Statin Rhabdomyolysis Risk Assessment Tool
Your Risk Assessment
Statins save lives. Millions of people take them every day to lower cholesterol and prevent heart attacks and strokes. But for a very small number of people, these common medications can trigger something dangerous: rhabdomyolysis. It’s rare-about 1.5 to 5 cases per 100,000 people per year-but when it happens, it can be life-threatening. Muscle tissue breaks down rapidly, spilling proteins into the bloodstream that can crush your kidneys. This isn’t just muscle soreness. This is a medical emergency.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis means your skeletal muscles are breaking down. Think of it like your muscles melting from the inside. When this happens, a protein called myoglobin floods into your blood. Your kidneys try to filter it out, but myoglobin clogs the tiny tubes inside them. That’s when kidney damage starts. Without quick treatment, you could need dialysis-or worse. The symptoms don’t sneak up. You’ll feel it. Severe muscle pain, especially in your thighs, shoulders, or lower back. Weakness so bad you can’t climb stairs. Dark urine-brown, tea-colored, or even red. These aren’t normal aches after a workout. If you’re on a statin and notice this, don’t wait. Get checked.Why Do Statins Cause This?
Statins work by blocking an enzyme called HMG-CoA reductase. That’s how they lower cholesterol. But that same enzyme is involved in making other important molecules your muscles need. When statins shut it down, they accidentally starve your muscle cells of things like coenzyme Q10 (CoQ10), which helps produce energy. Some research shows CoQ10 levels drop by up to 40% in people on high-dose statins. But that’s not the whole story. Statins also mess with how your muscles repair themselves. They turn up genes like atrogin-1, which tells your body to break down muscle proteins faster than they can be rebuilt. This is called the ubiquitin-proteasome system. Think of it like your muscles being torn down by a factory that’s gone rogue. There’s also evidence that statins make muscle cell membranes less stable. If you’re doing something that stretches your muscles-like hiking downhill, lifting weights, or even walking on uneven ground-it might trigger a chain reaction inside the cells. This is especially true for more lipophilic statins like simvastatin and lovastatin, which slip more easily into muscle tissue.Not All Statins Are the Same
