How to Clean a Wound Properly
Most people think cleaning a wound is as simple as rinsing it with water. But how you clean it matters more than you think. Using the wrong product can actually slow healing and increase your risk of infection.
The best way to clean a minor cut, scrape, or puncture is with cool running water. Hold the wound under the faucet for 5 to 10 minutes. This flushes out dirt, bacteria, and debris without damaging the delicate tissue. Studies show this simple step reduces infection risk by 40% compared to just dabbing or soaking the wound.
Don’t use hydrogen peroxide or rubbing alcohol. Even though they’re common in medicine cabinets, they kill healthy cells along with germs. This delays healing by up to 50%. The same goes for iodine solutions-too harsh for open skin.
For the skin around the wound, use mild soap and water. Gently wash the area, then rinse thoroughly. Avoid getting soap inside the wound. If there’s visible debris like gravel or glass, use clean tweezers to remove it. Wipe the tweezers with alcohol first to avoid introducing new bacteria.
Pressure matters too. You need enough force to flush out contaminants, but not so much that you tear the wound. Aim for 8 to 15 pounds per square inch (psi). That’s about the pressure of a gentle stream from a kitchen faucet. Too weak? You won’t clean well. Too strong? You risk more damage.
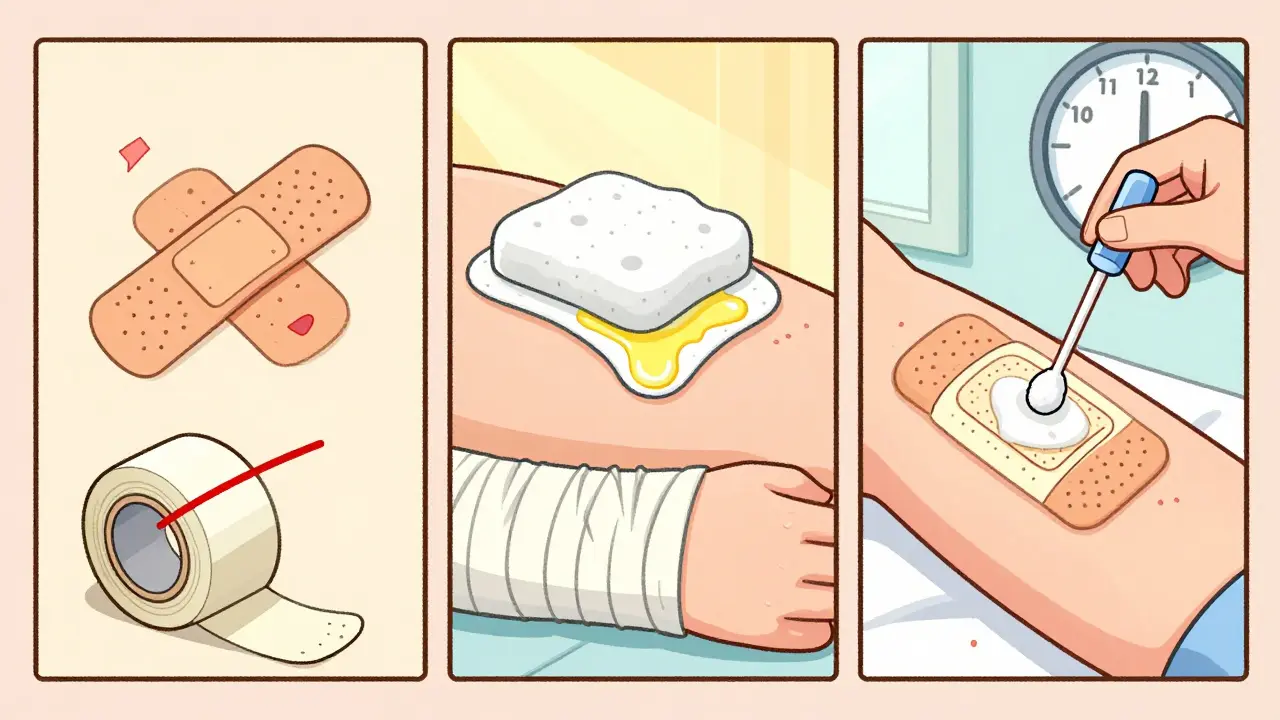
Choosing the Right Dressing
Once the wound is clean, it needs protection. But not just any bandage will do. The type of dressing depends on how much fluid the wound is producing.
