For decades, proving that a generic drug works the same as the brand-name version meant testing it on people. Dozens of healthy volunteers, blood draws every hour, weeks of planning, and costs that could hit $2 million per study. But now, in many cases, that’s no longer necessary. Instead, scientists are using a test tube and a dissolution machine to predict how a drug will behave inside the human body. This is IVIVC - In Vitro-In Vivo Correlation - and it’s quietly changing how generic drugs get approved.
What Is IVIVC, Really?
IVIVC stands for In Vitro-In Vivo Correlation. That sounds like jargon, but it’s simple: it’s a mathematical link between how a drug dissolves in a lab (in vitro) and how it gets absorbed in the body (in vivo). If you can show that the rate and amount of drug released from a pill in a beaker accurately predicts how much of it enters the bloodstream in a person, you don’t need to run a full clinical trial. You can skip the blood draws and just use dissolution data to prove bioequivalence.
This isn’t theoretical. The FDA first laid out clear rules for IVIVC in 1996 and updated them in 2014. The European Medicines Agency followed with similar guidance. Today, if you’re making a generic version of an extended-release pill - say, a 12-hour painkiller - and you can build a strong IVIVC model, you might avoid 3 to 5 full bioequivalence studies. That’s not just saving money. It’s cutting development time by a year or more.
The Four Levels of IVIVC - And Why Level A Matters Most
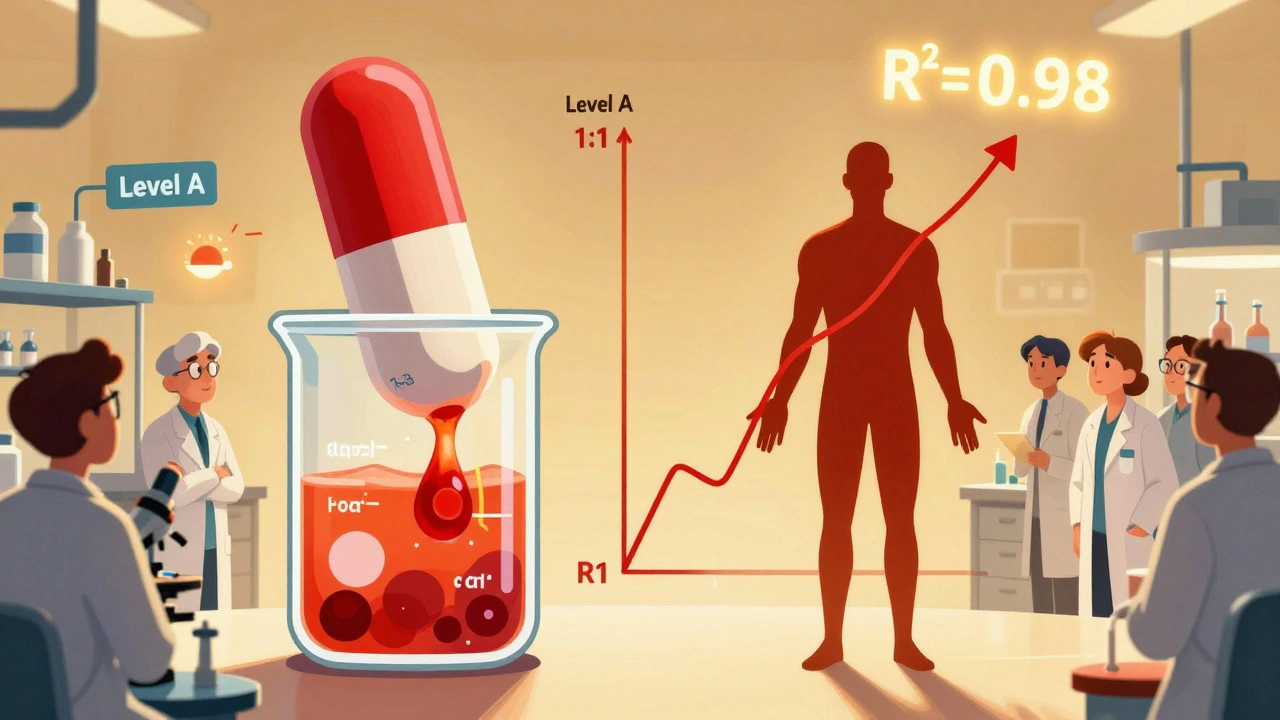
Not all correlations are created equal. The FDA classifies IVIVC into four levels, and only one really lets you skip human testing entirely: Level A.
