Imagine trying to follow a conversation in a busy restaurant, but no matter how hard you listen, voices from your left side vanish into silence. You turn your head, lean forward, and still hear nothing. This isn’t just poor hearing-it’s single-sided deafness (SSD), a condition where one ear has little to no hearing, while the other works normally. About 4 to 5 out of every 100,000 people develop it each year, often after an infection, injury, or sudden hearing loss. The problem isn’t just missing sound-it’s the head shadow effect. High-frequency speech sounds, like "s" and "th," get blocked by your skull before they reach your good ear. Background noise becomes overwhelming. You feel isolated, exhausted, and constantly guessing what people are saying.
What Are CROS Hearing Aids?
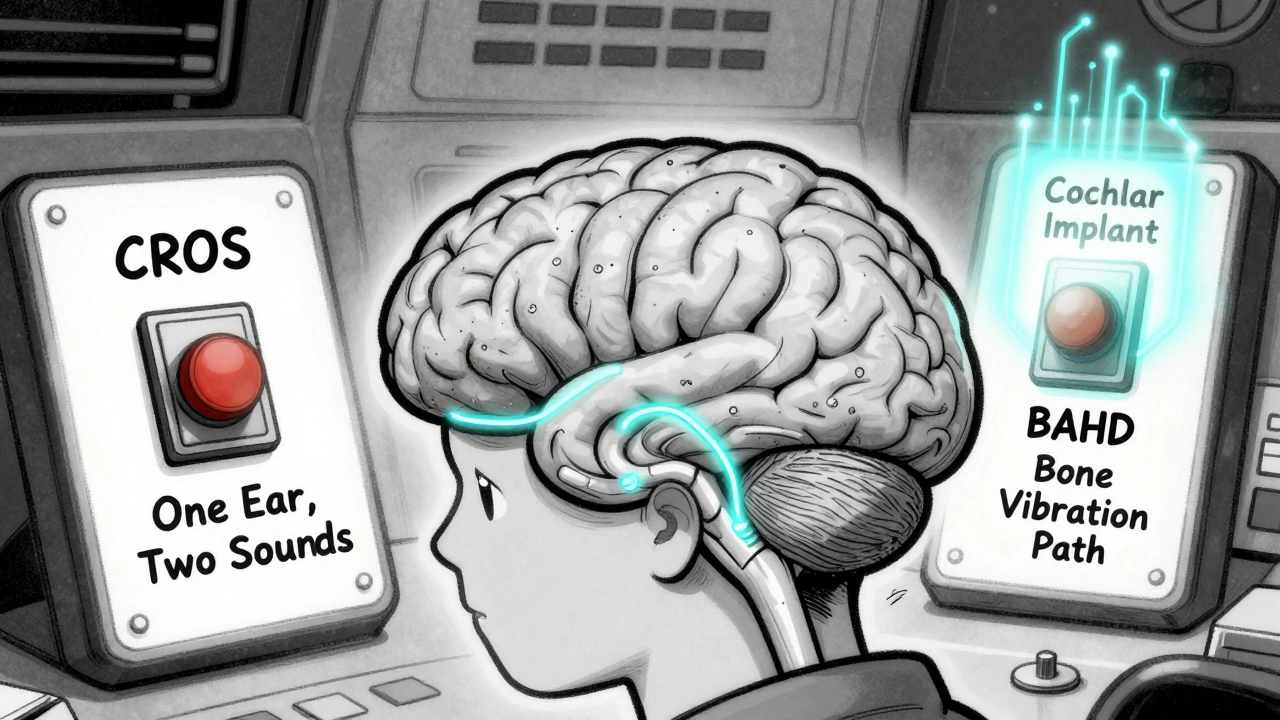
CROS stands for Contralateral Routing of Signals. It’s a non-surgical solution that uses two devices: a microphone on the deaf side and a hearing aid on the better ear. The microphone picks up sound from the deaf side and sends it wirelessly-usually via Bluetooth or magnetic signals-to the hearing aid on the good ear. Modern systems like Phonak CROS Marvel, Oticon CROS Free, and Signia CROS Pure 312 are small, nearly invisible, and connect seamlessly.
These devices don’t restore hearing in the deaf ear. Instead, they reroute sound. That means you hear voices from both sides, but only through one ear. For many, this is a game-changer. You can finally hear someone calling your name from behind, or catch a word spoken while you’re driving. Studies show CROS reduces the head shadow effect by 8-10 dB, making speech clearer in quiet settings.
