Statin Cognitive Side Effects Comparison Tool
Compare statins based on their potential for cognitive side effects. This tool helps you understand the differences between lipophilic and hydrophilic statins and how they might affect your memory.
How Statins Affect Memory
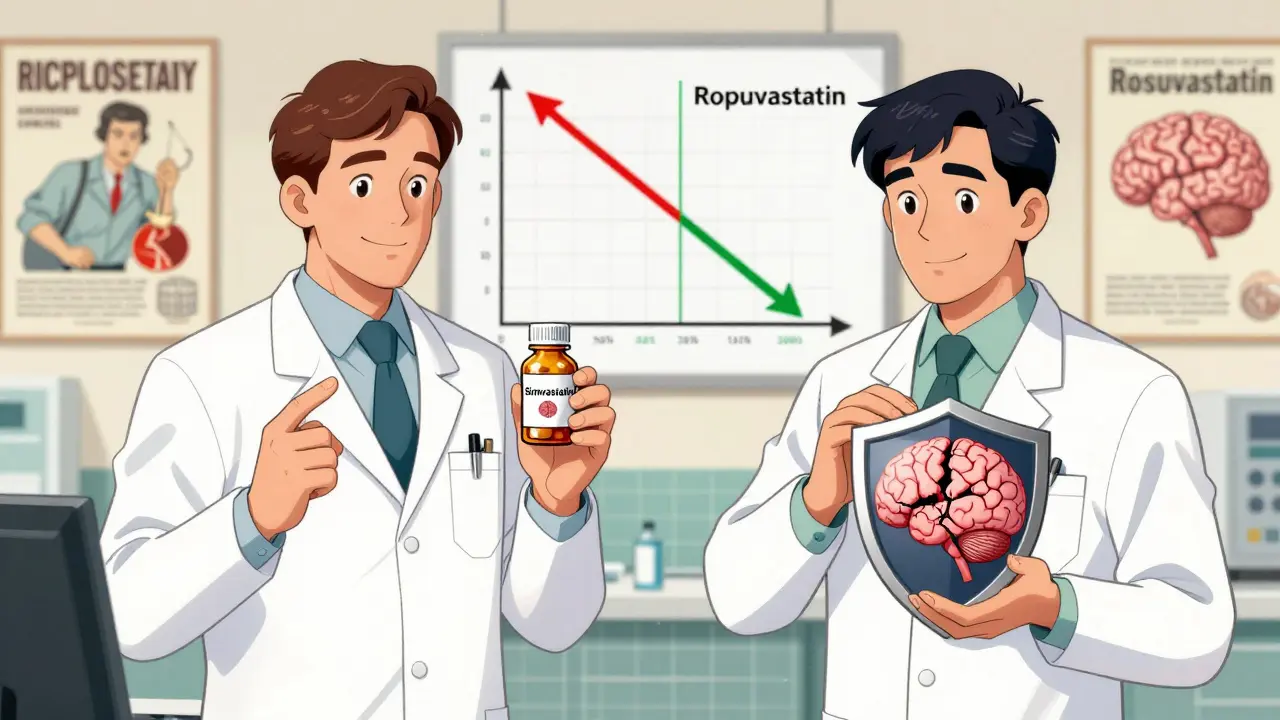
Statins can be divided into two types: lipophilic (which cross the blood-brain barrier more easily) and hydrophilic (which don't cross as easily). Lipophilic statins like simvastatin and atorvastatin are more commonly associated with memory complaints, while hydrophilic statins like pravastatin and rosuvastatin are associated with fewer cognitive issues.
The article explains that while some people experience memory problems when taking statins, these symptoms are typically temporary and reversible. If you're concerned about cognitive side effects, this tool can help you understand which statins might be better suited for you.
Compare Statins
Statin Reference Guide
Lipophilic Statins (Cross blood-brain barrier more easily)
Simvastatin: Most commonly associated with memory complaints. 1.42 times more likely to report memory issues compared to hydrophilic statins. Half-life: 2-3 hours.
Atorvastatin: Second most associated with memory complaints after simvastatin. Long half-life (up to 30 hours) means prolonged exposure to the brain. Half-life: Up to 30 hours.
Lovastatin: Lipophilic statin with moderate association with memory complaints. Half-life: 2-4 hours.
Fluvastatin: Lipophilic statin with lower risk of cognitive side effects compared to simvastatin and atorvastatin. Half-life: 1-3 hours.