- Level A: This is the gold standard. It matches dissolution at every time point to blood concentration at every time point. Think of it like a perfect mirror - if the pill releases 20% of the drug at 1 hour in the lab, the body absorbs exactly 20% at that same time. For this to work, the model needs an R² value above 0.95, a slope near 1.0, and an intercept near zero. Only Level A can predict the full pharmacokinetic profile. This is what regulators want for biowaivers.
- Level B: Uses averages. It links the average time the drug dissolves to the average time it stays in the body. Useful for some cases, but doesn’t predict individual time points. Not enough for a waiver.
- Level C: Links one dissolution number - like “80% dissolved at 2 hours” - to one blood parameter, like Cmax. It’s easier to build but risky. It might miss how the drug behaves later in the day.
- Multiple Level C: Uses several dissolution points to predict multiple pharmacokinetic values. More robust than single Level C, but still not as reliable as Level A.
The FDA requires Level A models to predict AUC within ±10% and Cmax within ±15% to be accepted. That’s strict. But when it works, it’s powerful.
Why Companies Are Trying (and Often Failing) to Use IVIVC
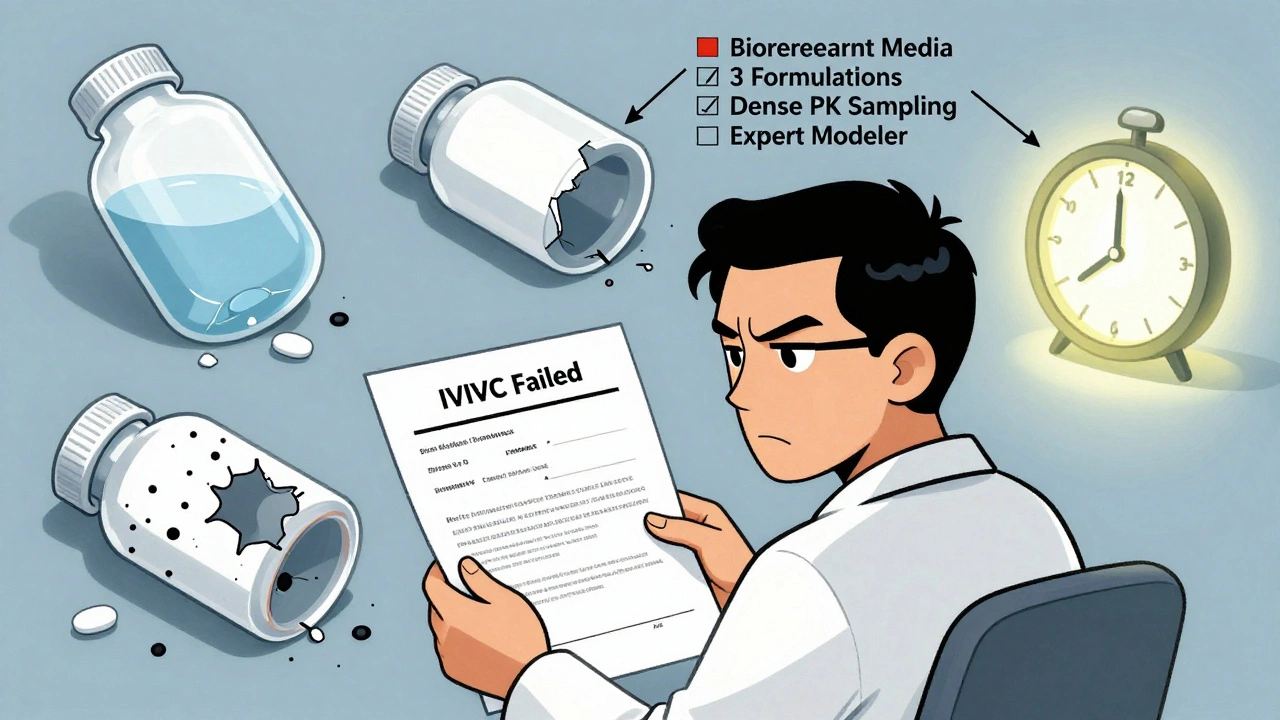
Here’s the reality: 68% of generic drug makers have tried to build an IVIVC model. Only 29% got approved on their first try. Why the high failure rate?
