Medication Errors: How They Happen and How to Prevent Them
When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug errors, they’re one of the most common causes of preventable harm in healthcare. These aren’t just rare accidents. They happen in hospitals, pharmacies, nursing homes, and even at home when people mix up pills or forget to tell their doctor about other meds they’re taking.
Dose verification, the process of double-checking medication amounts before giving them is one of the biggest shields against these mistakes. Nurses and pharmacists use barcode scanners and SBAR checklists to cut down on mix-ups, especially with high-alert drugs, medications like insulin, blood thinners, or opioids that can cause serious harm if given wrong. But even the best systems fail when communication breaks down. A doctor writes "0.5 mg" instead of "5 mg," a pharmacist misreads it, and the patient gets ten times the dose. That’s not a glitch—it’s a system gap.
It’s not just about who writes the script. Generic drugs, lower-cost versions of brand-name medicines that must meet the same FDA standards are used by millions, but confusion still happens. Patients think generics are "weaker," or worse, they get switched between brands without knowing. Some older generics made overseas have raised quality concerns, and patients don’t always know to ask. When you’re on multiple meds—say, levothyroxine and iron, or Bactrim and blood pressure pills—timing and interactions matter. One wrong combo can spike potassium, wreck your kidneys, or send your blood pressure crashing.
These aren’t theoretical risks. Look at the posts below: antibiotic rashes mistaken for allergies, fluoroquinolones tearing tendons, trimethoprim pushing potassium to dangerous levels, and PDE5 inhibitors causing deadly drops in blood pressure when mixed with nitrates. These aren’t edge cases. They’re everyday mistakes that happen because people don’t know what to watch for. And they’re preventable.
You don’t need to be a doctor to spot red flags. If a new pill makes you feel weird, if your doctor changes your dose without explaining why, if your pharmacy gives you a different-looking pill without telling you—it’s okay to ask. Again. And again. The system isn’t perfect. But your voice can stop a mistake before it starts.
Below, you’ll find real stories, clear explanations, and practical steps from clinicians and patients who’ve been there. From how to verify your dose to why some generics cost 20 times more than others, these posts cut through the noise. No fluff. Just what you need to stay safe, informed, and in control of your meds.
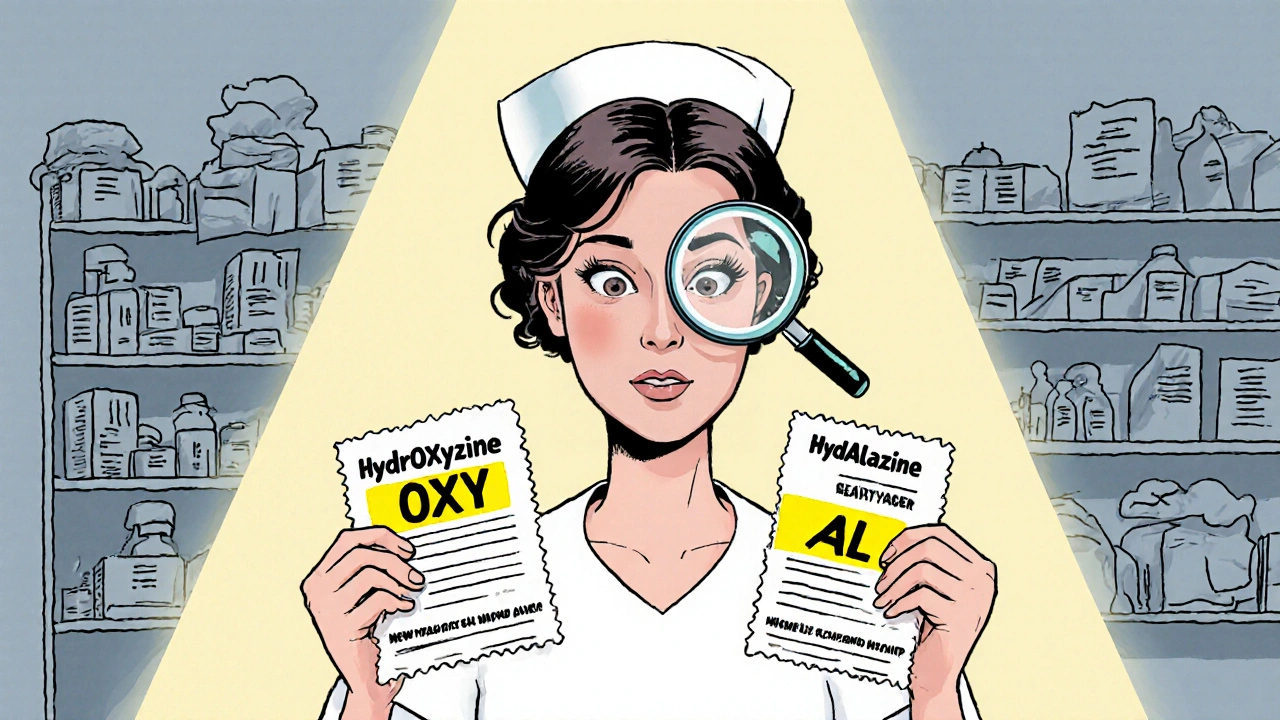
How to Identify Look-Alike Names on Prescription Labels
- Robin Tudge
- November 27, 2025
- 13 Comments
Learn how to spot dangerous look-alike drug names on prescription labels using tall man lettering, barcode scanning, and verification steps. Reduce medication errors with proven strategies used in U.S. hospitals.
read more