Drug Side Effects: What They Are, Why They Happen, and How to Spot Them
When you take a medication, your body doesn’t always react the way the label promises. Drug side effects, unintended physical or mental reactions to a medication that aren’t the intended therapeutic outcome. Also known as adverse drug reactions, they can be as simple as a dry mouth or as serious as a heart rhythm gone wrong. These aren’t mistakes—they’re predictable outcomes of how drugs interact with your biology. Even safe, FDA-approved medicines can cause side effects because your body isn’t a factory with one clear path. It’s a living system full of variables: age, genetics, other drugs you take, liver function, even what you ate that morning.
Some drug interactions, when two or more medications combine to create unexpected or dangerous effects are well-known, like mixing PDE5 inhibitors with nitrates and risking a sudden drop in blood pressure. Others are quieter but just as dangerous. Trimethoprim in Bactrim can spike potassium levels, especially in older adults on blood pressure pills. Steroids like prednisone can trigger high blood sugar—even in people who’ve never had diabetes. These aren’t rare accidents. They’re documented, studied, and often avoidable if you know what to watch for.
Generic drug risks, concerns about quality and consistency in lower-cost versions of brand-name medicines have become a real talking point. Some clinicians report higher rates of severe reactions with older generics made overseas, especially those with thin profit margins. It’s not that generics are unsafe by design—it’s that manufacturing standards vary. A pill that looks identical to the brand name might have different fillers, coatings, or dissolution rates that change how your body absorbs it. That’s why some people get a rash on one brand of amoxicillin and not another.
And it’s not just about what’s in the pill. Social media is now a frontline tool for spotting new side effects. Patients report tendon pain after taking ciprofloxacin, confusion after starting a new antidepressant, or swelling after a new blood pressure med. These real-world reports help regulators catch problems faster than clinical trials ever could. But not all posts are reliable. That’s why experts still need to validate signals before changing guidelines.
You don’t need to be a doctor to protect yourself. If a new symptom shows up after starting a drug, write it down. Note when it started, how bad it is, and whether it got worse after you took another pill. Was it after you switched from a brand to a generic? Did you start a new supplement? Did you skip a meal? These details matter. Many side effects—like antibiotic rashes or steroid-induced diabetes—can be managed if caught early. Others, like fluoroquinolone nerve damage, can become permanent if ignored.
There’s no such thing as a drug without risk. But there is such a thing as a well-informed patient. The posts below break down real cases: how corticosteroids mess with blood sugar, why some antibiotics cause rashes that aren’t allergies, how common painkillers can hurt your kidneys, and why timing your iron with thyroid meds matters. You’ll find what to watch for, when to call your doctor, and how to ask the right questions. No fluff. No jargon. Just what you need to stay safe while taking the meds you need.
Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
- Robin Tudge
- December 20, 2025
- 0 Comments
Taking five or more medications increases the risk of falls, confusion, and death. Learn how polypharmacy harms older adults and what deprescribing can do to restore safety and quality of life.
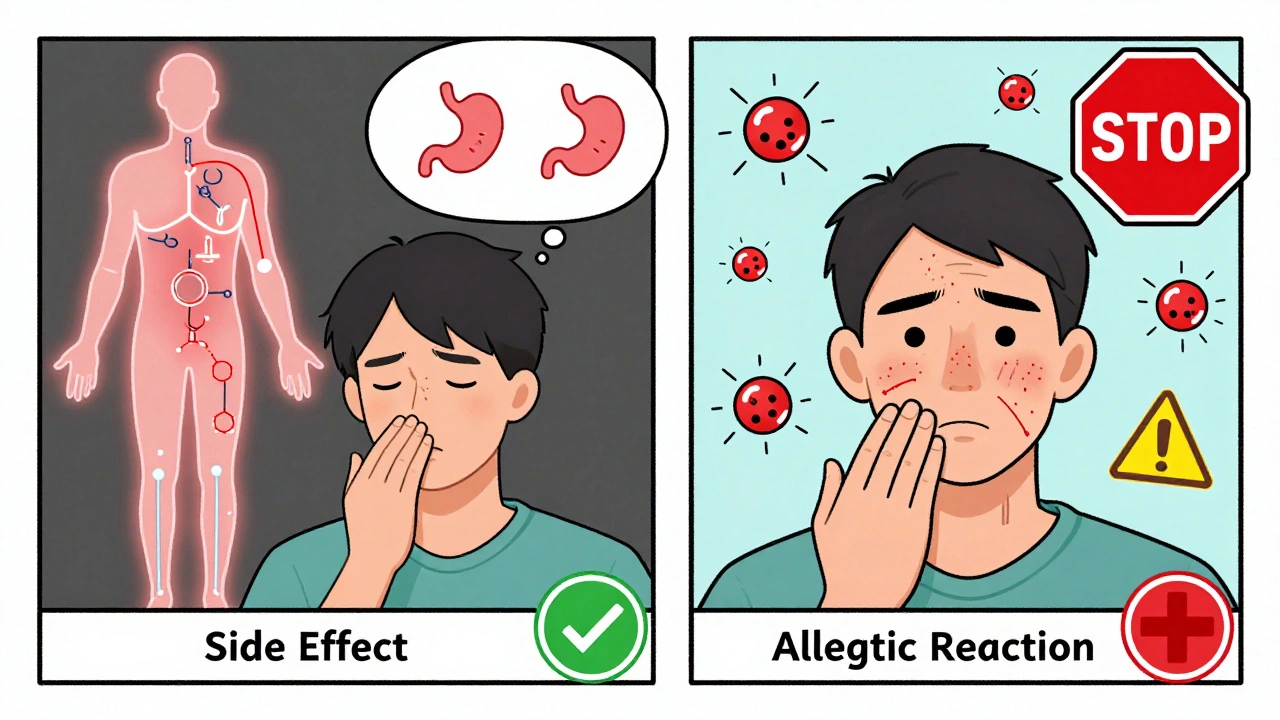
read moreDifference Between Medication Side Effects and Allergic Drug Reactions
- Robin Tudge
- December 3, 2025
- 8 Comments
Learn the key differences between medication side effects and true allergic drug reactions. Discover why mislabeling side effects as allergies leads to unnecessary risks, higher costs, and worse health outcomes.
read more