Dealing with a sore, urgent bladder right when your period starts can feel like a double whammy. You’re already coping with cramps, mood shifts, and fatigue, and now that burning sensation adds another layer of discomfort. This guide walks you through why the bladder gets cranky during menstruation and gives you straightforward ways to dial down the pain without piling on pills.
Quick Takeaways
- Identify if hormonal shifts, pelvic floor tension, or a hidden infection are behind the pain.
- Use heat, hydration, and gentle movement to calm the bladder fast.
- Try diet tweaks like magnesium‑rich foods and caffeine reduction.
- Over‑the‑counter NSAIDs work, but combine them with physical therapies for lasting relief.
- Seek medical advice if pain lasts beyond a week or is accompanied by fever.
First, let’s break down what’s really happening inside your body.
Why the Bladder Gets Painful During Your Period
When you notice bladder pain during menstruation, it’s usually tied to one of three culprits:
- Hormonal fluctuations - Estrogen and progesterone dip and surge, making the bladder lining more sensitive.
- Increased pelvic floor tension - Your pelvic floor muscles tighten to brace against menstrual cramping, squeezing the bladder.
- Underlying urinary issues - Conditions like interstitial cystitis or a silent urinary tract infection flare up when hormones shift.
Understanding which driver is at play helps you pick the right remedy instead of tossing a blanket over the problem.
Lifestyle Tweaks That Ease the Ache
Simple day‑to‑day moves can make a huge difference:
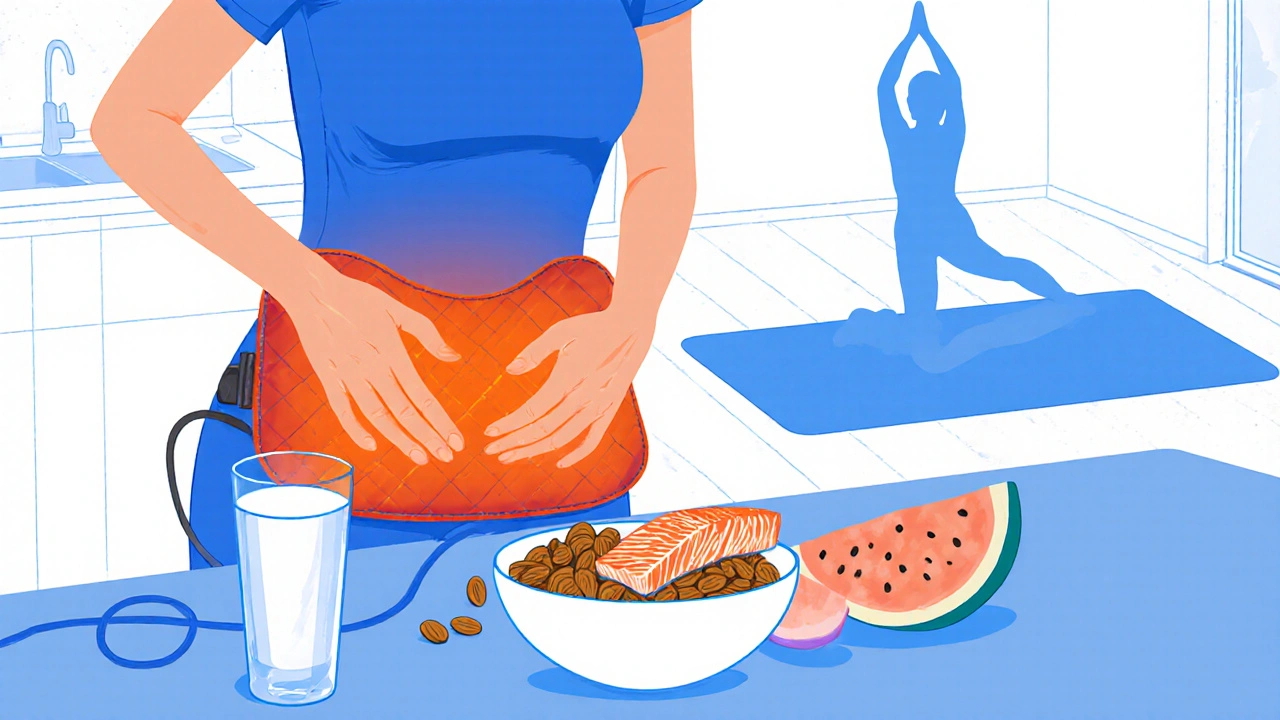
- Heat therapy - A warm water bottle or a low‑heat heating pad placed on your lower abdomen for 15‑20 minutes relaxes both the bladder wall and the surrounding pelvic floor.
