In Vitro Dissolution: What It Means for Generic Drug Quality and How It Affects Your Medication
When you take a generic pill, you expect it to work just like the brand-name version. That’s not luck—it’s because of in vitro dissolution, a lab test that measures how quickly a drug breaks down and dissolves in a controlled, artificial environment. Also known as drug dissolution testing, it’s one of the first things the FDA checks before approving any generic medication. This isn’t just paperwork—it’s the foundation of whether your medicine will actually get into your bloodstream and do its job.
Think of it like this: if a pill doesn’t dissolve properly in the lab, it won’t dissolve properly in your stomach. That means you might not get the full dose, even if the tablet looks identical to the brand. That’s why bioequivalence, the standard that proves a generic drug performs the same as the brand in your body, starts with in vitro dissolution. If the dissolution profile doesn’t match—same speed, same pattern—the FDA won’t approve it. This test catches problems before the drug ever reaches you, whether it’s a generic made in India, the U.S., or anywhere else. It’s also why some generics cost way less than others: cheaper ones might cut corners on ingredients or manufacturing, and dissolution testing helps spot those.
Related to this is drug absorption, how well your body takes in the active ingredient after the pill breaks down. Dissolution affects absorption directly. If a tablet dissolves too fast, you might get a spike in blood levels. Too slow, and you get no effect. That’s why the FDA doesn’t just look at one number—they compare the entire dissolution curve over time. This is especially critical for drugs like levothyroxine or iron supplements, where timing and consistency matter. Even small differences in dissolution can throw off your thyroid levels or cause side effects.
And it’s not just about safety. In vitro dissolution testing is how regulators catch bad batches, fake drugs, or poorly made generics. We’ve seen cases where overseas manufacturers used cheaper fillers that didn’t dissolve right—leading to drug shortages or ineffective treatments. The FDA uses these tests during inspections and after complaints. So when you hear about quality concerns with generics, it often starts with a dissolution test that didn’t pass.
What you’ll find in the posts below are real-world examples of how this invisible test impacts your health. From how generic drugs are approved to why some cost more than others, from thyroid meds to antibiotics, every post ties back to one thing: if the pill doesn’t dissolve right, it doesn’t work right. You’ll see how manufacturers are held to these standards, what happens when they’re not, and how you can tell if your medication is truly reliable. No fluff. Just the facts that keep your treatment effective—and your money well spent.
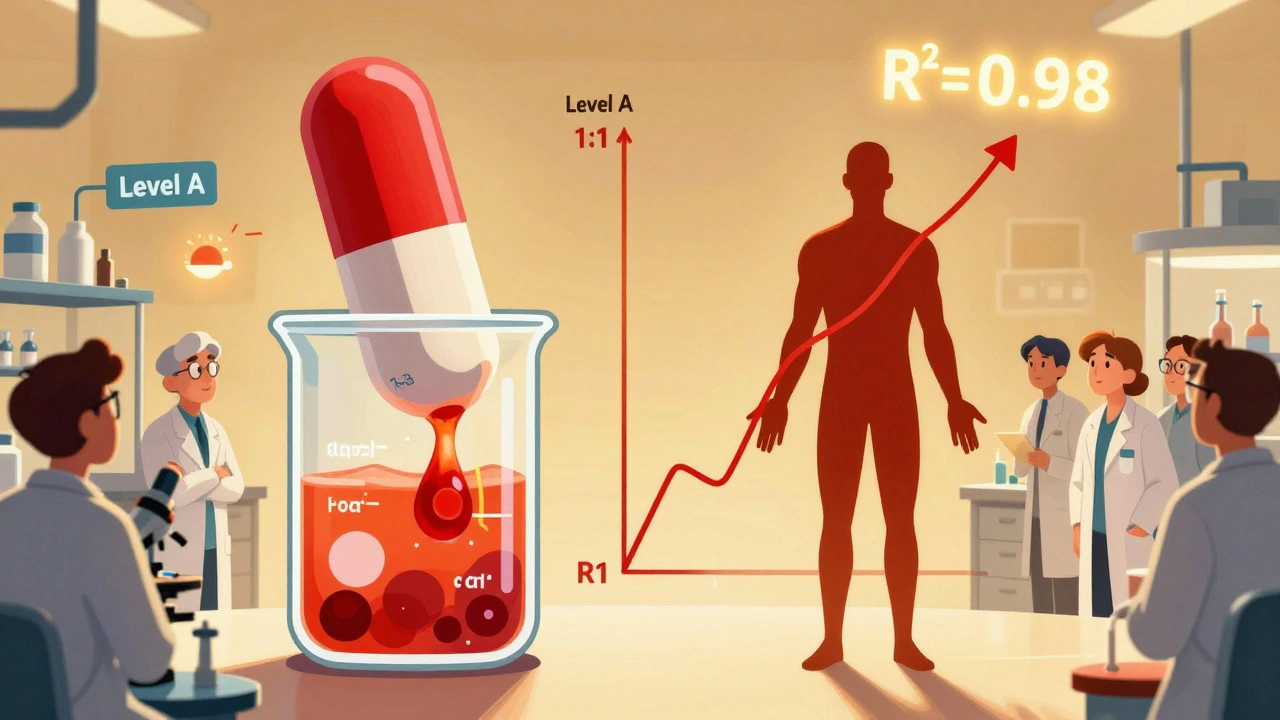
IVIVC and Waivers: How In Vitro Methods Are Replacing In Vivo Bioequivalence Testing
- Robin Tudge
- December 6, 2025
- 15 Comments
IVIVC lets generic drug makers replace costly human bioequivalence tests with lab-based dissolution data. Learn how Level A correlations work, why most submissions fail, and how biorelevant methods are changing the game.
read more