Oral Contraceptives – Your Quick‑Start Guide
When talking about oral contraceptives, a class of medication taken by mouth to prevent pregnancy through hormone manipulation. Also known as birth control pills, they blend synthetic estrogen and/or progestin to stop ovulation, thicken cervical mucus, and thin the uterine lining. This simple definition sets the stage for why millions rely on them every day.
Core Types and How They Differ
Two main combined oral contraceptives, packets that contain both estrogen (typically ethinyl estradiol) and a progestin dominate the market. The estrogen component suppresses the pituitary release of follicle‑stimulating hormone, while the progestin blocks the luteinizing hormone surge that triggers ovulation. In contrast, progestin‑only pills, sometimes called mini‑pills, rely solely on a synthetic progestin to thicken cervical mucus and alter the endometrium. Both types fulfill the same primary goal—preventing fertilization—but their side‑effect profiles and suitability for different health conditions vary.
Understanding the hormone regulation, the balance of estrogen and progestin that drives the menstrual cycle is crucial. Oral contraceptives essentially reset this balance, which can lead to lighter periods, reduced cramping, and fewer acne breakouts. However, the same hormonal shift can cause weight changes, mood swings, or breast tenderness in some users. Knowing that "oral contraceptives influence menstrual cycle dynamics" helps you anticipate what to expect and when to seek medical advice.
Another key entity is the menstrual cycle, the monthly hormonal rhythm preparing the uterus for possible pregnancy. By delivering steady levels of synthetic hormones, oral contraceptives flatten the natural peaks and troughs that cause the typical 28‑day cycle. This flattening can be therapeutic for conditions like endometriosis or polycystic ovary syndrome, where irregular hormone spikes exacerbate pain. In practice, many patients report that their "periods become more predictable and less painful" once they start a reliable birth control regimen.
Drug interactions represent a practical concern. Certain antibiotics, anticonvulsants, and herbal supplements (like St. John’s wort) can induce liver enzymes that speed up hormone metabolism, potentially reducing pill efficacy. That’s why clinicians advise a backup contraception method when starting or stopping these interacting drugs. This relationship—"oral contraceptives require careful monitoring for drug interactions"—highlights the importance of open communication with healthcare providers.
Beyond pregnancy prevention, oral contraceptives have secondary benefits. They can lower the risk of ovarian and endometrial cancers, improve acne, and even help manage hirsutism. On the flip side, rare but serious risks include blood clots, especially in smokers over 35 or those with clotting disorders. The balance of benefit versus risk is why many articles in this collection discuss safety tips, side‑effect management, and personalized pill selection.
Below, you’ll find a curated set of articles that dive into specific scenarios—whether you’re curious about weight gain linked to progesterone, looking for ways to ease menstrual bladder pain, or need a clear comparison of hormone‑based medications. Each post adds a piece to the larger puzzle of how oral contraceptives fit into everyday health decisions. Let’s explore the practical insights and evidence‑based tips that can help you choose the right pill, stay safe, and feel confident about your contraception choice.
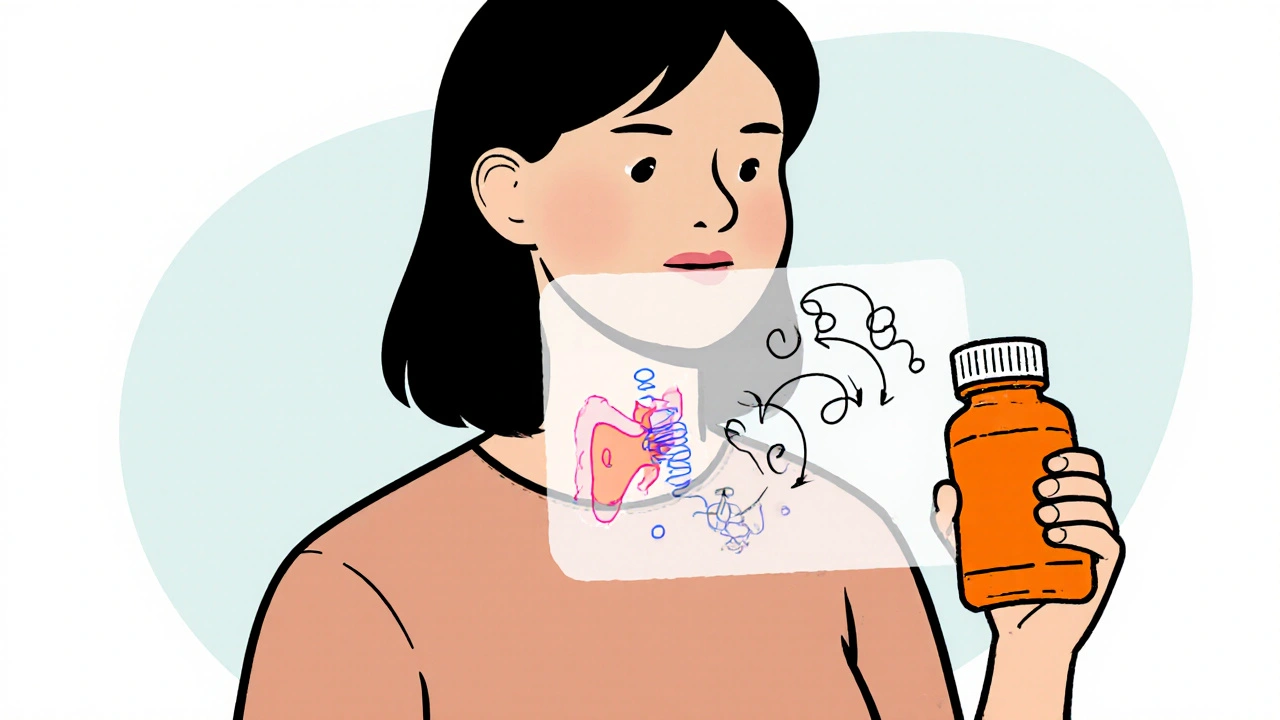
How Ethinylestradiol Impacts Thyroid Function - Risks, Mechanisms & Guidance
- Robin Tudge
- October 23, 2025
- 15 Comments
Discover how ethinylestradiol in birth‑control pills can alter thyroid hormone levels, affect test results, and what steps you can take to stay balanced.
read more