First, you need the right formulations. You can’t just test one version of the pill. You need at least three to five versions with different release rates - slow, medium, fast. That means making and testing multiple prototypes. Many companies skip this step because it’s expensive and time-consuming.
Second, your dissolution method must be discriminatory. If your test can’t tell the difference between a 5% change in a key ingredient, it’s useless. The FDA requires dissolution methods that detect real formulation differences - not just random noise. Too many companies use outdated methods designed for immediate-release pills, not complex extended-release ones.
Third, you need high-quality pharmacokinetic data. That means running multiple human studies - at least three, with 12 to 24 people each - with dense blood sampling. You can’t just take a few samples at 1, 2, and 4 hours. You need data every 30 to 60 minutes for 24 hours or more. That’s expensive. And if your data is messy or incomplete, the model collapses.
One company spent $1.2 million over 18 months on an IVIVC for a modified-release product - only to have it fail because the model didn’t account for food effects. Real people eat. Real stomachs change pH. Lab conditions don’t always reflect that.
When IVIVC Works Best - And When It Doesn’t
IVIVC isn’t a magic bullet. It shines in one area: extended-release oral products. Think opioid painkillers, antidepressants with once-daily dosing, or blood pressure meds that last 24 hours. These are complex. They rely on special coatings, matrices, or osmotic systems. For these, BCS (Biopharmaceutics Classification System) waivers - which rely on solubility and permeability - don’t work. IVIVC is the only viable path to a biowaiver.
But it fails in three key cases:
- Narrow therapeutic index drugs: Like warfarin or lithium. A tiny difference in absorption can cause toxicity or treatment failure. Regulators won’t accept a model here - they want real human data.
- Non-linear pharmacokinetics: If the drug’s absorption changes unpredictably with dose, a simple dissolution model can’t capture it.
- Non-oral products: Injectables, inhalers, eye drops - these are still mostly off-limits. But that’s changing. The FDA released draft guidance in June 2023 for topical products. The EMA is exploring IVIVC for implants. The next frontier is here.
For immediate-release drugs, the BCS pathway is simpler. If the drug is highly soluble and highly permeable (Class I), you can often skip human studies with just dissolution data and no IVIVC model. But if your drug is poorly soluble or doesn’t absorb well - you’re stuck with IVIVC or full bioequivalence studies.
The Rise of Biorelevant Dissolution
Early IVIVC models used simple buffers - water with a fixed pH. That’s fine for aspirin. Not for a drug that dissolves only in the small intestine, or one that’s affected by bile salts.
That’s why biorelevant dissolution is becoming standard. Instead of plain water, labs now use fluids that mimic stomach and intestinal conditions - pH that changes over time, bile salts, enzymes, even food particles. This isn’t fancy. It’s necessary.
University of Maryland research in 2019 showed that biorelevant media improved IVIVC success rates by 40% for complex products. The FDA now expects it. By 2025, 75% of new IVIVC submissions will use biorelevant methods, according to the American Association of Pharmaceutical Scientists.
Companies using standard compendial methods (like USP Apparatus 2 with pH 6.8 buffer) are seeing their submissions rejected. The science has moved on. If you’re still using old methods, you’re not just behind - you’re out of compliance.
Who’s Winning at IVIVC - And Who’s Falling Behind
IVIVC isn’t for everyone. It requires deep expertise in pharmacokinetics, formulation science, and statistical modeling. Only about 15% of pharmaceutical companies have this in-house.
That’s why the big players dominate. Teva, Sandoz, Mylan, Sun Pharma, and Lupin all have dedicated IVIVC teams. In 2021, Teva spent 14 months and three formulation iterations to get FDA approval for an IVIVC model for extended-release oxycodone. The payoff? They avoided five full bioequivalence studies - saving millions and accelerating market entry.
