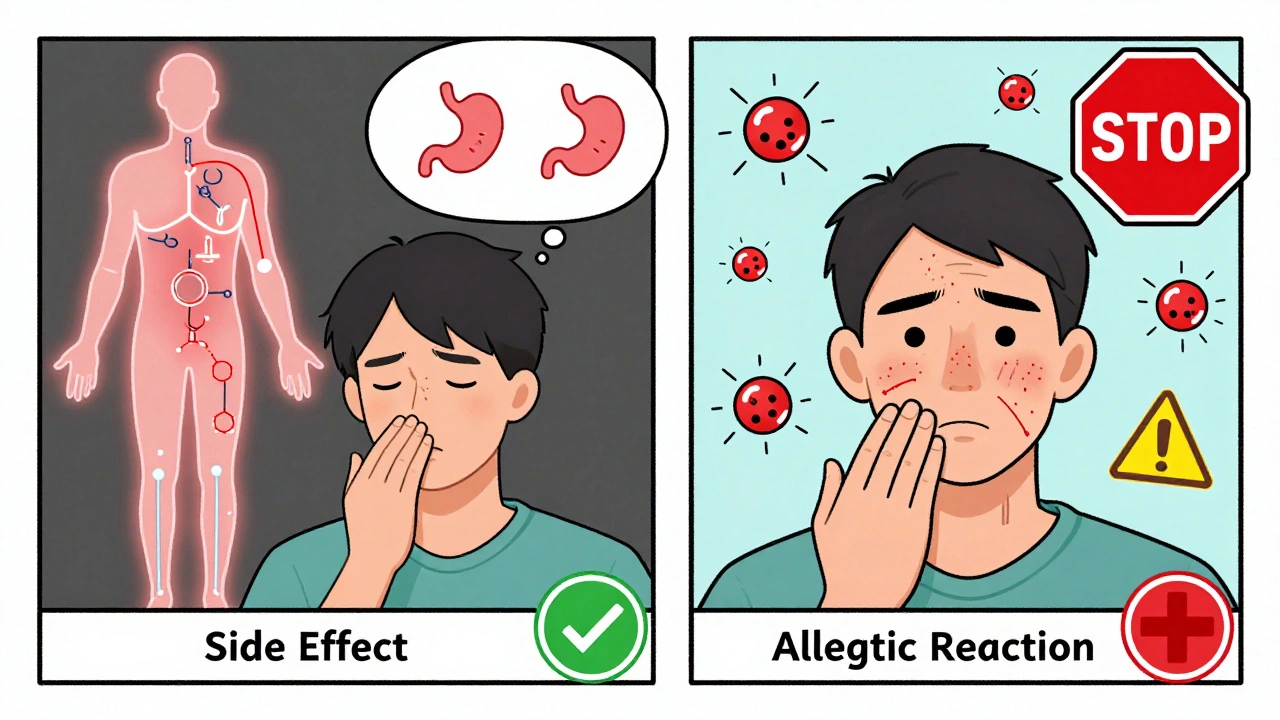
Many people think if a drug makes them feel sick, they’re allergic to it. But that’s not always true. In fact, most people who say they’re allergic to antibiotics like penicillin aren’t allergic at all. They’re just experiencing a side effect. Understanding the difference isn’t just about terminology-it can change your treatment options, lower your risk of antibiotic resistance, and even save money. Let’s break down exactly how these two reactions are different, why it matters, and what to do if you’re unsure.
What Are Medication Side Effects?
Side effects are predictable, non-allergic reactions that happen because of how a drug works in your body. They’re listed in the drug’s official labeling, often with percentages showing how common they are. For example, statins-medications used to lower cholesterol-cause muscle aches in about 5% to 10% of users. Metformin, a common diabetes drug, leads to stomach upset in 20% to 30% of people who take it. These aren’t random. They’re tied directly to the drug’s chemical action.Side effects usually show up within hours or days of starting the medication. They often get better over time as your body adjusts. About 70% to 80% of common side effects fade within two to four weeks. You can often manage them without stopping the drug. Taking metformin with food cuts GI issues in 60% of cases. Drinking plenty of water helps with some blood pressure meds. Your doctor might lower the dose or add another medication to offset the problem.