For small, dry cuts or scrapes, a simple adhesive bandage works fine. But if the wound is weeping, you need something more absorbent. Foam dressings and alginate pads are designed to soak up excess fluid without sticking to the wound bed. These are ideal for larger abrasions or surgical incisions.
For shallow wounds with little drainage, hydrocolloid dressings are a top choice. They create a moist environment that speeds healing and reduces pain. You can leave them on for several days, which means fewer changes and less irritation.
Never wrap tape completely around an arm or leg. That can cut off circulation and cause serious damage. Instead, use gauze and secure it with paper tape or a stretchy bandage that allows movement.
Change dressings daily-or sooner if they get wet or dirty. Wet-to-dry dressings (where gauze is soaked in saline and left to dry on the wound) are outdated. They rip away new tissue when removed, causing pain and delaying healing. Modern dressings keep things moist, not dry.
Apply a thin layer of petroleum jelly or plain antibiotic ointment like bacitracin before putting on the dressing. This keeps the wound from sticking and supports natural healing. But here’s a twist: some experts say petroleum jelly alone works just as well as antibiotic ointments, with fewer chances of allergic reactions.
Preventing Scars Before They Start
Scars aren’t inevitable. How you care for a wound in the first few weeks determines how noticeable the scar will be.
Keep the wound moist. Dry skin forms thicker, darker scars. Applying petroleum jelly or an ointment twice a day helps the skin heal smoothly. Studies show this simple habit cuts scar formation by 60%.
After the wound closes-usually around day 14-start using silicone gel or sheets. These are clinically proven to reduce raised, red scars by 50 to 60%. They work by regulating moisture and pressure on the healing skin. You can find them over the counter at any pharmacy.
Protect the area from the sun. New skin is extra sensitive to UV rays. Exposure can cause permanent darkening, making scars look worse. Use SPF 30+ sunscreen every day, even if it’s cloudy. Keep it on for at least 12 months after the injury. Dermatologists see this as non-negotiable.
Don’t pick at scabs. Let them fall off naturally. Pulling them off forces the skin to heal again, which increases scarring. And avoid tight clothing over healing wounds-it puts pressure on the tissue and can lead to thick, ropey scars.
When to Call a Doctor
Most minor wounds heal fine on their own. But some need professional care. Watch for these red flags:
- Redness spreading more than one inch from the wound edge
- Pus or thick yellow/green drainage
- Fever above 100.4°F (38°C)
- Wound isn’t improving after 7 days
- Deep cuts longer than 0.25 inches or deeper than 0.125 inches
- Wounds on joints, hands, or face that won’t stay closed
These signs suggest infection or tissue damage that needs antibiotics or stitches. Delaying treatment can lead to serious complications, especially for people with diabetes or poor circulation.
Diabetic wounds are a special case. Even a small blister can turn into a foot ulcer. If you have diabetes, check your feet daily and get any wound evaluated by a doctor within 24 hours.
What to Avoid
There are a lot of myths about wound care. Here’s what not to do:
- Don’t use butter, toothpaste, or baking soda on wounds. These can trap bacteria and cause infection.
- Don’t pop blisters. They protect the skin underneath. Breaking them raises infection risk by 35%.
- Don’t reuse old bandages or dirty tweezers. Always clean tools before touching the wound.
- Don’t ignore dehydration. Drink at least half an ounce of water per pound of body weight each day. Being dehydrated can stretch healing time by 25 to 30%.
- Don’t skip handwashing. Wash your hands with soap for 20 seconds before and after touching the wound. Use hand sanitizer with at least 60% alcohol if soap isn’t available.

Special Cases: Burns and Pressure Wounds
Burns need different handling. For minor burns, run cool (not ice-cold) water over the area for 10 to 15 minutes. Never apply ice directly-it can freeze the tissue. Leave blisters intact. Cover with a sterile, nonstick dressing.