Hydrophilic Statins (Less likely to cross blood-brain barrier)
Pravastatin: Hydrophilic statin that doesn't cross the blood-brain barrier easily. Lowest risk of cognitive side effects. Half-life: 1.5-2 hours.
Rosuvastatin: Hydrophilic statin that doesn't cross the blood-brain barrier easily. Very low risk of cognitive side effects. Half-life: 19 hours.
When you start taking a statin, you expect to lower your cholesterol and reduce your risk of a heart attack or stroke. You don’t expect to forget where you put your keys or struggle to remember a friend’s name. But for some people, that’s exactly what happens. Memory lapses, brain fog, confusion - these aren’t just rumors. They’re real reports backed by data, though the truth is more complicated than it sounds.
Statins and Memory: What the Data Really Shows
Statins are among the most prescribed drugs in the world. In 2023, nearly 39 million Americans took them. Their job? Block an enzyme called HMG-CoA reductase to cut down LDL (bad) cholesterol by 30% to 60%. That’s powerful. And it works. But somewhere in the early 2000s, patients started reporting memory issues. The FDA took notice and added cognitive side effects - including memory loss and confusion - to statin labels in 2012.
Here’s the twist: objective tests don’t always back up those reports. A 2020 study in the Journal of General Internal Medicine found that while 28% of statin users said they were having trouble remembering things, only 8% showed actual decline on standardized memory tests. That gap suggests something important: perception isn’t always reality. Some of this may be the nocebo effect - where expecting a side effect makes you notice it, even if it’s not there.
Still, the reports are too common to ignore. A 2015 JAMA Internal Medicine study found a 3.78-fold spike in acute memory loss within 30 days of starting a statin. But here’s the kicker: the same spike happened with non-statin cholesterol drugs. That points to detection bias - people and doctors start watching for memory issues once they know it’s a possible side effect.
Lipophilic vs. Hydrophilic: Not All Statins Are the Same
There are seven statins on the market. Not all of them behave the same way in your body. The key difference? How easily they cross the blood-brain barrier.
Lipophilic statins - like simvastatin, atorvastatin, lovastatin, and fluvastatin - are fat-soluble. That means they slip into your brain more easily. Hydrophilic statins - pravastatin and rosuvastatin - are water-soluble. They stay mostly in your bloodstream.
A 2023 analysis in the Journal of the American College of Cardiology looked at 48,732 patients across 12 trials. Those on lipophilic statins were 1.42 times more likely to report memory complaints than those on hydrophilic ones. The numbers were clear: simvastatin and atorvastatin showed the most links to cognitive reports. Pravastatin and rosuvastatin? Far fewer.
Half-life matters too. Atorvastatin sticks around for up to 30 hours. Simvastatin clears in just 2 to 3 hours. That doesn’t mean one is “worse” - it just means the timing and duration of exposure vary. If you’re sensitive, even short bursts might trigger a reaction.
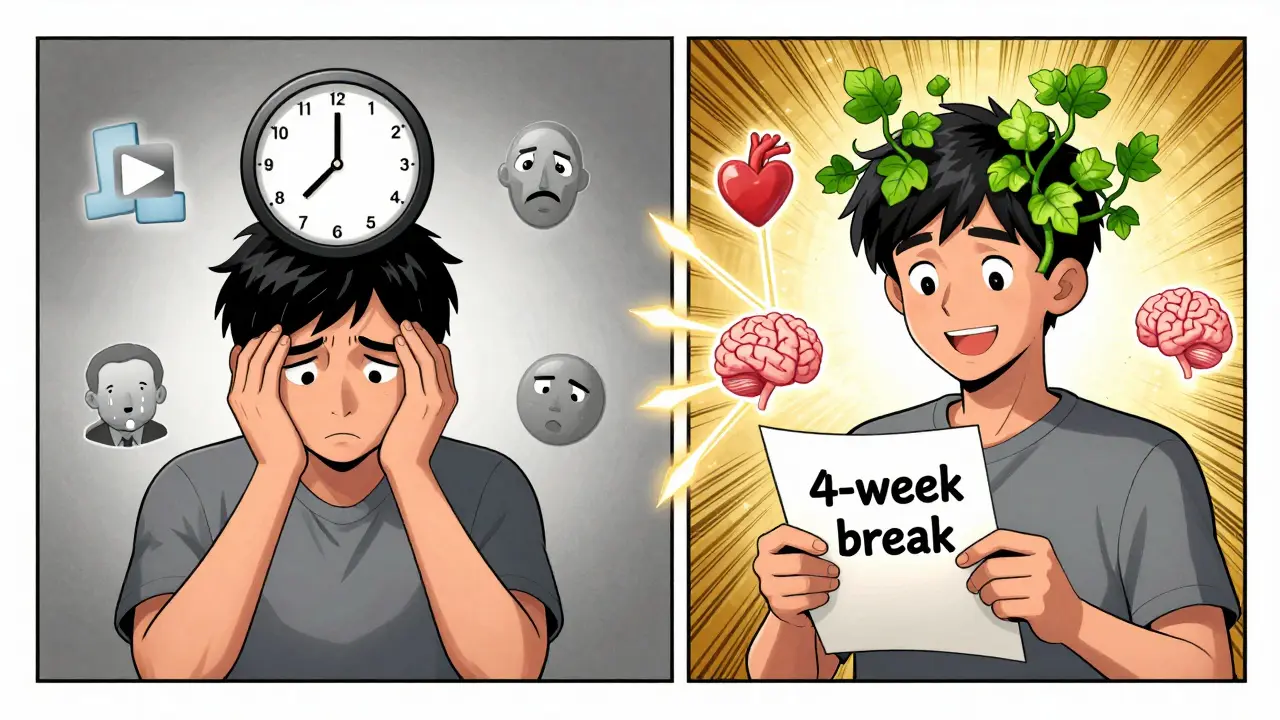
Reversibility Is the Key