These reactions don’t involve your immune system. They’re just the drug doing something it wasn’t meant to do-like irritating your stomach lining or affecting muscle cells. That’s why you can sometimes tolerate the same drug again later, even if you had a side effect before.
What Is a True Allergic Drug Reaction?
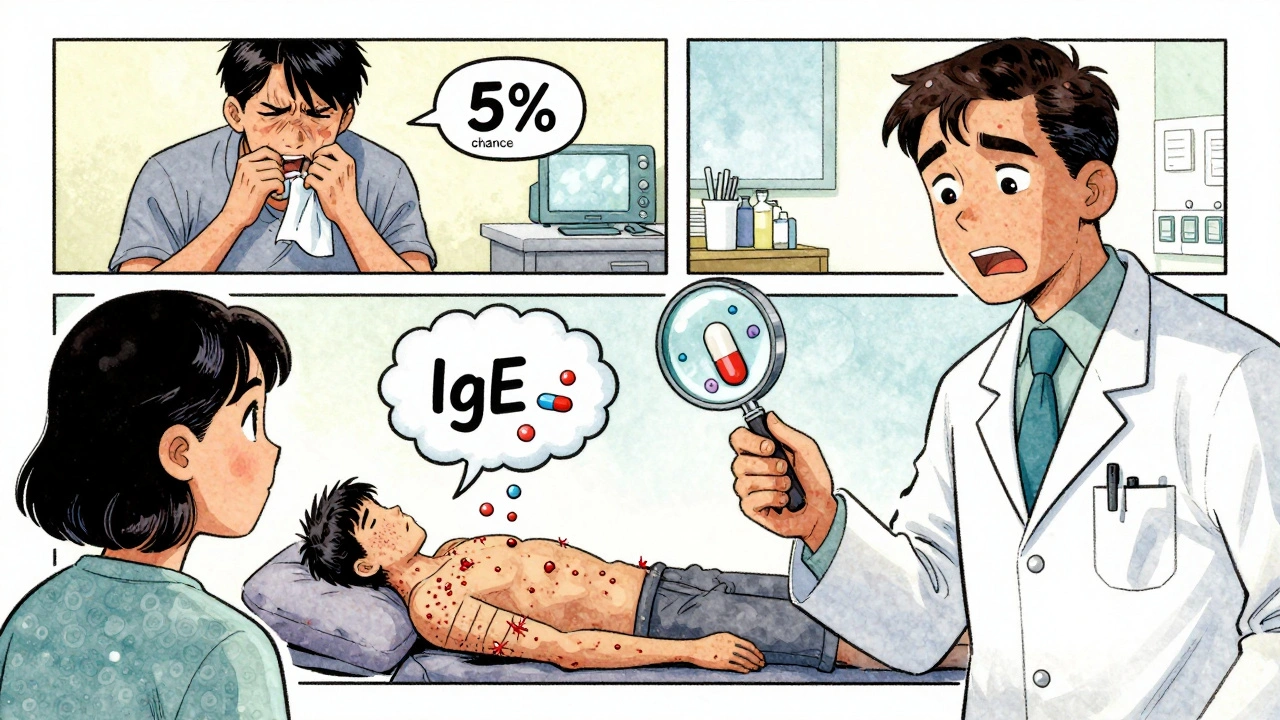
A true drug allergy is your immune system reacting like the drug is an invader-like a virus or pollen. It’s not just feeling bad. It’s your body launching an attack. This happens because your immune system mistakenly identifies the drug as dangerous and creates antibodies against it.There are two main types of allergic reactions: immediate and delayed. Immediate reactions, mediated by IgE antibodies, kick in within minutes to two hours. Symptoms include hives, swelling of the face or throat, wheezing, and in severe cases, anaphylaxis-a life-threatening drop in blood pressure and airway swelling. According to the European Academy of Allergy and Clinical Immunology, anaphylaxis from drugs affects 0.05% to 0.5% of exposures, with a death rate of 0.3% to 1% even with treatment.