- Gentle stretching - Yoga poses like Child’s Pose or the Supine Pelvic Tilt keep the pelvic floor from locking up.
- Stay hydrated - Aim for 8‑10 cups of water daily; sipping keeps urine dilute and reduces irritation.
- Timed bathroom trips - Going every 2-3 hours prevents the bladder from over‑filling, a common trigger for pain.
These habits are low‑cost, low‑risk, and can be combined with any other strategy you try.
Dietary Support: What to Eat (and What to Skip)
Food can either calm or inflame the bladder. Here’s a quick cheat‑sheet:
| Friendly | Irritant |
|---|---|
| Magnesium‑rich nuts (almonds, cashews) | Caffeinated coffee & energy drinks |
| Omega‑3 fatty fish (salmon, sardines) | Spicy sauces & hot peppers |
| Water‑rich fruits (watermelon, cucumber) | Artificial sweeteners (aspartame, sucralose) |
| Herbal teas (chamomile, peppermint) | Acidic juices (orange, grapefruit) |
Adding a daily magnesium supplement (200‑400 mg) can ease muscle cramps, while cutting back on caffeine often lessens urgency.
Over‑the‑Counter & Prescription Options
When lifestyle tweaks aren’t enough, medicines step in:
- NSAIDs like ibuprofen (400‑600 mg) target the inflammation caused by hormonal swings. Take with food to protect your stomach.
- Prescription anticholinergics (e.g., oxybutynin) calm an over‑active bladder, useful if you have frequent urges.
- For confirmed interstitial cystitis, doctors may recommend a low‑dose tricyclic antidepressant (amitriptyline) to relax bladder walls.
Never self‑diagnose; a quick doctor visit can confirm whether a prescription is needed.
Physical Therapies That Target the Pelvic Floor
Specialized care can unlock relief that pills can’t:
- Sitz bath - Sitting in warm (not hot) water for 10‑15 minutes soothes the perineal area and relaxes the pelvic floor.
- Pelvic floor physical therapy - A trained therapist teaches you “down‑release” techniques, using biofeedback to un‑tighten the muscles.
- Acupressure - Gentle pressure on points like SP6 (Sanyinjiao) has been shown to ease menstrual‑related bladder discomfort.
Most clinics offer a single session to assess whether a longer program is worth it.

When to Seek Professional Help
If any of these red flags appear, call your healthcare provider promptly:
- Pain that lasts more than 7 days after your period ends.
- Fever, chills, or blood in urine - signs of a genuine infection.
- Sudden increase in frequency (more than 10 trips a day) or inability to fully empty the bladder.
- Any new neurological symptoms such as numbness in the pelvis.
Early diagnosis can prevent chronic bladder issues from developing.
Relief Methods Comparison
| Method | Onset of Relief | Typical Cost | Ease of Use |
|---|---|---|---|
| Heat therapy | 15 min | Free‑to‑low | Very easy |
| NSAIDs | 30‑60 min | $0‑$10 per month | Easy |
| Magnesium supplement | 2‑3 days | $5‑$15 per month | Easy |
| Pelvic floor PT | 1‑2 weeks | $100‑$200 per session | Moderate |
| Prescription meds | 1‑2 days | Varies | Requires doctor |
Pick one or combine a few that match your schedule, budget, and severity. Many women find that heat + NSAIDs + magnesium covers most of the pain, while PT steps in for stubborn cases.
Frequently Asked Questions
Is bladder pain during my period normal?
A mild ache is common because hormonal swings sensitize the bladder lining. Persistent, sharp, or burning pain should be evaluated by a clinician.
Can I take ibuprofen if I have a stomach ulcer?
