Antibiotic Side Effects: What You Need to Know Before Taking Them
When you take an antibiotic, a medication designed to kill or slow the growth of bacteria. Also known as antibacterial agents, they’re one of the most common drugs prescribed worldwide — but they’re not harmless. Even when they work, they can cause real, sometimes serious, side effects that many people don’t expect. Not all antibiotics are the same. Some, like chloramphenicol, a broad-spectrum antibiotic linked to rare but fatal bone marrow damage, are rarely used today because safer options exist. Others, like amoxicillin or azithromycin, are common and generally well-tolerated — but still carry risks like diarrhea, yeast infections, or allergic reactions. The truth is, every antibiotic has a profile of possible side effects, and knowing which ones matter most can help you avoid unnecessary harm.
Antibiotic side effects don’t just happen because of the drug itself — they’re often tied to how you take it, what else you’re on, and even your age or health history. For example, mixing antibiotics with certain painkillers, supplements, or even grapefruit juice can change how your body handles them. Some people develop drug interactions, harmful reactions when two or more medications affect each other’s function that lead to kidney stress, liver damage, or dangerous drops in blood pressure. And if you’ve ever been told to finish your full course of antibiotics, that advice isn’t just about stopping infection — it’s also about preventing resistant strains that make future treatments harder. Meanwhile, overuse has led to a rise in antibiotic alternatives, like targeted therapies or probiotics, that aim to reduce reliance on broad-spectrum drugs. These aren’t magic fixes, but they’re part of a smarter approach to infection care.
You might think generic antibiotics are just cheaper versions of brand names — and sometimes they are. But recent data shows some low-cost generics, especially those made overseas, have higher rates of contamination or inconsistent potency. That doesn’t mean all generics are risky — many are perfectly safe — but it does mean you should pay attention to where your pills come from and whether your doctor or pharmacist stands behind the source. The antibiotic side effects you experience could be worse if the drug isn’t manufactured to proper standards. What’s more, some side effects show up days or weeks after you stop taking the pill — like Clostridioides difficile infection, which causes severe, recurring diarrhea. Others, like tendon rupture from fluoroquinolones, can strike even in healthy young adults. The goal isn’t to scare you off antibiotics — they save lives. But it’s to make sure you’re not taking them blindly.
Below, you’ll find real, practical guides on which antibiotics are safest, which ones to avoid unless absolutely necessary, how to spot dangerous reactions early, and what to do if you’re stuck with a prescription that feels too risky. You’ll also see how newer treatments are replacing older, more dangerous options — and how to talk to your doctor about alternatives that work just as well, without the hidden costs to your body.
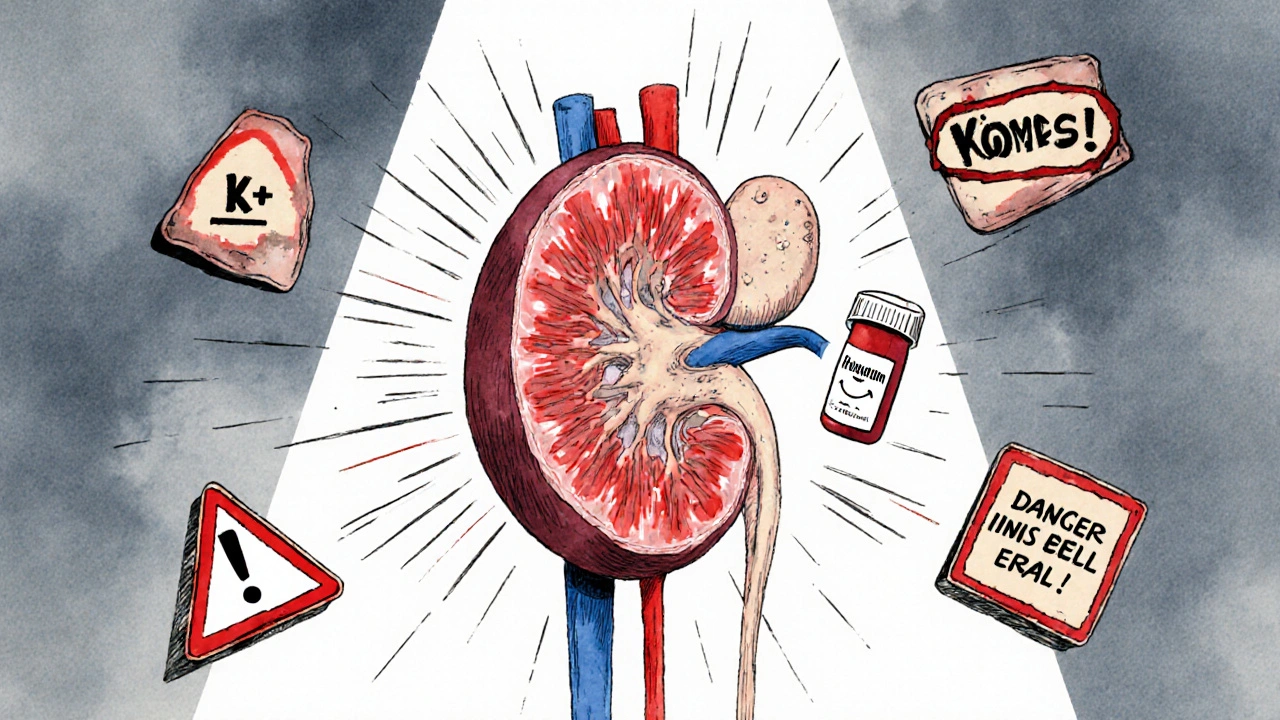
Trimethoprim and Potassium Levels: How This Common Antibiotic Can Raise Your Risk of Hyperkalemia
- Robin Tudge
- November 19, 2025
- 10 Comments
Trimethoprim, found in Bactrim, can dangerously raise potassium levels, especially in older adults and those on blood pressure meds. Learn who's at risk, how to prevent life-threatening hyperkalemia, and safer alternatives.
read more