Delayed reactions take longer. They often show up as rashes, sometimes days or even weeks after taking the drug. Maculopapular rashes-the most common type-appear in 90% of delayed cases within one to two weeks. These can be mistaken for viral infections, but they’re immune-driven.
Drugs most likely to cause true allergies include penicillin (responsible for 80% of severe drug allergies), sulfa drugs, and certain NSAIDs like ibuprofen or naproxen. Unlike side effects, allergic reactions usually happen at normal, prescribed doses. You don’t need to take a lot to trigger them. And once your immune system remembers the drug, it can react every time-even years later.
How to Tell the Difference
Here’s a quick way to tell them apart:- Timing: Side effects start within hours and often improve over days. Allergic reactions can be immediate (minutes) or delayed (days to weeks).
- Symptoms: Side effects = nausea, dizziness, dry mouth, headache. Allergic reactions = hives, swelling, trouble breathing, anaphylaxis, blistering rashes.
- Immune system: Side effects? No immune involvement. Allergy? Yes-confirmed by skin tests or blood tests measuring IgE.
- Dose dependency: Side effects often get worse with higher doses. Allergies happen at any dose-even a tiny amount.
- Reoccurrence: You might tolerate a side effect after a few days. An allergy? You’ll likely react again, every time.
One of the biggest red flags? Gastrointestinal symptoms. Diarrhea, nausea, or stomach cramps after taking antibiotics are almost never allergies. They’re side effects. Yet, 78% of Reddit users who report “penicillin allergy” say it’s because of diarrhea or vomiting. That’s not an allergy. That’s your gut reacting to the drug changing your bacteria balance.
Why Mislabeling an Allergy Is Dangerous
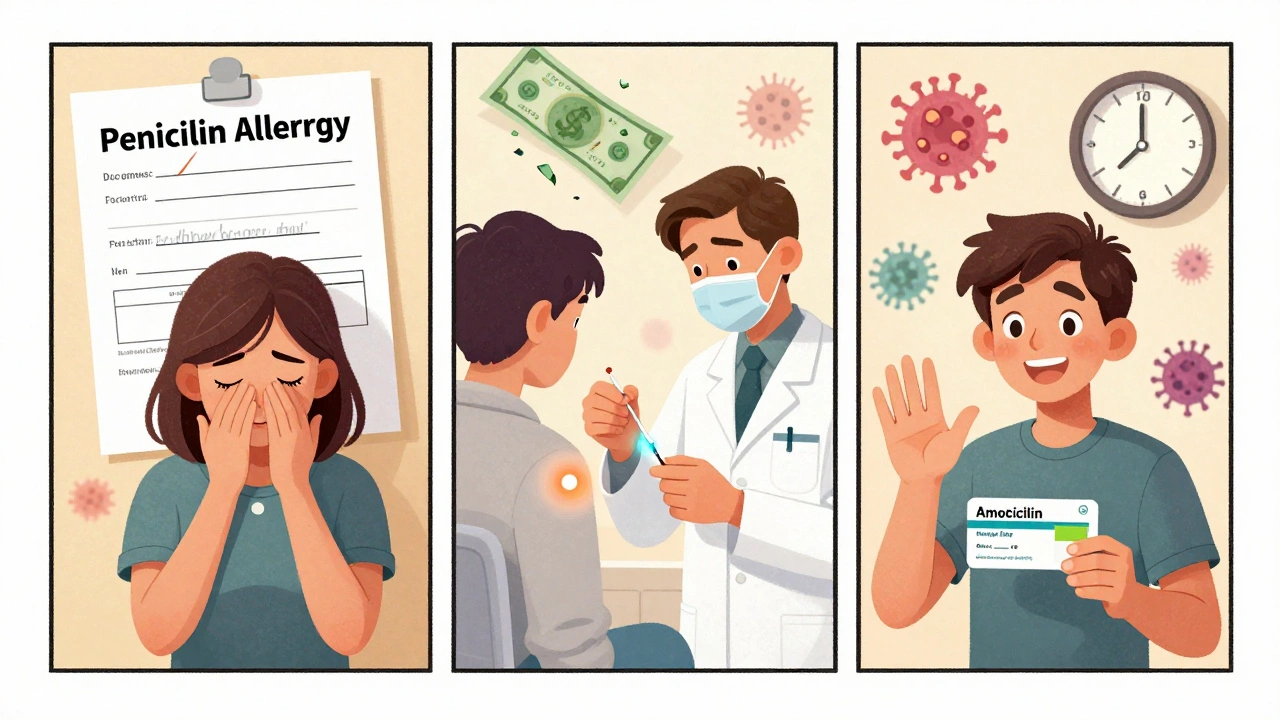
If you say you’re allergic to penicillin when you’re not, your doctor will avoid it. That sounds safe-but it’s not. Penicillin and related drugs like amoxicillin are among the safest, most effective antibiotics. When they’re ruled out, doctors turn to broader-spectrum alternatives like vancomycin or fluoroquinolones. These drugs are more expensive, more likely to cause side effects, and more likely to lead to antibiotic-resistant infections like MRSA.A 2021 study in JAMA Internal Medicine found that 80% to 90% of people who think they’re allergic to penicillin aren’t. When tested, most clear the label. But the damage is already done. Each mislabeled allergy increases annual healthcare costs by about $4,000 per patient. It also raises the risk of MRSA infection by 69%, according to Dr. Elina Jerschow of the American College of Allergy, Asthma & Immunology.