One thing almost every study agrees on: if memory problems happen, they usually go away.
Dr. Beatrice Golomb’s 2003 analysis of 60 case reports found that 56% of patients improved after stopping statins. In the Reddit community r/Statins, a 2023 review of over 1,200 posts showed that 74% of people who stopped their statin saw memory improvements within four weeks. The FDA’s own MedWatch database from 1997 to 2002 found that half of the reported cases resolved after discontinuation.
That’s why doctors often suggest a “statin holiday.” The American Academy of Neurology recommends pausing the medication for 4 to 6 weeks. If your memory clears up, then comes back when you restart - that’s strong evidence it’s the statin. A 2019 Mayo Clinic study found this method correctly identified statin-related cognitive effects in 82% of cases.
It’s not a cure-all. But it’s a simple, safe way to test whether your brain fog is real - and drug-related.
What About Dementia? Do Statins Protect Your Brain?
Here’s where it gets really interesting. While some people worry about memory loss, long-term studies suggest statins might actually help prevent dementia.
The Alzheimer’s Society analyzed 36 studies involving over 1.2 million people. They found statin users had a 21% lower risk of developing dementia overall - and a 33% lower risk of vascular dementia, which is tied to blood vessel damage in the brain.
The Rotterdam Study, which followed 12,567 people for 15 years, found statin users had a 27% lower incidence of dementia. Why? Statins reduce inflammation, improve blood flow, and lower cholesterol - all of which help protect brain vessels. The same mechanisms that prevent heart attacks may also protect your thinking.
And it’s not just observational data. A 2023 study in Nature Communications showed that statins’ short-term cognitive effects might be partly caused by a drop in LDL and a rise in blood sugar - two side effects that can temporarily affect brain function. But over time, the vascular benefits appear to dominate.
What Should You Do If You’re Worried?
If you’ve started a statin and noticed memory slips, don’t panic. Don’t quit cold turkey. Talk to your doctor.
Here’s what to do:
- Track your symptoms. Note when they started, how often they happen, and what triggers them.
- Ask if you’re on a lipophilic statin (simvastatin, atorvastatin, lovastatin). If so, ask about switching to pravastatin or rosuvastatin.
- Request a 4- to 6-week break from the statin. If your memory improves, that’s a clue.
- Don’t assume it’s the statin. Other things - sleep apnea, thyroid issues, depression, vitamin B12 deficiency - can mimic brain fog.
- Rechallenge only under supervision. If symptoms return after restarting, you’ve got your answer.
Dr. JoAnn Manson of Harvard puts it simply: “The benefits of statins clearly outweigh the risks in people who are appropriate candidates.” For someone with a history of heart disease, high LDL, or diabetes, the protection statins offer is life-saving. For someone with mild cholesterol issues and no heart disease, the risk-benefit balance is different.
Doctors Are Still Prescribing - and Here’s Why
Despite the headlines, 78% of U.S. physicians continue statins in patients with mild cognitive impairment - unless the memory loss is severe and clearly tied to starting the drug.