But there’s a catch. In noisy places-like a café or a family dinner-the system can backfire. When noise comes from the deaf side, the CROS device picks it up and sends it straight to your good ear. Your brain gets flooded with competing sounds. One study found users actually understood speech worse with CROS than without it when noise was on the deaf side. That’s why some people quit after a few months. Battery life is another issue. Most need a new battery every two to three days. If you’re active, forgetful, or hate fiddling with tiny batteries, this can be frustrating.
How Do Bone-Anchored Hearing Devices Work?
Bone-anchored hearing devices (BAHD), also called bone conduction systems, work differently. Instead of sending sound through the air, they send vibrations directly through your skull bone to the inner ear. Think of it like tapping your finger on your temple-you feel the vibration. That’s what BAHD does, but with precision.
There are two types: percutaneous and transcutaneous. Percutaneous systems, like the Cochlear Baha 6 Max, have a titanium implant surgically placed in the skull behind the ear. Over three to six months, the bone grows around the implant (osseointegration), creating a solid anchor. A sound processor then clips onto a small abutment sticking out of the skin. Transcutaneous systems, like Oticon Medical Ponto 5 SuperPower, use magnets to hold the processor against the skin without breaking through it. No visible post, but slightly less power.
BAHD bypasses the ear canal entirely. That means no occlusion effect (that plugged-up feeling you get with regular hearing aids). Sound feels more natural. Wind noise? Less of a problem. During exercise? The device stays put. A 2022 study found 92% of BAHD users reported no issues with device movement during physical activity, compared to just 68% of CROS users.
But surgery isn’t simple. The procedure takes about 45 minutes under local anesthesia, but recovery isn’t instant. You need to wait three to six months before turning the device on. Then there’s skin care. About 58% of percutaneous users get skin irritation around the abutment at least once a year. Some need antibiotic cream, special cleaning routines, or even minor surgeries to fix it. Transcutaneous systems reduce this risk but may not deliver as much sound power.
Which One Is Better?
There’s no one-size-fits-all answer. It depends on your lifestyle, hearing goals, and tolerance for surgery.
If you want to avoid surgery, have normal hearing in your good ear, and mostly need help in quiet environments, CROS might be your best first step. It’s cheaper-$2,500 to $4,000 for the pair-and you can try it before buying. Many clinics offer a two-week trial. You’ll adapt quickly: 78% of users feel comfortable within two weeks.
If you’re active, work in noisy places, or have mild hearing loss in your good ear (up to 45-55 dB), BAHD might be worth the surgery. It gives you better sound quality, handles noise better, and doesn’t require daily battery changes. Most users report improved spatial awareness-knowing where sound is coming from-even if it’s not perfect. In one study, BAHD users scored 3.5 dB better than CROS users in speech tests when noise came from the deaf side.
But here’s something most people don’t tell you: both devices only give you monaural hearing. You’re still hearing with one ear. Your brain doesn’t get true binaural cues-like tiny time differences between when sound hits each ear-that help us locate sound naturally. That’s why even with BAHD, sound localization is still worse than normal hearing. In a 2015 trial, people with cochlear implants on the deaf side had the best spatial hearing. That’s why experts now recommend considering cochlear implants for SSD if other options don’t work.
Who Should Avoid Each Option?
Not everyone qualifies. For CROS, your better ear must have near-normal hearing-pure-tone average below 25 dB. If your good ear is already struggling, CROS won’t help. It can even make things worse by overloading it with too much sound.
For BAHD, your skull bone must be thick enough-minimum 3.5 mm at the implant site. A CT scan checks this. If you have active skin conditions, poor healing, or are on long-term steroids, you’re not a candidate. Children under five usually don’t get implants because their skulls are still growing.
Also, if you’re not willing to commit to daily skin care or handle the risk of infection, skip BAHD. If you hate changing batteries or can’t stand the idea of a device that sometimes sounds like voices are coming from inside your head, CROS might not be for you.
Real People, Real Experiences
Reddit user HearingHelp101 tried a Phonak CROS for six months. "I love not having surgery," they wrote. "But voices from my deaf side sound like they’re inside my skull. And I’m changing batteries every two days. It’s exhausting." Another user, SkullVibrator, chose Cochlear Baha. "I get skin irritation twice a month," they said. "I have to clean it with alcohol wipes and use antibiotic cream. But the sound? Worth it. I finally hear my kids calling from the other room." A 2022 survey found CROS users were happier with the fitting process-87% said it was easy. But BAHD users were more satisfied long-term. Only 46% of CROS users showed up for their 12-month follow-up. Nearly all BAHD users did.
