Penicillin Allergy: What It Is, How It Shows Up, and What to Do
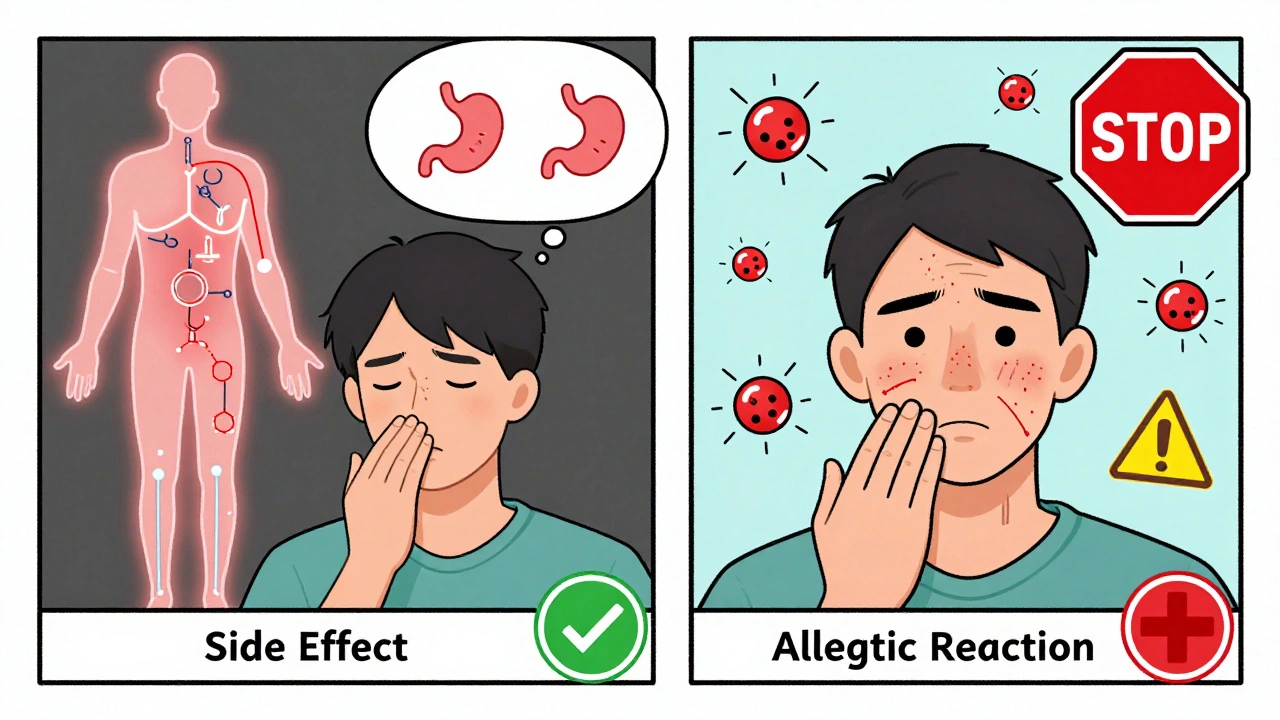
When someone says they have a penicillin allergy, a potentially life-threatening immune response to penicillin-based antibiotics. Also known as beta-lactam allergy, it’s one of the most commonly reported drug allergies in the U.S. But here’s the catch: up to 90% of people who think they’re allergic to penicillin aren’t. Many outgrew it. Others had a rash from a virus, not the drug. Or they confused side effects like nausea or diarrhea with an allergic reaction.
A true penicillin allergy, an immune system overreaction triggered by penicillin or related antibiotics like amoxicillin. Also known as hypersensitivity reaction, it can cause hives, swelling, trouble breathing, or anaphylaxis. These reactions usually show up within an hour of taking the drug. But not all rashes are emergencies. A delayed, non-itchy rash—common with amoxicillin in kids with mono—is often just a side effect, not an allergy. Mistaking it for one can lead doctors to prescribe stronger, costlier, or riskier antibiotics like vancomycin or fluoroquinolones, which carry their own dangers like tendon rupture or nerve damage.
That’s why antibiotic allergy, a broader category that includes reactions to any drug in the antibiotic family. Also known as drug hypersensitivity, it’s a key concern in safe prescribing. If you’ve been labeled allergic to penicillin, you might be avoiding the safest, cheapest, and most effective treatment for infections like strep throat, pneumonia, or ear infections. Testing—through skin tests or graded challenges—can clear up confusion and open up better options.
And it’s not just about penicillin. If you’re truly allergic, you might also react to cephalosporins or carbapenems, though cross-reactivity is lower than most think. Knowing your real risk helps avoid unnecessary drug switches and reduces the chance of side effects from alternatives. For example, trimethoprim can raise potassium levels dangerously in older adults, and fluoroquinolones can cause permanent nerve damage. Avoiding penicillin without good reason might put you at higher risk than staying on it.
Below, you’ll find real-world advice from patients and clinicians on how to recognize true reactions, what to do if you think you’re allergic, and how to safely test or rechallenge your history. You’ll also see how common misdiagnoses affect treatment choices—and why asking the right questions can save you money, time, and health risks.
Penicillin Desensitization: Safe Protocols for Patients with Penicillin Allergy
- Robin Tudge
- December 15, 2025
- 11 Comments
Penicillin desensitization safely allows allergic patients to receive life-saving penicillin therapy when no alternatives exist. Learn how it works, who qualifies, and why it's critical for fighting antibiotic resistance.
read moreDifference Between Medication Side Effects and Allergic Drug Reactions
- Robin Tudge
- December 3, 2025
- 8 Comments
Learn the key differences between medication side effects and true allergic drug reactions. Discover why mislabeling side effects as allergies leads to unnecessary risks, higher costs, and worse health outcomes.
read more