If you’re worried about muscle damage, the type of statin you take matters. Simvastatin at 80 mg carries the highest risk. In fact, the FDA warned doctors in 2011 to avoid prescribing that dose to new patients. The SEARCH trial showed people on 80 mg of simvastatin had over 10 times the risk of muscle injury compared to those on 20 mg. On the other end, pravastatin and fluvastatin are much gentler on muscles. Rosuvastatin and pitavastatin also have lower risk profiles. Why? Because they don’t rely as much on the CYP3A4 liver enzyme to break down. That’s important because many common drugs-like antibiotics (clarithromycin), antifungals, and even grapefruit juice-block CYP3A4. When that happens, statins like simvastatin and atorvastatin build up in your blood like traffic on a highway with no exits. One real-world example: a 72-year-old man on simvastatin 40 mg took clarithromycin for a sinus infection. His simvastatin levels spiked 10-fold. Within days, he had severe muscle pain and kidney failure. He survived, but only because his doctor caught it early.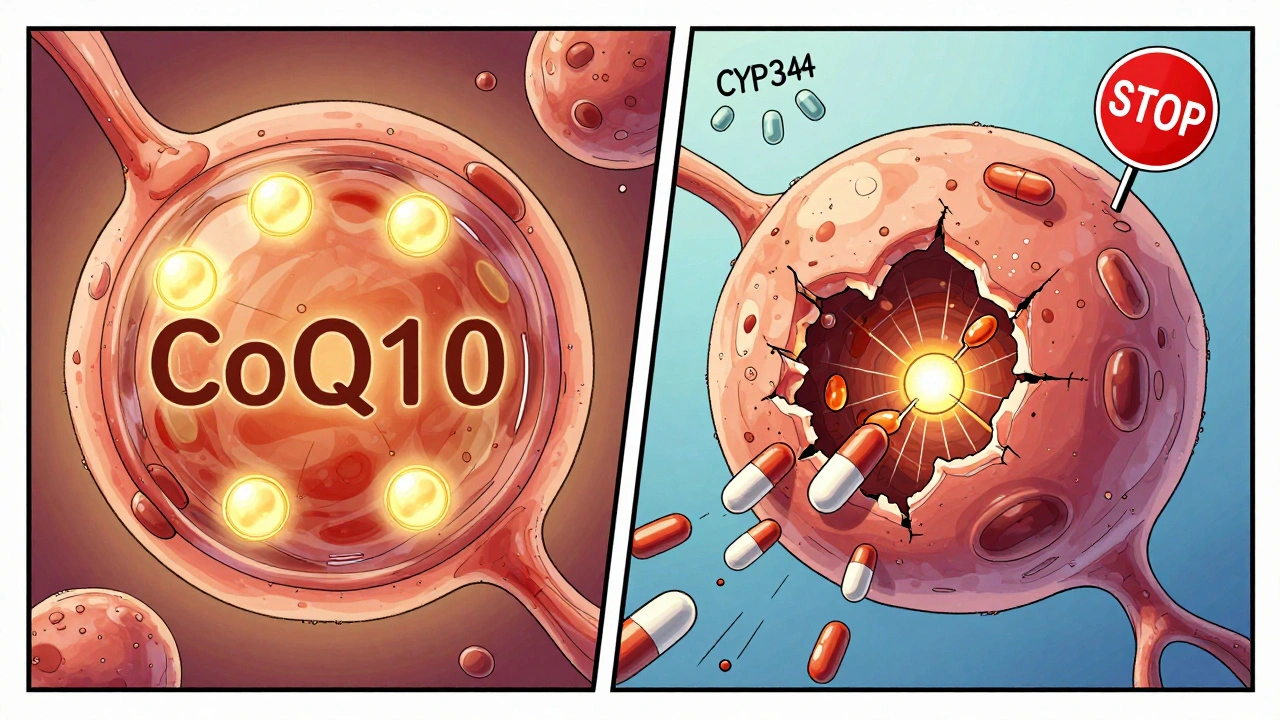
Who’s Most at Risk?
Age is a big factor. About 78% of rhabdomyolysis cases happen in people over 65. Women are more likely to be affected than men. If you have kidney disease, thyroid problems, or are dehydrated, your risk goes up. So does taking multiple medications that affect how your body processes statins. Genetics play a role too. About 1 in 10 people carry a gene variant called SLCO1B1 c.521T>C. This gene controls how well your liver pulls statins out of your blood. If you have two copies of this variant, your statin levels can be 200% higher than normal. That’s why some people get muscle pain on low doses while others take 80 mg without issue. There’s a test for this. Companies like OneOme offer a $249 genetic test that checks your SLCO1B1 status. Insurance usually won’t cover it unless you’ve already had muscle problems. But if you’re starting a statin and have a family history of muscle issues, it’s worth asking your doctor.What to Do If You Have Muscle Pain
Not every ache means rhabdomyolysis. About 5% to 29% of people on statins report muscle discomfort, but only a tiny fraction develop true muscle breakdown. The key is knowing when to act. If you have mild soreness that goes away after a few days, it might be nothing. But if the pain is deep, persistent, or gets worse with movement, don’t ignore it. See your doctor. They’ll check your creatine kinase (CK) levels. Normal CK is under 200 IU/L. If it’s over 1,000, that’s a red flag. Over 10,000? That’s rhabdomyolysis. Your doctor might stop your statin for a few weeks, then try a different one at a lower dose. Many people who think they’re statin-intolerant can actually tolerate a switch. The American College of Cardiology says 78% of people who quit statins due to muscle pain can get back on them with the right approach. Physical therapists recommend avoiding eccentric exercise-things like downhill walking, lowering weights slowly, or descending stairs quickly. These movements stress muscles in ways that may trigger the membrane instability linked to statin damage. Stick to gentle walking, swimming, or cycling.
What Happens After Diagnosis?