And it’s not just penicillin. About 30% to 40% of hospitalized patients have a documented drug allergy. But when allergists evaluate them, 90% to 95% turn out not to have a true allergy. That’s a massive gap between what’s recorded and what’s real.
What to Do If You Think You Have a Drug Allergy
If you’ve had a reaction, don’t just assume it’s an allergy. Talk to your doctor. Ask: Was this a side effect or an allergic reaction? If the reaction was mild-like a rash or upset stomach-it might not be an allergy. But if you had swelling, trouble breathing, or passed out, you need to see an allergist.For penicillin, the standard evaluation is a three-step process:
- History review: Your doctor will ask exactly what happened, when, and how long it lasted. About 60% of people can be cleared just by answering these questions.
- Skin test: A small amount of the drug is placed under your skin. If there’s no reaction after 15-20 minutes, it’s very unlikely you’re allergic (97% negative predictive value).
- Oral challenge: If the skin test is negative, you’ll be given a small dose under supervision. Less than 0.2% of low-risk patients react. If you tolerate it, you’re cleared.
This process is safe, quick, and widely available in hospitals and allergy clinics. Yet, only 10% of U.S. allergists have the capacity to do these tests regularly. That’s why primary care doctors are being trained to recognize the signs and refer appropriately.
What’s New in Drug Allergy Testing
In 2023, the FDA approved a new blood test called the basophil activation test (BAT) for penicillin allergy. It’s more accurate than skin testing alone, with 85% sensitivity and 95% specificity. It’s especially helpful for people who can’t stop taking antihistamines or have skin conditions that make skin tests hard.Another big advance is pharmacogenomics. For example, the drug abacavir, used for HIV, can cause a severe allergic reaction in people with the HLA-B*57:01 gene. Before testing, 8% of patients reacted. Now, doctors screen for the gene first. The reaction rate has dropped to 0.4%. That’s a game-changer.