Why? Because the data on long-term harm just isn’t there. The European Medicines Agency classifies memory disorders as “very rare” - affecting fewer than 1 in 10,000 patients. The American Heart Association and American College of Cardiology’s 2018 guidelines are clear: don’t stop statins because of vague memory complaints.
And the numbers speak for themselves. Statins generated $14.3 billion in global sales in 2022. Atorvastatin alone accounts for nearly 40% of prescriptions. If they were causing widespread brain damage, we’d see it in population-wide dementia rates. We don’t.
Bottom Line: It’s Rare, Reversible, and Often Overblown
Memory loss from statins is possible - but it’s uncommon. It usually shows up within the first few weeks. It almost always goes away when you stop the drug. And for most people, the risk of a heart attack or stroke far outweighs the chance of a temporary brain fog.
If you’re concerned, don’t suffer in silence. Talk to your doctor. Try a switch. Take a break. Test it out. But don’t stop your statin without a plan. Your heart is counting on it.
Can statins cause permanent memory loss?
No, there’s no strong evidence that statins cause permanent memory loss. In nearly all reported cases, cognitive symptoms improve after stopping the medication. Studies show that 50% to 75% of people who experience memory issues see improvement within weeks of discontinuation. Long-term brain damage from statins has not been demonstrated in large, high-quality studies.
Which statin is least likely to affect memory?
Pravastatin and rosuvastatin are the least likely to cause cognitive side effects because they’re hydrophilic - meaning they don’t cross the blood-brain barrier easily. In contrast, lipophilic statins like simvastatin and atorvastatin are more likely to be associated with memory complaints. If you’re concerned about brain fog, switching to one of these two may help.
How long does it take for memory to improve after stopping statins?
Most people who experience statin-related memory issues notice improvement within 2 to 4 weeks after stopping the drug. Some feel better in days; others take up to 6 weeks. A 2019 Mayo Clinic study found that 82% of patients who took a 4- to 6-week break saw clear improvement, confirming the link between the drug and symptoms.
Do statins increase the risk of Alzheimer’s disease?
No - the opposite appears to be true. Multiple large studies, including one from the Alzheimer’s Society analyzing over 1.2 million people, show that statin users have a 21% lower risk of developing dementia overall, and up to a 33% lower risk of vascular dementia. Statins help protect blood vessels in the brain, which may reduce the risk of dementia linked to poor circulation.
Should I stop taking statins if I have mild memory problems?
Not without talking to your doctor. Mild memory lapses can have many causes - stress, sleep deprivation, vitamin deficiencies, or thyroid issues. If you suspect statins, ask about a supervised 4- to 6-week break. If your memory improves, you can rechallenge to confirm. But if you have heart disease, high cholesterol, or diabetes, stopping statins without a plan could put your heart at risk.
What’s Next?
Research is still evolving. The STATIN-COG trial, funded by the NIH and tracking 3,200 people over five years, will deliver its first results in late 2024. That study could finally settle whether statins have a real, measurable impact on brain function - or if the concerns are mostly noise.
For now, the best advice is simple: if you’re on a statin and feel your memory slipping, don’t ignore it. But don’t assume the worst, either. Work with your doctor. Test it out. And remember - for most people, the statin is saving their life, not stealing their memory.

All Comments
Darren McGuff January 7, 2026
Man, I remember when I first heard about statin brain fog. I was on atorvastatin for six months and started forgetting my wife’s birthday. Not the kind of thing you forget. Turned out it was the statin - switched to rosuvastatin, and boom, memory came back like I’d been on vacation. No drama, no panic. Just science. If you’re having issues, don’t suffer. Talk to your doc. Pravastatin or rosuvastatin are your friends.
Catherine Scutt January 8, 2026
I stopped mine after one week. Brain fog was real. No more statins for me.
Jacob Paterson January 8, 2026
Oh wow, another one of you people thinks your brain fog is magic. Let me guess - you also think gluten gave you anxiety and your phone is spying on you. The FDA added a warning because people complained, not because there’s proof. You’re not special. Your memory’s just bad because you’re 52 and binge-watching Netflix while eating nachos.
Heather Wilson January 8, 2026
Let’s be brutally honest: the entire ‘statin memory loss’ narrative is a perfect storm of confirmation bias, media sensationalism, and patients who mistake normal aging for pharmaceutical sabotage. The 28% who report memory issues? They’re the same people who Google every sneeze and come away convinced they have brain cancer. The 8% who show actual decline? That’s within the margin of error for normal cognitive fluctuation in middle-aged adults. The real issue isn’t statins - it’s our collective willingness to pathologize forgetfulness.
