Differences in Medications: Why Generic, Brand, and Alternatives Matter
When you hear differences, the variations between how drugs are made, priced, and regulated. Also known as drug variability, it's not just about price—it's about what’s inside the pill, who made it, and how your body reacts. Many people assume a generic drug is just a cheaper copy of the brand name. But the truth is more complicated. Some generics work just as well. Others? They cause unexpected side effects, interact badly with other meds, or don’t dissolve the same way. These aren’t minor details. They’re the difference between feeling better and ending up in the hospital.
Take generic drugs, lower-cost versions of brand-name medications approved by the FDA. Also known as therapeutic equivalents, they’re supposed to be identical in active ingredients. But quality control varies wildly. A 2023 FDA inspection found certain Indian-made generics for high-blood-pressure and seizure meds had inconsistent dissolution rates—meaning the drug didn’t release properly in your body. That’s not a theory. That’s a documented risk. Meanwhile, brand drugs, originally developed medications protected by patents. Also known as innovator drugs, they’re often more expensive but come with tighter manufacturing standards. Then there are authorized generics, exact copies of brand drugs sold under a different label by the same company. Also known as same-drug, lower-price versions, they’re the best of both worlds—same formula, no markup. And don’t forget drug interactions, when one medication changes how another works in your body. Also known as medication conflicts, they’re behind many avoidable emergencies. Like mixing PDE5 inhibitors with nitrates, or iron with thyroid meds. These aren’t rare. They’re common—and often missed.
Why these differences actually affect your health
It’s not just about cost. It’s about control. When you switch from a brand to a generic, your body might react differently—even if the active ingredient is the same. Fillers, binders, and coatings change between manufacturers. For people with sensitive stomachs, allergies, or chronic conditions like epilepsy or thyroid disease, that tiny difference can mean the difference between stability and crisis. Fluoroquinolones? They can cause permanent nerve damage. Trimethoprim? It can spike your potassium to dangerous levels. These aren’t side effects you can ignore. They’re red flags tied directly to the specific drug formulation and your personal health profile.
And then there’s the confusion. One generic costs $4. Another for the same drug costs $80. Why? Because not all generics are created equal. Some are made by reputable labs. Others? They’re produced in facilities with poor inspection records. Clinicians are starting to notice patterns—higher failure rates, more hospital visits—linked to certain batches. Transparency is low. You’re often left guessing. That’s why knowing the differences isn’t just smart. It’s necessary.
Below, you’ll find real stories, hard data, and clear comparisons about what changes when you switch meds. From how Budez CR stacks up against other inhalers, to why Paxlovid beats Molnupiravir for most people, to how timing your iron pills can make or break your thyroid treatment. These aren’t theory pieces. They’re practical guides written by people who’ve seen the fallout when differences are ignored. You don’t need to be a doctor to understand them. You just need to know what to look for.
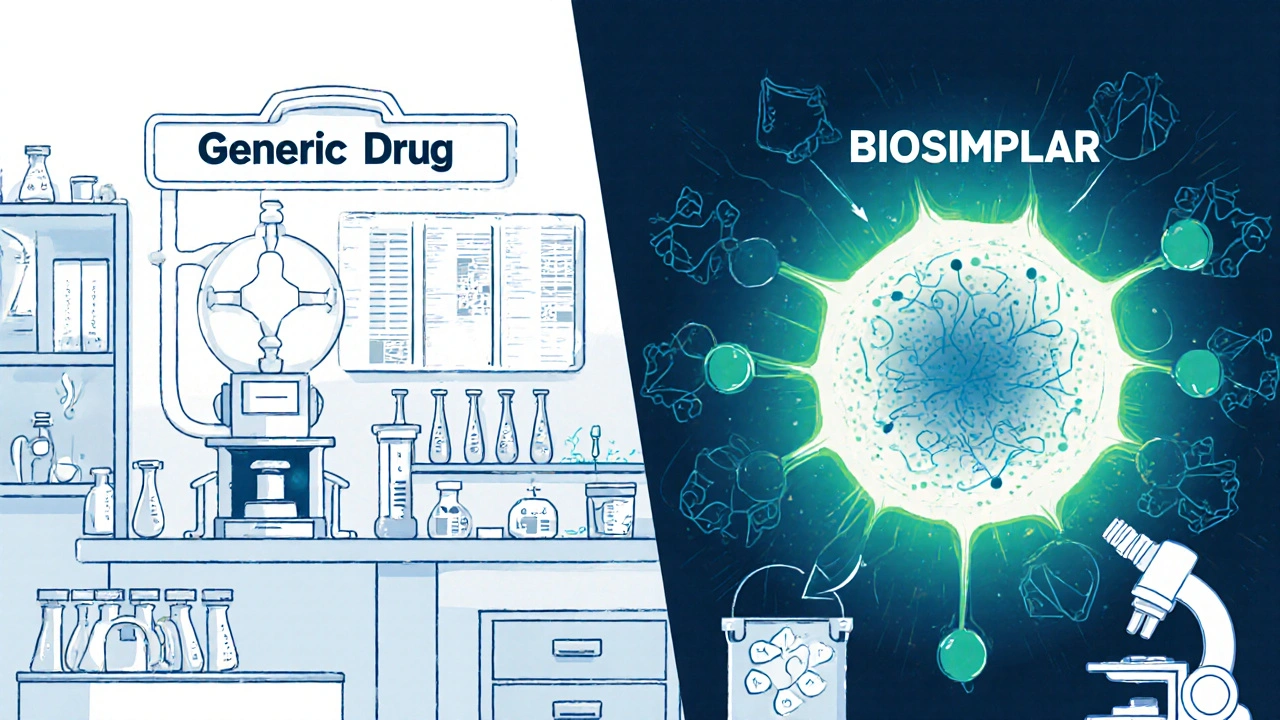
Biosimilars vs Generics: Key Differences Explained
- Robin Tudge
- November 24, 2025
- 13 Comments
Biosimilars and generics both lower drug costs, but they’re not the same. Biosimilars are complex biologic copies with stricter rules, while generics are simple chemical copies. Understand the key differences in safety, cost, and substitution.
read more