Pressure wounds, common in people who sit or lie in one position for long periods, need frequent repositioning. Turn every two hours. Use pillows to lift heels off the bed and keep pressure off bony areas. The National Pressure Injury Advisory Panel says this reduces new pressure sores by 65%.
The Bigger Picture
Wound care isn’t just about bandaids. It’s a system. Clean properly, dress smartly, protect from sun, stay hydrated, and watch for warning signs. Done right, you reduce infection risk from 10-15% down to 2-5%. Healing time drops by 30-50%. Scars become barely noticeable.
Chronic wounds affect 6.5 million Americans each year and cost over $25 billion. But most are preventable. The most powerful tool? Simple, consistent care.


All Comments
Ryan Riesterer January 21, 2026
The 8-15 psi pressure recommendation is clinically sound. Studies from the Journal of Wound Care (2021) corroborate that suboptimal irrigation pressure correlates with residual biofilm formation. Most home faucets deliver 20-40 psi-so adjusting flow via aerator or partial valve closure is necessary. Don’t assume ‘gentle stream’ equals therapeutic.
Also, hydrocolloids outperform gauze in moisture retention metrics (pH 5.5-6.5 microenvironment). Avoid saline-soaked dressings-they’re a relic of 1980s protocol.
Mike P January 22, 2026
LMAO people still use hydrogen peroxide? Bro, that stuff is for cleaning your garage floor, not your skin. I saw my cousin put it on a cut and she screamed like she got stabbed. And don’t even get me started on butter on burns-what is this, 1953? We got science now. Stop listening to your grandma’s advice and read a damn article.
Sarvesh CK January 22, 2026
The philosophical underpinning of wound care lies not merely in antiseptic protocols, but in the recognition of the body’s innate regenerative intelligence. To interfere with this process through excessive mechanical disruption or chemical aggression is to impose an anthropocentric bias upon biological autonomy. The moist wound environment, therefore, is not merely a clinical preference-it is an alignment with the organism’s evolutionary design. One might even say, in a metaphysical sense, that healing is not something we do to the body, but something we facilitate within it.
Daphne Mallari - Tolentino January 22, 2026
I’m surprised this article didn’t cite the 2023 Cochrane Review on silicone gel efficacy. Also, petroleum jelly is hardly a ‘twist’-it’s been standard since the 1940s. The fact that this is still being presented as novel suggests a concerning gap in medical literacy among the general public. And ‘SPF 30+ for 12 months’? That’s barely adequate. I’d recommend SPF 50+ with UVA-PF rating ≥ 20 for optimal photoprotection.
Neil Ellis January 24, 2026
This is the kind of info that turns a scratch into a story. You know what’s wild? When you treat a wound like it’s a baby-gentle, warm, patient-it actually rewards you. No drama. No drama scars. Just smooth, quiet skin that looks like it never even cried. And hydration? Oh honey, your skin is thirsty. Drink up like your life depends on it… because it kinda does.
Rob Sims January 25, 2026
So let me get this straight. You’re telling me the entire medical establishment spent 50 years getting wound care wrong, and now we’re just learning not to use peroxide? I’ve seen people use superglue on cuts. At least that’s faster than waiting for a ‘gentle stream’.
arun mehta January 25, 2026
I appreciate the science here 🙏. In India, we’ve long used turmeric paste on minor wounds-antimicrobial, anti-inflammatory, and culturally rooted. But modern evidence supports the same principle: keep it clean, keep it moist. Let’s blend tradition with data. No need to reject either. 🌿✨
Lauren Wall January 26, 2026
Don’t use butter. Seriously? Who even does that?
Kenji Gaerlan January 27, 2026
bro why is this so long like i just cut my finger on a chip bag 🤡
Tatiana Bandurina January 28, 2026
The article implies dehydration delays healing by 25-30%. That’s a gross oversimplification. No controlled study has isolated hydration as a primary variable in cutaneous repair. This is pseudoscientific fluff dressed as evidence. Also, ‘half an ounce per pound’? That’s over 100 oz for a 150-lb person. Hyponatremia risk increases with that kind of recommendation.