How to Get It Right
If you’ve been told you have a drug allergy:- Don’t just accept it. Ask for a referral to an allergist.
- Write down exactly what happened: symptoms, timing, dose, how long it lasted.
- Bring your full medication list to your appointment.
- Don’t avoid a drug unless you’ve been tested. You might be missing out on the safest, most effective option.
And if you’re a patient who’s had side effects, don’t panic. Most aren’t allergies. Talk to your doctor about managing them. You might not need to stop the drug at all.
Final Takeaway
Side effects are common, often manageable, and don’t mean you’re allergic. Allergic reactions are rare, immune-driven, and dangerous. Confusing the two leads to unnecessary restrictions, higher costs, and worse health outcomes. If you’ve ever said, “I’m allergic to this drug,” ask yourself: Did I have hives or swelling? Or did I just feel nauseous? The answer could change your future care.Can you outgrow a drug allergy?
Yes, many people outgrow drug allergies, especially penicillin. Studies show that up to 80% of people who had a true penicillin allergy in childhood lose their sensitivity after 10 years. That’s why retesting later in life is important-especially if you need the drug for an infection. Never assume you’re still allergic just because you were once.
Is a rash always a sign of a drug allergy?
No. Many rashes from medications are not allergic. Viral infections, heat, or even non-allergic inflammation can cause rashes that appear right after starting a drug. True allergic rashes often itch, spread, and last longer than 24 hours. Non-allergic rashes may be flat, not itchy, and fade quickly. Only a doctor can tell the difference-so don’t self-diagnose.
Can you be allergic to a drug you’ve taken before without problems?
Yes. Allergic reactions can develop after multiple exposures. Your immune system doesn’t always react the first time. It might take two, three, or even ten doses before it recognizes the drug as a threat. That’s why you can suddenly have an allergic reaction to a medication you’ve taken safely for years.
If I’m allergic to penicillin, am I allergic to all antibiotics?
No. Penicillin allergies don’t automatically mean you’re allergic to all antibiotics. Only certain classes, like cephalosporins, have some cross-reactivity-about 10% for older types, less than 2% for newer ones. Many people labeled penicillin-allergic can safely take other antibiotics like azithromycin, doxycycline, or clindamycin. Testing clears up these misconceptions.
Should I carry an epinephrine auto-injector if I think I’m allergic to a drug?
Only if you’ve had a confirmed anaphylactic reaction. If your reaction was mild-like a rash or stomach upset-you don’t need one. Carrying an auto-injector unnecessarily can lead to anxiety and false alarms. If you’re unsure, see an allergist. They’ll determine if you’re at real risk and whether you need emergency medication.
If you’ve ever avoided a medication because you thought you were allergic, consider getting tested. You might be surprised-and your future self will thank you.

All Comments
Krys Freeman December 5, 2025
Stop lying to yourself. If you puked after taking penicillin, you’re allergic. Period. No ‘side effect’ BS.
Lyn James December 6, 2025
It’s not just medical ignorance-it’s a systemic failure of trust. We’ve been conditioned to accept pharmaceutical narratives without question. The immune system doesn’t lie. If your body recoils, it’s not ‘just’ nausea-it’s a sacred warning. We’ve turned medicine into a commodity and spirituality into a side effect. The real allergy? To truth.
When you reduce human experience to percentages and clinical trials, you erase the soul’s voice. That rash? Maybe it’s your soul rejecting the chemical invasion. You think doctors know better? They’re paid by the same corporations that profit from misdiagnoses. The truth is buried under layers of profit-driven orthodoxy.
And yet, we still bow at the altar of ‘evidence.’ Evidence based on what? Trials funded by Big Pharma? Studies that exclude the very people who react violently? We’ve normalized oppression as ‘science.’