Smaller companies? They’re outsourcing. Contract research organizations like Alturas Analytics and Pion report success rates of 60-70% for Level A models when they’re brought in early. But if you wait until your product is nearly ready for submission, your odds drop to under 30%.
Approval rates are rising. In 2018, only 15% of IVIVC submissions were accepted. By 2022, that jumped to 42%. Why? Better science. Better tools. And regulators who are now more willing to work with companies to fix models before rejection.

The Future: Machine Learning and Global Harmonization
IVIVC is getting smarter. In 2024, the FDA and EMA held a joint workshop on machine learning-enhanced IVIVC models. Instead of linear regression, companies are now using AI to find hidden patterns in dissolution and blood data. These models can handle more variables - food, pH shifts, gastric emptying - without needing a dozen extra human studies.
But there’s a catch. Regulators want transparency. You can’t use a black-box AI model. You have to explain how it works. The science must be open, reproducible, and validated with real-world data.
Global harmonization is also accelerating. What’s accepted in the U.S. is more likely to be accepted in Europe and Japan. That’s good news. It means one IVIVC model can support approvals in multiple markets - reducing duplication and cost.
By 2027, McKinsey & Company projects that 35-40% of all modified-release generic approvals will rely on IVIVC waivers - up from 22% in 2022. That’s not a trend. It’s a transformation.
What You Need to Know Before You Start
If you’re developing a generic extended-release product, here’s your roadmap:
- Start early. Don’t wait until your final formulation. Begin IVIVC planning during prototype development.
- Build a discriminatory dissolution method. Use biorelevant media. Test at least three different pH levels and include bile salts if needed.
- Make multiple formulations. At least three - fast, medium, slow release. This gives you the data range you need to build a strong model.
- Run dense PK studies. Minimum 12 time points per subject over 24+ hours. Use the same sampling schedule for all formulations.
- Partner with experts. If you don’t have a pharmacokinetic modeler on staff, hire one. Don’t try to build this alone.
- Validate rigorously. Use cross-validation. Test your model on data it didn’t see. If it can’t predict new results, it’s not valid.
Failure isn’t the end. It’s feedback. The FDA will tell you exactly why your model was rejected. Use that to improve. Many companies submit twice. The second time, they get approved.
Is IVIVC the Future of Bioequivalence?
Yes - but not for everything. For simple immediate-release drugs, BCS waivers will still dominate. For complex, extended-release products, IVIVC is becoming the standard. It’s faster, cheaper, and more ethical - no need to expose volunteers to repeated dosing just to prove a pill works.
The days of running dozens of bioequivalence studies for every minor formulation change are ending. With IVIVC, manufacturers can make small tweaks - change a coating, switch a supplier, move production lines - without going back to human trials. That’s innovation. That’s efficiency. And that’s the future of generic drugs.
It’s not easy. It’s not cheap. But when done right, IVIVC turns a lab test into a lifeline - for patients who need affordable medicine, and for companies who want to bring it to market.
What is the main purpose of IVIVC in generic drug development?
The main purpose of IVIVC is to establish a scientifically valid link between how a drug dissolves in a lab setting and how it behaves in the human body. When this correlation is strong enough - especially at Level A - regulators like the FDA can approve a generic drug without requiring a full human bioequivalence study. This saves time, reduces costs, and avoids exposing volunteers to repeated dosing.
Can IVIVC be used for all types of drugs?
No. IVIVC works best for extended-release oral products where dissolution controls absorption. It’s not accepted for narrow therapeutic index drugs like warfarin or lithium, drugs with non-linear pharmacokinetics, or non-oral products like injections or inhalers - though research is expanding into these areas. For immediate-release drugs, the BCS pathway is often simpler and preferred.
Why do most IVIVC submissions get rejected?
The top reasons for rejection are: 1) dissolution methods that aren’t discriminatory enough to detect real formulation differences, 2) insufficient coverage of formulation variations (too few prototypes tested), and 3) lack of physiological relevance - using plain water or fixed pH instead of biorelevant media that mimic stomach and intestinal conditions. About 64% of rejections in 2023 were due to inadequate dissolution conditions.
