Bioequivalence Waivers: When Generic Drugs Don't Need Testing
When a generic drug company wants to sell a copy of a brand-name medicine, the bioequivalence waiver, a regulatory shortcut that allows certain generic drugs to be approved without conducting full bioequivalence studies. Also known as biowaiver, it’s a rule that saves time, money, and resources—without putting patient safety at risk. This isn’t a loophole. It’s a science-backed exception built into the FDA’s approval system for drugs that behave predictably in the body.
Not every generic drug qualifies. Bioequivalence studies, clinical tests that compare how quickly and completely a generic drug enters the bloodstream versus the brand-name version are the gold standard. But if a drug is highly soluble, rapidly absorbed, and has a wide safety margin, the FDA says: skip the tests. These are usually oral tablets or capsules made with simple chemical structures. Think of common drugs like metformin, lisinopril, or amoxicillin—small molecules that don’t change much from one manufacturer to another. For these, the body doesn’t care if it’s made in Indiana or India, as long as the ingredients match.
That’s where regulatory science, the field that uses data and modeling to support drug approval decisions without always requiring human trials comes in. The FDA uses things like solubility data, dissolution profiles, and pharmacokinetic models to predict whether a drug will act the same way. If the numbers line up, they grant a waiver. This keeps prices low and supply stable. It’s why you can buy a $4 generic version of a drug that used to cost $400.
But here’s the catch: waivers only apply to a narrow set of drugs. Complex ones—like extended-release pills, suspensions, or biologics—still need full testing. That’s why you’ll see FDA requirements, the strict standards generic manufacturers must meet to prove their product is safe and effective vary from one drug to the next. A waiver isn’t a free pass. It’s a smart filter. The FDA doesn’t cut corners—they just skip the steps that don’t add value.
And it’s not just about cost. When bioequivalence waivers work right, they keep essential medicines available. During drug shortages, this process lets new manufacturers jump in fast. It’s why you didn’t run out of your blood pressure pill when the original maker had a factory issue. Waivers keep the system moving.
Some people worry that skipping tests means lower quality. But the data doesn’t back that up. The FDA has tracked thousands of waived generics over decades. Side effect rates? No difference. Treatment success? Just as good. What changes is the price tag—not the outcome.
What you’ll find in the posts below are real-world examples of how this system works—or sometimes, how it doesn’t. From cases where generic manufacturers got it right, to situations where quality concerns popped up despite a waiver, to how the FDA updates its rules based on new science. You’ll see how bioequivalence waivers connect to everything from drug pricing to patient safety to global manufacturing. No fluff. Just facts that help you understand why your generic works—and when you should ask questions.
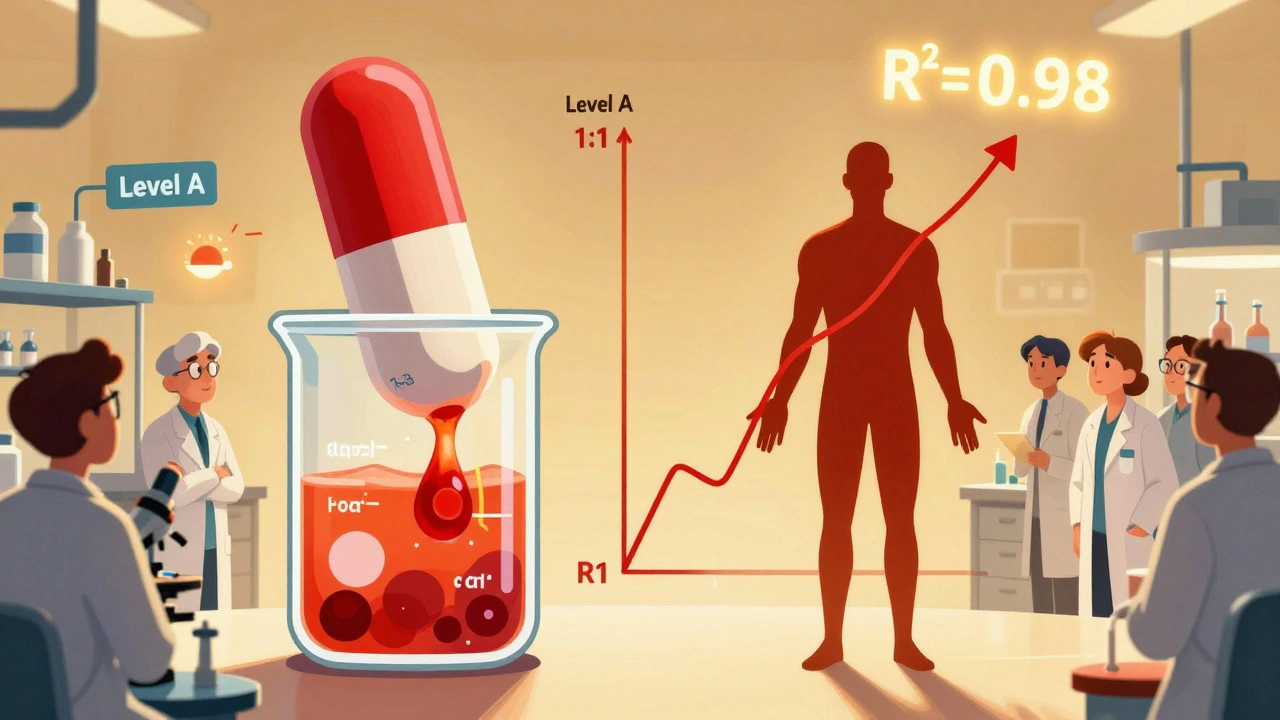
IVIVC and Waivers: How In Vitro Methods Are Replacing In Vivo Bioequivalence Testing
- Robin Tudge
- December 6, 2025
- 15 Comments
IVIVC lets generic drug makers replace costly human bioequivalence tests with lab-based dissolution data. Learn how Level A correlations work, why most submissions fail, and how biorelevant methods are changing the game.
read more