Don’t be fooled by the jargon. A ‘non-allergic side effect’ is just the system’s way of gaslighting you into compliance. Your body knows. It always knows. You just need to stop listening to the white coats and start listening to your own trembling hands.
They’ll tell you to get tested. But what if the test is designed to confirm their narrative, not yours? What if the ‘negative result’ is just another form of control?
I’ve seen people die because they were told their anaphylaxis was ‘just anxiety.’ Don’t let them do that to you. Trust your body. Even if the data says otherwise.
They want you to believe you’re wrong. But sometimes, the outlier is the one who’s right.
And if you’re still skeptical? Ask yourself: Who benefits if you keep taking the drug?
Not you.
Craig Ballantyne December 7, 2025
There's a significant clinical distinction here, but the public discourse is dangerously oversimplified. Side effects are pharmacodynamic; allergic reactions are immunologic. The key is the involvement of IgE-mediated pathways, which are quantifiable and reproducible. The 80–90% false-positive penicillin allergy rate is well-documented in peer-reviewed literature-JAMA, NEJM, Annals of Allergy all corroborate this.
Yet, primary care providers rarely refer for formal evaluation. The infrastructure for allergen skin testing and basophil activation assays remains under-resourced. This isn’t a patient education issue-it’s a healthcare system failure.
Moreover, the economic burden is underappreciated. Broad-spectrum antibiotics aren’t just costlier-they’re ecological disruptors. Each unnecessary fluoroquinolone prescription accelerates resistance. We’re not just mislabeling patients-we’re engineering a post-antibiotic future.
Testing protocols are safe, standardized, and accessible in academic centers. The barrier isn’t medical-it’s administrative. Until reimbursement models change, this gap will persist.
Patients need to be empowered, not just informed.
Robert Altmannshofer December 8, 2025
bro i took amoxicillin once and got the worst headache of my life 😵💫 thought i was allergic for 5 years then found out it was just dehydration + caffeine withdrawal lol
now i take it like candy 🍬
Victor T. Johnson December 9, 2025
you people are so weak you think your body is a temple but it’s just a machine that breaks down when you feed it poison
if you got diarrhea from antibiotics you’re not allergic you’re just a walking gut microbiome disaster zone
stop being dramatic and take the damn pill
penicillin is the most tested drug on earth and you’re scared of it because you watched a medical drama on netflix
your fear is killing people more than the drug ever could
get tested or shut up
Bethany Hosier December 10, 2025
While I appreciate the clinical breakdown, I must raise a concern: the very institutions promoting these ‘safe’ re-challenges are the same ones that concealed adverse event data for decades. I’ve reviewed the FDA’s MAUDE database-there are thousands of unreported anaphylactic events tied to ‘low-risk’ penicillin challenges. Are we sure the ‘97% negative predictive value’ isn’t skewed by underreporting?
And what of the patients who develop delayed reactions post-challenge? The FDA’s own 2023 safety bulletin noted a 0.8% incidence of late-onset rashes following oral challenges in previously ‘negative’ patients.
I’m not dismissing science-I’m demanding transparency. If we’re going to re-label people, we must have fully disclosed, long-term follow-up data. Not just ‘you’re fine’ after 20 minutes in a clinic.
My mother died from a delayed reaction to a ‘cleared’ penicillin challenge. She was told it was ‘impossible.’
Let’s not turn patient safety into a statistical gamble.
Kathleen Koopman December 11, 2025
so if i got a rash after sulfa and it went away in 3 days… is that allergic or side effect?? 🤔
also can i get tested even if i’m not currently sick?? 😅
Robert Altmannshofer December 12, 2025
@Kathleen Koopman you can totally get tested even if you’re not sick 😊 the skin test is just a tiny prick, like a mosquito bite but less cute
and if the rash faded fast and didn’t itch like crazy or swell your face? probably not allergic. more like your body was like ‘hey, weird chemical, thanks but no thanks’
but if you’re unsure? go get checked. your future self will hug you