What’s the difference between Level A and Level C IVIVC?
Level A provides a point-to-point match between dissolution and absorption at every time point - it can predict the entire blood concentration curve. Level C links just one dissolution value (like % dissolved at 2 hours) to one pharmacokinetic parameter (like Cmax). Level A is required for full biowaivers. Level C may be accepted in some cases with extra data, but it’s less reliable and doesn’t predict the full profile.
How much does it cost to develop an IVIVC model?
Developing a successful IVIVC model typically costs $1 million to $2 million and takes 12 to 18 months. This includes formulation development, dissolution method optimization, running multiple human pharmacokinetic studies, and model validation. But it saves $1-2 million per avoided bioequivalence study - and often prevents five or more such studies.
Is IVIVC accepted globally?
Yes. Both the U.S. FDA and the European Medicines Agency (EMA) accept IVIVC for regulatory waivers, and their guidelines are increasingly aligned. Japan’s PMDA also recognizes IVIVC. A well-designed model meeting FDA or EMA standards is likely to be accepted in other major markets, making global approval more efficient.
What role does biorelevant dissolution play in IVIVC?
Biorelevant dissolution uses fluids that mimic the human gastrointestinal tract - changing pH, bile salts, enzymes, and food components. Traditional dissolution in plain buffer often fails to predict real-world absorption. Biorelevant media improve correlation accuracy by 30-40% and are now expected by regulators for complex products. By 2025, 75% of new IVIVC submissions are projected to use them.
Can IVIVC be used for post-approval changes?
Yes. Once an IVIVC model is approved, it can support waivers for certain post-approval changes - like scale-up, minor formulation adjustments (within ±5% for non-critical excipients), or manufacturing site transfers - as long as the dissolution profile remains similar (f2 similarity factor >50). Without IVIVC, each of these changes would require a new bioequivalence study.

All Comments
Mayur Panchamia December 6, 2025
IVIVC? Finally! India's generic giants are gonna crush this game-no more begging the FDA for human trials! We've got the labs, the brains, the patience. Why should Americans keep hoarding bioequivalence studies like they're gold bars? We're not just making pills-we're making history. And yes, I said it: Level A is the only way. No compromises. No excuses. We're not here to play nice-we're here to dominate.
Andrew Frazier December 8, 2025
lol who cares about level A when you can just slap a ‘bioequivalent’ sticker on it? FDA’s been asleep at the wheel since 2014. My cousin works at a lab in Ohio-he says half the ‘validated’ models are just Excel sheets with trendlines drawn by interns. They call it science. I call it magic. And yeah, I said magic. With glitter.
Ibrahim Yakubu December 9, 2025
This is why Africa is left behind. We don’t have the money for biorelevant media. We don’t have the equipment. We don’t even have stable electricity in some places. Meanwhile, you guys are debating R² values like it’s a TED Talk. IVIVC? Sure. But only for the rich. The rest of us still need real people to test drugs. Real people who can’t afford the brand. Real people who die waiting.
Nava Jothy December 10, 2025
Ugh. Another whitepaper pretending to be progress. 😒 You think this is innovation? It’s just corporate greed in a lab coat. They’re not saving lives-they’re saving $$$ by skipping human testing. And then they wonder why people don’t trust pharma. 🤦♀️ I’ve seen too many ‘bioequivalent’ generics that made patients sick. Don’t be fooled by fancy graphs. The body isn’t a beaker. It’s a miracle. And you’re reducing it to data points.
olive ashley December 11, 2025
Let’s be real-this whole IVIVC thing is a scam. The FDA approves these models because they’re understaffed and overworked. They don’t have time to run 500 human trials. So they take the path of least resistance. And guess what? Companies know that. They game the system. Build a model that looks good on paper, ignore food effects, and bingo-approval. Then someone has a seizure because the generic didn’t absorb right. And nobody gets held accountable. It’s not science. It’s liability laundering.