Cost, Care, and Future Tech
CROS systems cost $2,500-$4,000. No surgery. No insurance hassle in most cases. Repairs? Usually fixed in two business days.
BAHD costs $4,000-$8,000 for the device, plus $3,000-$7,000 for surgery. Insurance sometimes covers part of it, but not always. Repairs take longer-up to two weeks-because only a few centers handle them.
New tech is coming. Signia’s 2023 CROS model now includes tinnitus therapy-helpful since 78% of SSD patients also have ringing in the ears. Cochlear’s 2024 Baha 7 uses AI to reduce background noise in real time. And in January 2024, the FDA expanded cochlear implant approval for SSD. For some, that’s now the best long-term option.
Experts now recommend a step-by-step approach: try CROS first. If it doesn’t work after four weeks, move to BAHD. If you’re still struggling with spatial hearing after six months on BAHD, consider a cochlear implant.
What’s the Bottom Line?
Single-sided deafness doesn’t have a perfect fix-but it has options. CROS is simple, affordable, and risk-free. But it’s not magic. It helps in quiet, struggles in noise, and demands daily maintenance.
Bone-anchored devices are more involved, but they deliver better sound, stability, and long-term satisfaction. If you’re willing to accept surgery and skin care, BAHD gives you a more natural listening experience.
Don’t rush. Try a CROS trial. Talk to an audiologist who specializes in SSD. Ask about cochlear implants if you’re still struggling. Your hearing matters-not just for conversations, but for safety, confidence, and connection.
Can CROS hearing aids restore hearing in my deaf ear?
No. CROS systems don’t restore hearing in the deaf ear. They pick up sound from that side and wirelessly send it to your better ear. You still hear with only one ear, but you can hear sounds from both sides. It helps with the head shadow effect but doesn’t recreate true binaural hearing.
Is bone-anchored surgery risky?
The surgery itself is low-risk and usually done under local anesthesia. But complications can happen. Skin irritation around the abutment affects up to 63% of users, sometimes requiring antibiotic cream or minor procedures. Infection, poor bone integration, or implant loosening are rare but possible. Transcutaneous systems reduce skin risks but may offer slightly less sound power.
How long do CROS and bone-anchored devices last?
CROS hearing aids typically last 3-5 years before needing replacement. Batteries need changing every 2-3 days. Bone-anchored processors last about 5-7 years. The titanium implant, if properly integrated, can last a lifetime. Only the external processor needs replacing over time.
Can I use CROS if my good ear has some hearing loss?
CROS is designed for people with normal or near-normal hearing in the better ear (pure-tone average ≤25 dB). If your good ear has mild to moderate hearing loss (up to 45-55 dB), a bone-anchored device is usually better. CROS can overload your good ear and make speech harder to understand.
Do I need a cochlear implant for SSD?
Not always. Most people start with CROS or bone-anchored devices. But if you still struggle with understanding speech in noise or locating sounds after 6 months of using BAHD, a cochlear implant may be the next step. The FDA expanded CI approval for SSD in January 2024, and studies show it offers the best sound localization outcomes.
Will insurance cover CROS or bone-anchored devices?
CROS hearing aids are often not covered by Medicare or private insurance because they’re classified as Class I devices. Bone-anchored systems are Class II medical devices, and many insurers will cover part or all of the cost if you have documented hearing loss and a doctor’s recommendation. Always check with your provider and ask about surgical coverage.
Can children get bone-anchored devices?
Children as young as five can get bone-anchored devices, but only if their skull bone is thick enough for implantation. Younger children usually wear a softband version-a headband that holds the processor against the skull without surgery. Surgery is delayed until the skull has grown enough, typically around age five or six.
Why do some people quit using CROS?
Many quit because the sound quality isn’t natural-voices from the deaf side can sound hollow or like they’re coming from inside the head. Battery life is short, requiring changes every two days. And in noisy environments, CROS can make speech harder to understand. Studies show nearly half of users stop using CROS after a year because the benefits don’t match their expectations.