No. NSAIDs can irritate the stomach lining further. Talk to your doctor about alternatives like acetaminophen or a prescription that’s ulcer‑safe.
Will cutting caffeine help?
Yes. Caffeine is a bladder stimulant and can increase urgency and pain. Reducing or swapping for herbal tea often brings noticeable relief within a few days.
Is a sitz bath safe during menstruation?
Absolutely. Use warm (not hot) water for 10‑15 minutes. It soothes the perineum without affecting menstrual flow.
When should I consider a pelvic floor physical therapist?
If heat and OTC meds only provide temporary relief, or if you notice frequent pressure points, a PT can help retrain the muscles. A single assessment usually decides if a series is needed.
By mixing these strategies, you can keep bladder pain from stealing the spotlight during your period. Remember, each body reacts differently, so feel free to experiment and find the combo that works best for you.

All Comments
Don Goodman-Wilson October 22, 2025
Great, another excuse to avoid real problems.
Bret Toadabush October 23, 2025
The pharma cartels planted this tip to get us buying more meds, wake up!
Sarah Riley October 25, 2025
Symptomatic bladder hyperalgesia correlates with estrogenic nadir; consider neurogenic modulation.
Tammy Sinz October 26, 2025
Targeted pelvic floor release combined with magnesium supplementation yields measurable reduction in dysuria during menses.
Christa Wilson October 27, 2025
Totally agree 😊! Small changes can make a big difference.
John Connolly October 28, 2025
First, make sure you’re staying hydrated throughout the day; aim for at least eight glasses of water.
Second, apply a heating pad to the lower abdomen for 15‑20 minutes at the onset of discomfort.
Third, schedule regular bathroom trips every two to three hours to prevent over‑filling.
Fourth, incorporate gentle pelvic‑floor stretches like the child’s pose or supine pelvic tilt during your period.
Fifth, consider a daily magnesium supplement of 300 mg to help relax the smooth muscle.
Sixth, limit caffeine intake; replace coffee with herbal teas such as chamomile or peppermint.
Seventh, if pain persists, take an NSAID like ibuprofen with food, staying within the recommended dosage.
Eighth, track your symptoms in a journal to identify patterns and triggers.
Ninth, if you suspect an infection, don’t self‑diagnose-consult a healthcare provider for a urine test.
Tenth, a sitz bath in warm water for 10 minutes can soothe the perineal area.
Eleventh, explore acupressure point SP6 for additional relief.
Twelfth, if over‑the‑counter options aren’t enough, discuss prescription options with your doctor.
Thirteenth, pelvic‑floor physical therapy can provide lasting muscle re‑education.
Fourteenth, maintain a balanced diet rich in omega‑3 fatty acids and avoid spicy foods that may irritate the bladder.
Finally, remember that every body is different, so tailor the combination that works best for you.
Sajeev Menon October 29, 2025
Hey, dont forget to drink plenty of water and try a warm compress – it really helps calm the bladder pain, trust me!
Emma Parker October 30, 2025
I totally get it, the urgency can be maddening. I started doing the supine pelvic tilt before bed and it’s made a world of difference for me.
Wade Grindle October 31, 2025
Your suggestion to schedule bathroom trips is spot‑on; I’ve found that emptying every two hours prevents the burning sensation from escalating.
Jai Reed November 2, 2025
Stop wasting time on vague tips; the only proven method is combining NSAIDs with a magnesium regimen and a structured PT program.
Sameer Khan November 3, 2025
From a neuro‑physiological perspective, the interplay between estrogen withdrawal and autonomic bladder innervation warrants a multimodal therapeutic approach.
WILLIS jotrin November 4, 2025
I’ve tried the heating pad and the timed voiding technique; both are simple yet surprisingly effective for reducing that sharp bladder ache.
Vin Alls November 5, 2025
Picture this: a cozy warm bottle hugging your lower belly while you sip a soothing chamomile tea – pure bliss for a cranky bladder.
Tiffany Davis November 6, 2025
Thanks for the thorough guide; I’ll try the heat and magnesium combo this month.
Diane Thurman November 7, 2025
This article reads like a marketing brochure, full of generic tips that anyone with a basic search can find.