Corticosteroids: What They Are, How They Work, and Safer Alternatives
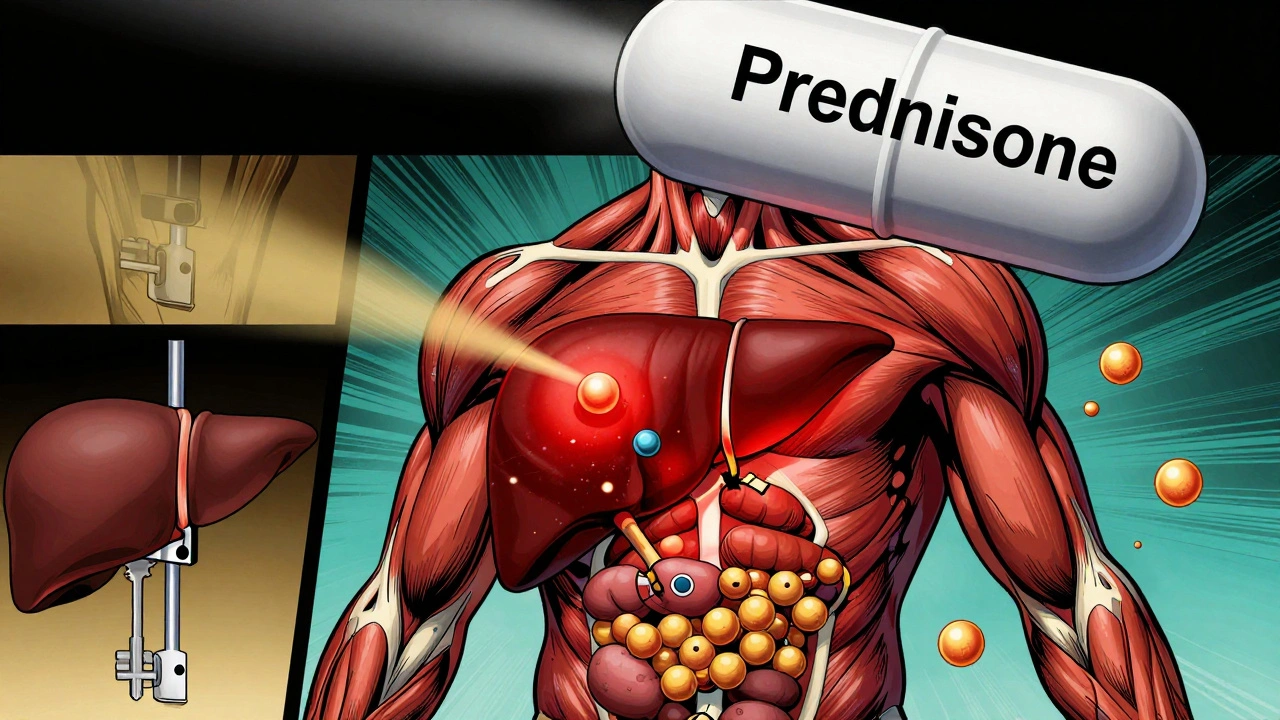
When your body’s immune system goes into overdrive—whether from asthma, arthritis, or an autoimmune flare—corticosteroids, a class of powerful anti-inflammatory drugs that mimic natural hormones produced by your adrenal glands. Also known as steroids, they’re one of the most effective tools doctors have to calm dangerous inflammation fast. But using them for more than a few weeks can turn them from lifesavers into health risks.
That’s why oral corticosteroids, daily pills like prednisone used to manage chronic conditions are now being replaced wherever possible. Long-term use can lead to weight gain, bone loss, high blood sugar, cataracts, and even weakened immune defenses. A 2023 study showed patients on daily steroids for over six months had a 40% higher risk of fractures and serious infections. For people with severe asthma, a chronic lung condition where airways swell and narrow, triggering wheezing and breathlessness, the reliance on these pills has been a silent epidemic—until now.
The game is changing. New treatments called biologics, targeted therapies that block specific parts of the immune system causing inflammation are giving patients a way to control flare-ups without the side effects of daily steroids. Drugs like omalizumab and mepolizumab don’t just reduce attacks—they cut hospital visits and steroid use by half in many cases. This isn’t theory. Real patients are breathing easier, sleeping better, and avoiding the weight gain and mood swings that come with long-term steroid use.
But corticosteroids aren’t going away. They’re still essential for sudden flare-ups, allergic reactions, or when biologics aren’t an option. The key is knowing when to use them, how long to use them, and when to switch. If you’ve been on steroids for months, you’re not alone—and there’s a better path ahead. Below, you’ll find real-world guides on steroid risks, how biologics compare, and how to talk to your doctor about reducing your dependence. No fluff. Just what works.
Corticosteroids and Diabetes: How Steroids Cause High Blood Sugar and How to Manage It
- Robin Tudge
- December 1, 2025
- 10 Comments
Corticosteroids like prednisone can cause dangerous spikes in blood sugar, even in people without diabetes. Learn how steroids trigger hyperglycemia, who's most at risk, and how to manage it safely with insulin and monitoring.
read more