Prednisone: What It Is, How It Works, and What You Need to Know
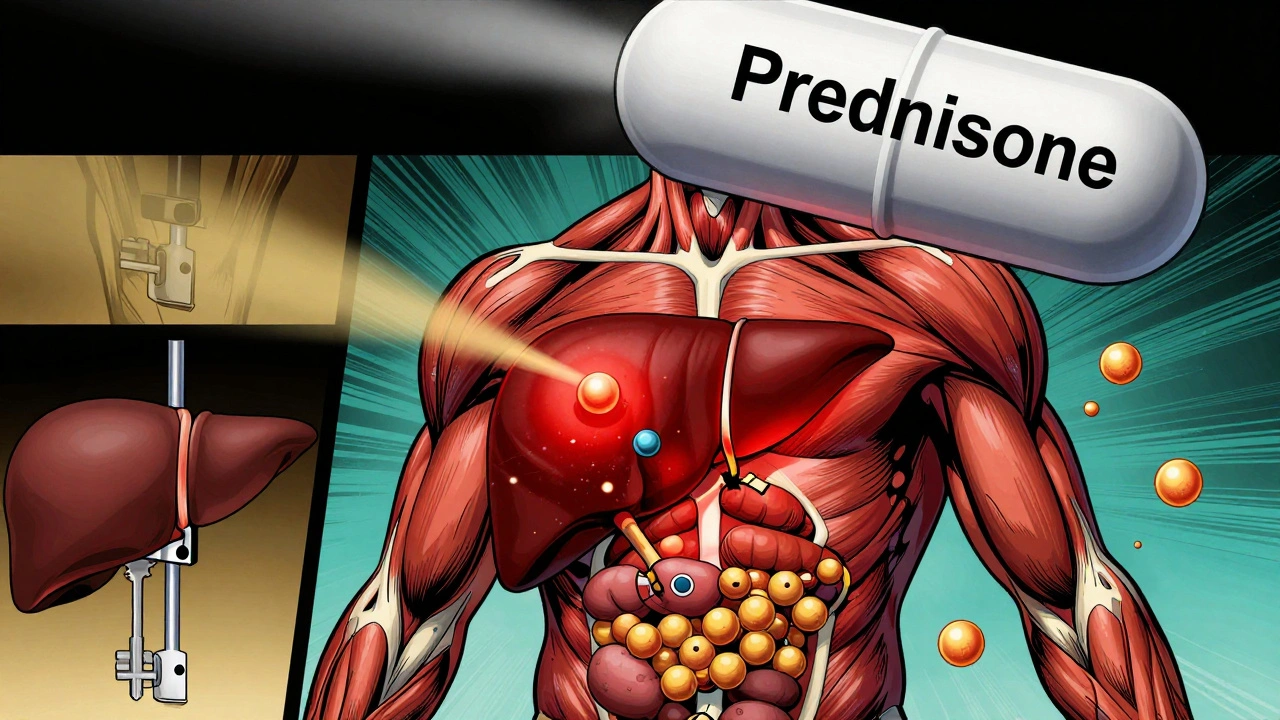
When you hear prednisone, a synthetic corticosteroid used to calm inflammation and shut down overactive immune responses. Also known as a steroid pill, it’s one of the most commonly prescribed drugs for conditions ranging from asthma to rheumatoid arthritis — but it’s not harmless. Unlike painkillers that just mask symptoms, prednisone changes how your body reacts to injury, infection, or autoimmune attacks. It doesn’t cure anything. It just turns down the noise your immune system makes when it’s gone rogue.
People take prednisone for many reasons. If you’ve been told you have inflammation, the body’s natural response to injury or illness that can become chronic and damaging in your lungs, joints, or skin, your doctor might reach for prednisone. It’s also used in immune suppression, the intentional weakening of the body’s defense system to treat autoimmune diseases or prevent organ rejection after transplants. But here’s the catch: the longer you take it, the more your body forgets how to run itself. Your adrenal glands slow down. Your bones thin. Your blood sugar climbs. And if you stop too fast, your body can crash.
Many patients don’t realize prednisone isn’t meant for long-term use. Yet it’s often prescribed for months or even years because alternatives are expensive, complex, or not covered by insurance. That’s why so many posts here talk about steroid side effects — weight gain, mood swings, cataracts, diabetes, and weakened muscles. One patient took it for a year after a severe asthma flare-up and ended up with osteoporosis. Another developed a fungal infection because their immune system was too quiet. These aren’t rare outcomes. They’re predictable.
There are smarter ways to manage chronic conditions now. Biologics, inhaled steroids, and targeted therapies can often replace oral prednisone — especially for asthma, lupus, or inflammatory bowel disease. But switching isn’t always easy. Cost, access, and doctor habits keep prednisone on the shelf. That’s why understanding how it works — and when to push back — matters more than ever.
Below, you’ll find real stories and science-backed advice on how prednisone affects your body, how to spot dangerous reactions, what to do if you’re stuck on it long-term, and how to reduce your reliance on it safely. Some posts compare it to other steroids. Others warn about interactions with common drugs like blood pressure pills or antibiotics. One even explains how patients use social media to track side effects no clinical trial ever caught. This isn’t theory. It’s what people are living — and surviving — every day.
Corticosteroids and Diabetes: How Steroids Cause High Blood Sugar and How to Manage It
- Robin Tudge
- December 1, 2025
- 10 Comments
Corticosteroids like prednisone can cause dangerous spikes in blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who's most at risk, and how to manage it safely with insulin and monitoring.
read more