joanne humphreys December 12, 2025
It’s fascinating how much we’ve evolved in drug testing. I remember when bioequivalence meant 12 volunteers in a hospital bed for two weeks. Now we can predict absorption with a machine and a cup of simulated gastric fluid. It’s elegant. It’s efficient. And honestly? It’s more ethical. Less burden on volunteers. Fewer risks. More access to medicine. I just hope we keep the human element in mind-data doesn’t feel pain, but people do.
pallavi khushwani December 12, 2025
IVIVC feels like the quiet revolution nobody talks about. We’re moving from ‘test on people’ to ‘understand the science.’ It’s not perfect-but nothing worth doing ever is. I love how the FDA is finally pushing for biorelevant media. It’s like they finally realized: the stomach isn’t tap water. 🌱 I’m hopeful. This could mean cheaper meds for everyone. Even in small towns. Even in villages. That’s the dream, right?
Katie O'Connell December 13, 2025
It is imperative to underscore that the regulatory acceptance of Level A IVIVC models constitutes a paradigmatic shift in pharmaceutical development methodology. The empirical validation of dissolution profiles against pharmacokinetic parameters necessitates a rigorous, multi-variable analytical framework that transcends mere statistical correlation. Failure to adhere to the stringent criteria delineated by the FDA and EMA constitutes a fundamental breach of scientific integrity, and may engender catastrophic therapeutic outcomes. One must not conflate expediency with efficacy.
brenda olvera December 14, 2025
I just want to say-thank you for writing this. I’m from Mexico, and my mom takes a generic blood pressure pill. We used to worry every time the bottle changed. Now I understand why. IVIVC isn’t just about money. It’s about consistency. About trust. About knowing that the pill you get in a small town pharmacy works the same as the one in the city. That’s not science fiction. That’s real progress.
Saketh Sai Rachapudi December 15, 2025
India made this possible! We have the best chemists, the cheapest labs, the most disciplined workers. Why do you think the US imports 80% of its generics? Because we outsmarted them. We didn’t wait for permission-we built the models, we ran the tests, we proved it. And now they’re copying OUR methods. Level A? We invented it in our sleep. And we’re not stopping. Not now. Not ever. 🇮🇳💪
Akash Takyar December 16, 2025
While I acknowledge the technical merits of IVIVC, I remain cautiously optimistic regarding its scalability and long-term reliability. The assumption that dissolution kinetics can fully encapsulate the complexity of human physiology-particularly with regard to inter-individual variability, gut microbiota, and metabolic polymorphisms-remains, in my view, an overreach. A model may be statistically robust, but biological systems are inherently stochastic. We must not mistake precision for truth.
Myles White December 17, 2025
Look, I’ve worked in formulation for 18 years. I’ve seen IVIVC fail more times than I’ve had hot dinners. But here’s the thing-it’s not about the model. It’s about the team. The companies that win? They hire the right people early. They don’t wait until the product’s done. They start with the dissolution method before they even pick the polymer. They run three different formulations before breakfast. They use biorelevant media because they know it’s not optional anymore. And they don’t try to do it alone-they partner with the CROs who’ve done this 50 times. It’s not magic. It’s discipline. And discipline? That’s what separates the winners from the ones who spend $1.2 million and get rejected anyway.
Kenny Pakade December 19, 2025
Oh great, another ‘innovation’ that lets big pharma skip testing. Next they’ll say we don’t need to test insulin on diabetics because a machine ‘predicted’ it. This isn’t progress-it’s corporate laziness dressed up as science. And don’t even get me started on how they’ll use this to push cheaper generics into developing countries. ‘Oh don’t worry, the model says it’s safe!’ Right. And I’m the Queen of England. This is a disaster waiting to happen.
Karen Mitchell December 19, 2025
This entire post reads like a pharmaceutical industry lobbying document. You speak of ‘efficiency’ and ‘cost savings’ as if those are moral virtues. But where is the accountability? Where is the patient safety? You’ve replaced human beings with dissolution curves, and now you’re patting yourselves on the back for being ‘ethical.’ This isn’t ethics-it’s detachment. And it’s dangerous. If a child dies because a Level A model missed a food interaction, will you still call it progress? Or will you just say, ‘The model was statistically valid’?
Geraldine Trainer-Cooper December 21, 2025
it's just a fancy way of saying 'we don't want to do the hard work anymore'