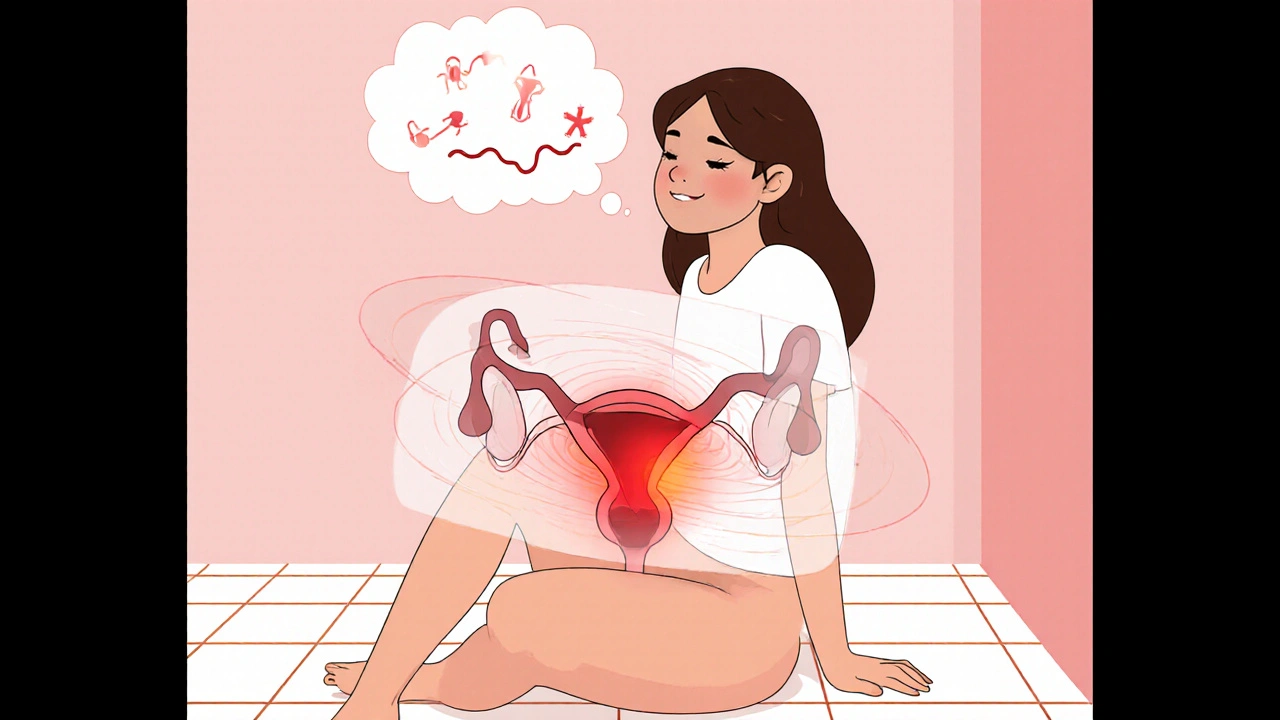
Menstrual Cystitis: What It Is and Why It Happens
When dealing with Menstrual Cystitis, a bladder inflammation that coincides with the menstrual cycle, often causing painful urination and pelvic discomfort. Also known as period‑related bladder infection, it menstrual cystitis is a specific form of Cystitis, general bladder inflammation usually triggered by bacterial invasion that becomes more likely during certain phases of the Hormonal Cycle, the monthly pattern of estrogen and progesterone fluctuations. The hormonal surge can alter the urinary tract’s protective lining, making it easier for a Urinary Tract Infection, infection of the kidneys, ureters, bladder, or urethra to take hold. In short, Menstrual Cystitis encompasses bladder inflammation triggered by hormonal changes, Hormonal Cycle influences urinary tract infection risk, and Effective treatment often requires antibiotics. Understanding these connections helps you spot symptoms early and choose the right care.
Symptoms, Diagnosis, and Medication Safety
Typical signs include burning during urination, increased frequency, lower‑abdomen pressure, and sometimes blood in the urine that appears right before or during a period. Doctors usually confirm it with a urine dip‑stick test and a short culture, then consider your menstrual history to differentiate it from regular cystitis. Because many of our articles discuss drug safety—like how NSAIDs such as ketorolac can affect kidney function or how certain antibiotics interact with hormonal contraceptives—it's crucial to pick a medication that won’t upset your hormonal balance. For example, a short course of trimethoprim‑sulfamethoxazole works well for many, but if you’re on birth‑control pills, you might need a backup method due to potential interaction. Likewise, avoid high‑dose NSAIDs if you have underlying kidney concerns, as highlighted in our piece on ketorolac risks. Always check the dosage recommendations and ask your pharmacist about possible side effects, especially if you have a history of thyroid issues, which can be influenced by estrogen‑containing medications.
Managing menstrual cystitis doesn’t have to break the bank. Simple steps like staying well‑hydrated, urinating before and after sexual activity, and using a heating pad can reduce discomfort. Probiotic‑rich foods may support a healthy bladder microbiome, lowering infection chances. If antibiotics are needed, look for reputable online pharmacies that offer generic versions at lower prices—our guides on cheap generics for drugs like amoxicillin and cefalexin show how to save up to 80%. Keep a symptom diary to track any patterns linked to particular cycle days; this information is gold when discussing treatment with your clinician. With these practical tips and a clearer picture of how hormones, infections, and medications intersect, you’re ready to navigate the next steps. Below you’ll find a curated selection of articles that dive deeper into the safest drug choices, hormone‑related side effects, and cost‑effective treatment options for menstrual cystitis.
Manage Menstrual Bladder Pain: Practical Relief Tips
- Robin Tudge
- October 22, 2025
- 15 Comments
Learn why bladder pain spikes during periods and get practical tips-heat, diet, meds, and physical therapy-to ease discomfort fast.
read more