All Comments
Jaswinder Singh December 1, 2025
Bro this is wild I had no idea CROS could make noise worse. I tried one for three weeks and it felt like my brain was being hijacked by random whispers from my dead side. Battery life? Absolute joke. Changed them every 48 hours like clockwork. Gave up and got a BAHD. Worth every penny and every scar.
Bee Floyd December 3, 2025
There’s something quietly beautiful about how technology can bridge the silence between us and the world. Not magic, not perfect-but a quiet, stubborn kind of grace. I’ve seen people go from isolated to present, just because they finally heard their kid laugh from the other side of the room. That’s the real win.
Jeremy Butler December 5, 2025
It is imperative to recognize that the physiological and psychological ramifications of unilateral auditory deprivation extend beyond mere perceptual inconvenience. The head shadow effect, while quantifiable in decibels, engenders a profound epistemological dislocation in spatial auditory cognition. The proposed technological interventions, while pragmatically efficacious, remain fundamentally epiphenomenal in their capacity to restore binaural integrity.
Courtney Co December 6, 2025
I just cried reading this. My brother had SSD after meningitis at 12. He used CROS for a year and then just… stopped talking to people. He’d sit in silence at dinner. I didn’t know why until I read this. Now he’s getting his BAHD next month. Thank you for saying what no one else did.
Shashank Vira December 7, 2025
One must ask: are we not merely patching the symptom rather than confronting the ontological rupture of unilateral sensory loss? CROS and BAHD are elegant bandages on a severed nerve. The true solution lies not in rerouting sound but in neuroplastic recalibration - and yet, we settle for amplification. How tragic. How profoundly human.
Eric Vlach December 8, 2025
So CROS is like a wireless mic for your bad ear but you hear it through your good one? Yeah that sounds like a glitchy AirPods connection. Batteries every 2 days? No thanks. BAHD is the real MVP. I got mine last year and I can finally hear my dog bark from the backyard. No more leaning in like a detective. Life changed.
Souvik Datta December 8, 2025
To anyone considering these options: don’t rush. This isn’t just a device choice - it’s a lifestyle shift. Try the CROS trial. Give it two weeks. If you’re still exhausted after listening to your own family, it’s not you - it’s the tech. BAHD isn’t just surgery, it’s an investment in your peace. And if you’re still struggling after six months? Don’t be afraid of the cochlear implant. It’s not failure. It’s evolution.
Priyam Tomar December 8, 2025
Everyone’s acting like this is groundbreaking. Newsflash: CROS has been around since the 90s. BAHD? Same. And now we’re treating them like miracle cures? You still hear with one ear. You still can’t localize sound properly. And you’re paying thousands for a glorified Bluetooth speaker glued to your skull. The real solution? Learn lip reading. Or move to a quiet country. Or stop pretending tech fixes biology.
Jack Arscott December 9, 2025
Just got my Baha 6 Max last month 😍 no more battery drama, no more weird echo-y voices. Skin irritation? Yeah, but a little aloe vera and I’m good. I can finally hear my cat purr from across the room 🐱❤️
Irving Steinberg December 10, 2025
So you’re telling me I gotta pay 8k and get surgery just to hear my wife say ‘honey dinner’s ready’? I’ll just turn my head. I’ve been doing it for 15 years. Also batteries? Nah. I’m not a robot. 🤖❌
Lydia Zhang December 11, 2025
My mom has SSD. She uses CROS. She hates it. She says it sounds like the TV is in her head. She’s going to try BAHD next year. I hope it works.
Kay Lam December 13, 2025
I’ve been working with SSD patients for over a decade and I can tell you this: the emotional toll is often worse than the physical. People feel like they’re broken. Like they’re asking too much. The tech helps, but what really changes lives is the quiet support from audiologists who don’t treat them like a case file. Take the time to find one who listens. Not just to the numbers, but to the silence behind them.
Grant Hurley December 15, 2025
My buddy got the Signia CROS and now he’s got tinnitus relief built in? That’s wild. I didn’t even know that was a thing. He says the noise canceling actually helps him sleep now. I’m gonna ask my audiologist about it. Also typo: ‘fiddling with tiny batteries’ - yep, that’s me.
Lucinda Bresnehan December 15, 2025
I’m a deafness advocate and I’ve seen so many people give up on CROS because they didn’t know what to expect. It’s not a cure. It’s a tool. And like any tool, it takes practice. I wish more clinics gave people real demos - like sitting them in a noisy coffee shop with and without the device. That’s the only way to know if it’s right for you.