Drug Hypersensitivity: Signs, Risks, and What to Do When Your Body Reacts
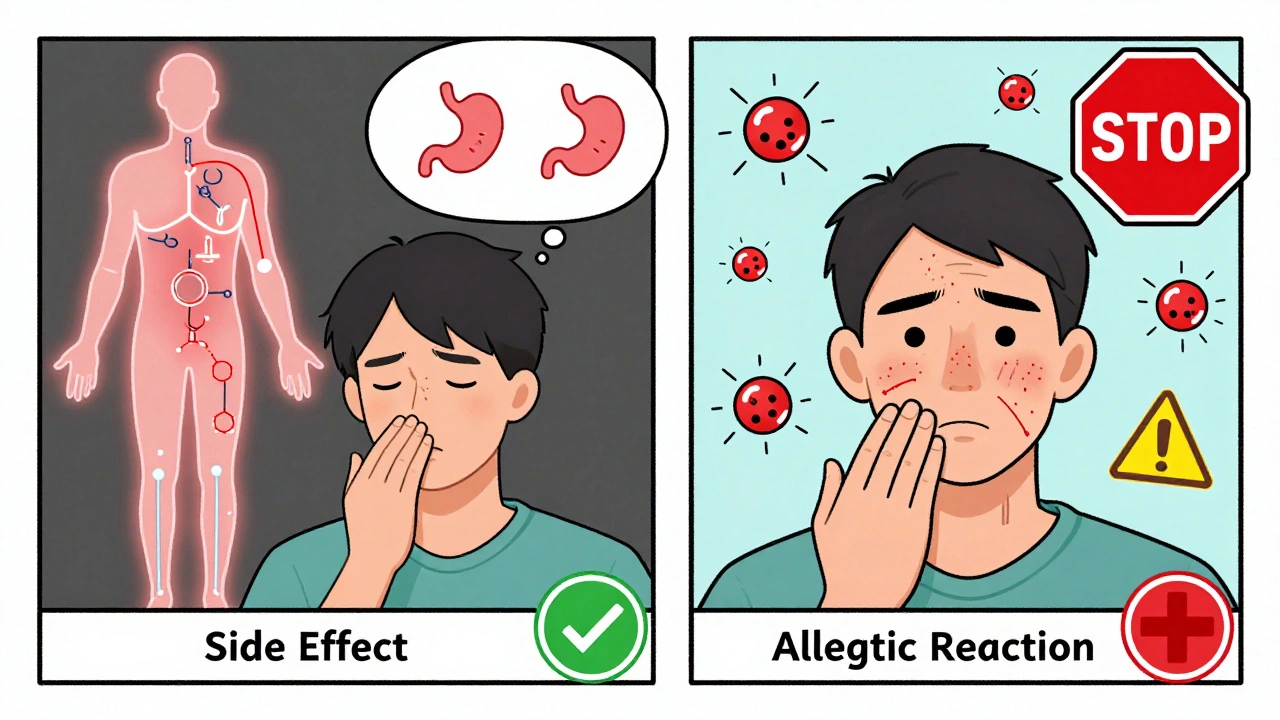
When your body treats a medicine like an invader, that’s drug hypersensitivity, an immune system overreaction to a medication that isn’t harmful to most people. Also known as medication allergy, it’s not just a rash—it can mean trouble breathing, swelling, or even organ failure. Unlike side effects, which are predictable and dose-related, drug hypersensitivity is unpredictable. One person takes amoxicillin and feels fine. Another breaks out in hives within minutes. There’s no way to know ahead of time who’s at risk—until it happens.
This isn’t rare. Studies show up to 10% of people report some kind of reaction to drugs, and antibiotics like penicillin, sulfa drugs, and NSAIDs like ibuprofen top the list. But it’s not just antibiotics. Even common painkillers, antiseizure meds, and chemotherapy drugs can trigger it. The allergic drug reaction, a specific type of immune response triggered by medication exposure often shows up as a skin rash, fever, or swollen lymph nodes. But the worst cases—like Stevens-Johnson syndrome or anaphylaxis—can be deadly if not caught fast.
What makes it worse is that many people mistake a drug hypersensitivity for something harmless. A mild rash after taking amoxicillin? They think it’s just a virus. But if you’ve had one reaction, your risk goes up next time—even with a different drug in the same class. And doctors don’t always ask the right questions. Did you get sick after that last antibiotic? Did your face swell? Did you feel like you couldn’t breathe? These aren’t just details—they’re lifesaving clues.
Some people carry epinephrine pens because they’ve had a severe reaction before. Others learn to avoid entire drug families—like all sulfa-based meds—after one bad experience. The adverse drug reaction, any harmful or unintended effect caused by a medication, including hypersensitivity can show up hours or even weeks after starting a drug. That delay makes it easy to miss the connection. But if you’ve ever had unexplained itching, blistering skin, or joint pain after starting a new pill, you need to connect those dots.
And it’s not just about stopping the drug. Knowing what to take instead matters too. If you’re allergic to one NSAID, you might still be able to use another. If penicillin isn’t safe, there are alternatives. But you can’t make those choices without clear records. That’s why tracking your reactions—what you took, when, and what happened—is as important as the prescription itself.
Below, you’ll find real cases and practical advice from people who’ve been through it. You’ll learn how to spot the warning signs before it turns dangerous, which drugs are most likely to cause trouble, and how to talk to your doctor so you’re never caught off guard again. This isn’t theoretical. These are the stories that keep people alive.
Difference Between Medication Side Effects and Allergic Drug Reactions
- Robin Tudge
- December 3, 2025
- 8 Comments
Learn the key differences between medication side effects and true allergic drug reactions. Discover why mislabeling side effects as allergies leads to unnecessary risks, higher costs, and worse health outcomes.
read more