FDA Requirements: What You Need to Know About Drug Safety and Approval
When you take a pill, whether it’s a brand-name drug or a cheap generic, you’re relying on FDA requirements, the set of rules enforced by the U.S. Food and Drug Administration to ensure drugs are safe, effective, and properly labeled. Also known as drug regulatory standards, these rules determine what gets on pharmacy shelves and what gets pulled off them. The FDA doesn’t just approve drugs once and walk away. They keep watching—through inspections, side effect reports, and updates to warnings. If a drug causes unexpected harm, the FDA can slap on a boxed warning, the strongest safety alert the agency issues, often for drugs that can cause serious injury or death. You’ll find these warnings on medications like fluoroquinolones, PDE5 inhibitors, and even some antibiotics.
FDA requirements also cover how drugs are made. That’s why FDA inspections, unannounced visits to manufacturing plants, both domestic and overseas, to check for cleanliness, accuracy, and compliance matter so much. A lot of generic drugs are made in India or China, and not all factories follow the same standards. Recent data shows some older generics have higher rates of severe side effects—not because the active ingredient is different, but because of how it’s produced. The FDA isn’t perfect, but their inspections are the main line of defense against contaminated or ineffective pills.
And then there’s the difference between generics and biosimilars. The FDA treats them differently because they’re not the same thing. Generic drugs, are simple copies of chemical-based medications, made to match the brand-name version in strength, dosage, and effect. Biosimilars, on the other hand, are copies of complex biologic drugs made from living cells. They’re harder to replicate exactly, so the FDA demands more testing. Both save money, but only generics can be swapped in automatically at the pharmacy. Biosimilars? Often need a doctor’s okay.
FDA requirements also shape how drug information gets to you. That’s why some medications come with clear, plain-language guides—because the FDA knows confusion kills. If a patient doesn’t understand how to time iron with thyroid meds, or why they can’t mix energy drinks with Adderall, the risk goes up. The agency pushes for better labeling, better warnings, and better education. And when a drug’s risks change—like when trimethoprim was found to spike potassium levels in older adults—the FDA updates its guidance. That’s why you see new boxed warnings every year.
What you’ll find below isn’t just a list of articles. It’s a real-world look at how FDA requirements play out in clinics, pharmacies, and homes. From how tall man lettering prevents deadly mix-ups to why some generics cost 20 times more than others, these posts show you the hidden rules behind your medicine. You’ll learn what to ask your pharmacist, how to spot a risky interaction, and when to push back if something doesn’t feel right. This isn’t theory. It’s what keeps you safe.
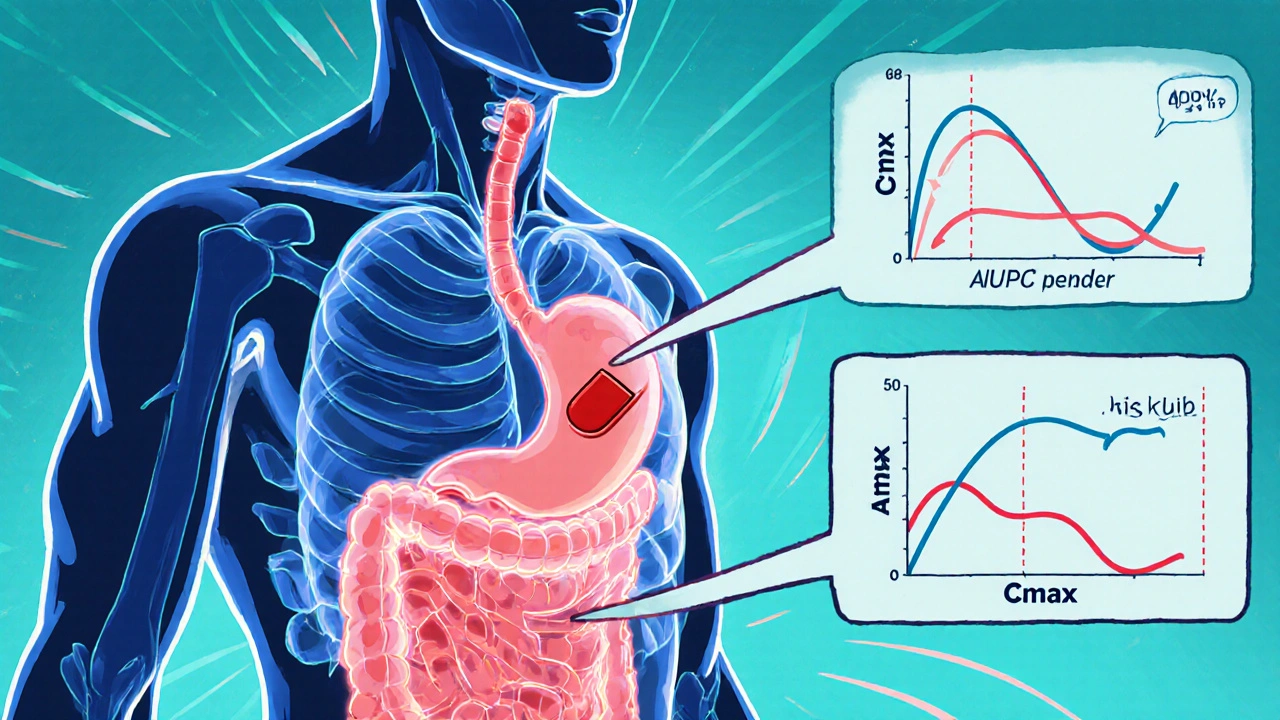
Bioequivalence Studies: What the FDA Requires Generic Drug Manufacturers to Prove
- Robin Tudge
- November 29, 2025
- 8 Comments
Learn what the FDA requires generic drug makers to prove through bioequivalence studies to ensure their products work just like brand-name drugs. Key criteria, exceptions, and recent updates explained.
read more