Steroid-Induced Diabetes: Causes, Risks, and How to Manage It
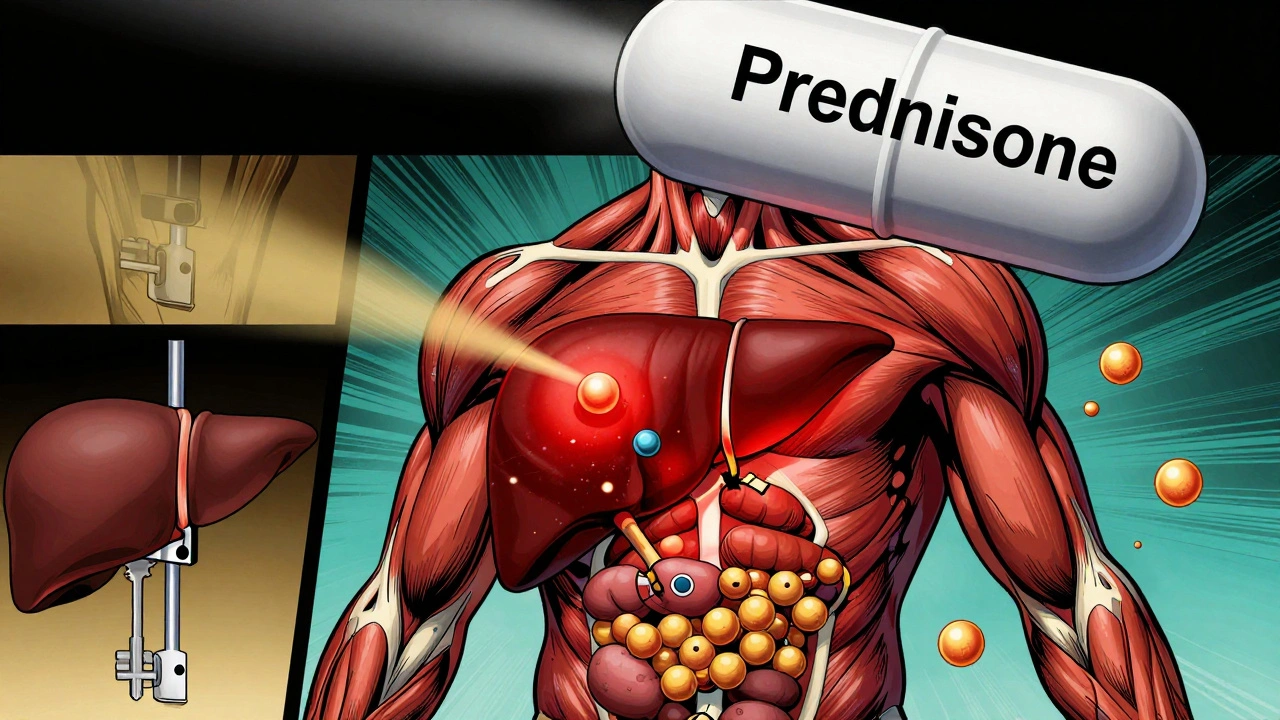
When you take steroid-induced diabetes, a temporary form of high blood sugar triggered by corticosteroid medications. Also known as glucocorticoid-induced hyperglycemia, it’s not the same as type 2 diabetes—but it can feel just as scary if you’re not prepared. This isn’t rare. People on long-term corticosteroids, drugs like prednisone, methylprednisolone, or dexamethasone used for inflammation, asthma, or autoimmune conditions often see their blood sugar climb. It’s not a mistake. It’s a known side effect—so why do so many patients get caught off guard?
Insulin resistance, when your body stops responding well to insulin is the main driver. Steroids tell your liver to dump more glucose into your bloodstream while blocking insulin from doing its job. Your pancreas tries to keep up, but eventually, it can’t. That’s when your numbers jump—sometimes overnight. You might not feel anything at first. No thirst, no frequent urination. But your fasting glucose? It’s up. Your HbA1c? Rising. And if you’re already prediabetic, overweight, or over 45? Your risk shoots up.
This isn’t just about pills and numbers. It’s about real life. Someone on steroids for rheumatoid arthritis might start gaining weight, feeling tired all the time, or needing to wake up at night to pee. A kid with severe asthma on daily prednisone might crash after school because their sugar dropped too low after a spike. These aren’t coincidences. They’re direct results of how these drugs mess with your metabolism.
Here’s the good news: steroid-induced diabetes often reverses when you stop the meds. But while you’re on them, you need a plan. Monitoring your blood sugar at home isn’t optional—it’s essential. Eating fewer refined carbs helps. Moving your body—even a short walk after meals—can lower spikes. And if your doctor prescribes metformin or insulin temporarily? That’s not a failure. It’s smart management.
You’ll find posts here that break down how drug side effects, like those from corticosteroids can sneak up on you. Others show how to spot the difference between a normal reaction and something dangerous. You’ll see how people track these changes, what tests matter, and how to talk to your doctor without sounding alarmist. There’s no sugarcoating this—steroids can wreck your blood sugar. But with the right info, you’re not helpless. You’re prepared.
Corticosteroids and Diabetes: How Steroids Cause High Blood Sugar and How to Manage It
- Robin Tudge
- December 1, 2025
- 10 Comments
Corticosteroids like prednisone can cause dangerous spikes in blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who's most at risk, and how to manage it safely with insulin and monitoring.
read more