And yet, here we are, turning a rare, reversible side effect into a cultural panic. Meanwhile, heart disease still kills 650,000 Americans yearly. But sure, let’s swap a life-saving drug for ‘natural remedies’ and hope our arteries don’t turn into concrete.
Ian Long January 9, 2026
I get both sides. I’ve seen patients lose their keys and then get them back after stopping statins. I’ve also seen people who swear their memory’s shot - but it’s just stress, sleep apnea, or depression. The key isn’t to panic or to dismiss. It’s to test. A 6-week break? Low risk. High reward. If your memory clears? Great. If not? You didn’t lose anything. And if your LDL’s still high? You’ve got a better story to tell your doctor.
Gregory Clayton January 11, 2026
Y’all are acting like statins are some kind of Big Pharma mind-control drug. We’re talking about a pill that saves lives. My grandpa had a heart attack at 68. He’s still alive at 82 because of atorvastatin. You think he’d trade that for remembering where he put his damn keys? Hell no. You want to stop your statin? Fine. But don’t pretend you’re some brave health warrior. You’re just scared of pills.
Aron Veldhuizen January 11, 2026
Let’s deconstruct the epistemological fallacy at play here: the conflation of subjective phenomenology with objective neurophysiological change. The fact that individuals report memory lapses does not imply causation, nor does it validate the nocebo effect as a diagnostic tool - it merely reveals the human tendency to attribute internal states to external agents when cognitive dissonance arises. The FDA’s labeling, while politically expedient, is not scientific consensus. It is a legal safeguard against litigation, not a biological revelation. The true question is not whether statins cause memory loss - but whether our society has become so averse to pharmacological nuance that we mistake correlation for catastrophe.
Micheal Murdoch January 13, 2026
If you’re worried about memory issues on statins, you’re not alone - and you’re not crazy. I’ve been a primary care doc for 18 years, and I’ve had more than a hundred patients come in with the same story: ‘I used to be sharp. Now I’m foggy.’ And guess what? Most of them got better after switching to rosuvastatin or taking a break. It’s not about fear. It’s about listening. Your brain matters. Your heart matters. You don’t have to choose one over the other. Sometimes, it’s just about finding the right statin - not quitting the whole game. Talk to your doctor. Try a switch. Give it time. You might be surprised.
And if you’re reading this and thinking, ‘I’m too old for this,’ - you’re not. Age isn’t the enemy. Ignorance is. Knowledge is power. And you’ve got the power to ask the right questions.
Jeffrey Hu January 14, 2026
Okay, but did anyone check if their vitamin D was low? Or their B12? Or if they’re sleep-deprived from scrolling TikTok until 2 a.m.? People blame statins for everything. I had a patient who thought his forgetfulness was from statins - turned out he had undiagnosed sleep apnea and was getting 3 hours of sleep a night. He stopped the statin, felt worse, then realized it was his sleep. Now he uses a CPAP. Moral of the story? Don’t assume. Test everything. Statins are the easiest scapegoat, but they’re rarely the real villain.
Drew Pearlman January 14, 2026
I just want to say - if you’re reading this and you’re scared about your memory, you’re not alone. I was too. I was on simvastatin for two years, and I started forgetting names, missing appointments, feeling like my thoughts were wrapped in cotton. I cried in my doctor’s office. I thought I was losing myself. But then I switched to pravastatin. Within three weeks, I remembered my daughter’s favorite song. I started reading books again. I didn’t just get my memory back - I got my life back. It’s not about being weak. It’s about being brave enough to say, ‘This isn’t right.’ And then doing something about it. You deserve to feel like yourself again. Don’t let fear keep you silent. Talk to your doctor. You’ve got this.
Ashley Kronenwetter January 15, 2026
Thank you for this thorough and well-referenced overview. The distinction between lipophilic and hydrophilic statins is critical and often overlooked in patient education. The reversibility of cognitive symptoms, supported by both clinical data and patient-reported outcomes, underscores the importance of individualized care. I encourage all clinicians to proactively discuss these potential side effects with patients at initiation, rather than waiting for complaints to arise. A collaborative, evidence-based approach ensures that patients remain adherent to life-saving therapy while minimizing unnecessary anxiety.