrina Sofiya December 6, 2025
Thank you for writing this with such clarity and compassion. As a nurse, I’ve seen the quiet panic in a patient’s eyes when they realize they’ve been given the wrong pill. This isn’t just about protocols-it’s about dignity. I’ve started laminating the ISMP list and posting it above my med cart. I also say the drug name, the dose, and the reason out loud every single time. It feels awkward at first, but now my team does it too. Small habits save lives.
kaushik dutta December 7, 2025
In the Indian context, we face a dual challenge: linguistic diversity and infrastructural gaps. While TML helps in English-speaking environments, many patients and providers operate in Hindi, Tamil, or Bengali where phonetic similarity shifts entirely. The real innovation isn't in capitalization-it's in multilingual, context-aware EHRs that auto-translate drug indications. AI can bridge this. But only if we prioritize accessibility over cost-cutting. This isn't just a medical issue-it's a linguistic justice issue.
doug schlenker December 8, 2025
I really appreciate how this breaks it down. I used to think TML was just a nice-to-have. Then my cousin got the wrong drug because the label was smudged and the font was tiny. She ended up in the ER. Since then, I've started checking every label like it's my own. I read it out loud. I ask the pharmacist to confirm. I look for the purpose on the label. It’s not about being paranoid-it’s about being present. We all have the power to stop this.
Olivia Gracelynn Starsmith December 8, 2025
The 3-step check is gold. I do it every time. Read it. Confirm it. Read it again. I don’t care if I’m rushed. I don’t care if the system says it’s fine. I’ve seen too many near-misses. And if the label is printed on a cheap printer? I don’t use it. I go back and ask for a new one. It’s not extra work. It’s part of the job. And if you’re a patient? Ask what it’s for. Always.
Skye Hamilton December 9, 2025
I hate how this stuff gets normalized. Like it’s just part of the chaos. But it’s not. It’s negligence dressed up as 'efficiency'. I saw a nurse hand a patient a vial labeled 'HydrALazine' and the script said 'HydrOXYzine'. She didn’t even blink. I asked her if she’d read it. She said 'I’ve done this a thousand times.' That’s the exact moment someone dies. And we’re all just waiting for it to be us.