If rhabdomyolysis is confirmed, you’ll need hospital care. The goal is to flush out the myoglobin before it damages your kidneys. You’ll get IV fluids-lots of them. Your creatinine levels will be monitored closely. If your kidney function drops by more than 0.5 mg/dL, a nephrologist needs to get involved. You’ll likely never take that statin again. But you might still need to lower your cholesterol. Alternatives include ezetimibe, bile acid sequestrants, or PCSK9 inhibitors like evolocumab. The problem? Those cost over $5,800 a year. Most people can’t afford them without insurance.The Bigger Picture: Risk vs. Reward
Yes, rhabdomyolysis is scary. But the numbers put it in perspective. Statins prevent about 500,000 heart attacks and strokes every year in the U.S. alone. The chance of dying from rhabdomyolysis from a statin is less than 1 in a million per year. For someone with high cholesterol and a history of heart disease, the benefit of taking a statin is enormous. The real problem isn’t the rare complication-it’s the fear that keeps people from taking them. A 2019 study found that muscle side effects cause 75% of statin discontinuations. But many of those cases weren’t true drug reactions. Sometimes, it’s the nocebo effect: you expect to feel bad, so you do. That’s why doctors now encourage open conversations. If you’re worried, talk about it. Get tested. Try a different statin. Don’t quit cold turkey. You’re not alone. And you don’t have to live with high cholesterol.What’s Next?
Science is getting better at predicting who’s at risk. In 2023, a study called STOMP found 17 proteins in the blood that can predict statin muscle damage with nearly 90% accuracy. That means in the near future, your doctor might run a simple blood test before prescribing a statin-and pick the one safest for you. New statins are also in development. Researchers are designing molecules that lower cholesterol without touching muscle cells. Early trials look promising. For now, the message is clear: statins are safe for most people. But if you feel unusual muscle pain, don’t brush it off. Know the signs. Get checked. Your muscles-and your heart-will thank you.Can statins cause muscle pain without rhabdomyolysis?
Yes. About 5% to 29% of people on statins report muscle discomfort, soreness, or weakness-this is called statin-associated muscle symptoms (SAMS). These symptoms are usually mild and don’t involve muscle breakdown or elevated creatine kinase. Many people mistake normal exercise soreness for statin side effects. But if the pain is deep, persistent, or worsens with movement, it’s worth checking with a doctor to rule out rhabdomyolysis.
Which statin has the lowest risk of muscle damage?
Pravastatin and fluvastatin have the lowest risk of muscle-related side effects. Rosuvastatin and pitavastatin are also considered safer choices. These statins are less dependent on the CYP3A4 liver enzyme for metabolism, which means they’re less likely to build up to dangerous levels when taken with other medications or in people with genetic differences. Simvastatin, especially at 80 mg, carries the highest risk.
Should I get genetic testing before starting a statin?
Routine genetic testing isn’t recommended for everyone. But if you’ve had unexplained muscle pain on a statin before, or if you have a family history of statin intolerance, testing for the SLCO1B1 gene variant can be helpful. The c.521T>C variant increases statin exposure by up to 221% in homozygous carriers. If you carry it, your doctor may choose a lower dose or a different statin. Tests like OneOme RightMed cost around $249 and are not always covered by insurance.
Can I exercise while taking statins?
Yes-but be smart. Avoid eccentric exercises like downhill hiking, heavy weightlifting with slow lowering phases, or jumping down from heights. These movements stress muscles in ways that may trigger statin-related damage. Stick to moderate, steady activities like walking, swimming, or cycling. Stay hydrated and listen to your body. If you feel unusual pain during or after exercise, stop and talk to your doctor.
How do I know if my muscle pain is serious?
Look for three signs: 1) Severe, deep muscle pain that doesn’t improve with rest, 2) Muscle weakness that makes daily tasks hard (like climbing stairs), and 3) Dark, tea-colored, or red urine. These are red flags for rhabdomyolysis. Normal soreness from exercise fades within a day or two. If your pain lasts longer than a week, gets worse, or comes with dark urine, get a creatine kinase (CK) blood test immediately.
Can I restart a statin after having rhabdomyolysis?
Generally, no. Once you’ve had rhabdomyolysis, restarting the same statin is not advised. However, some people can tolerate a different statin at a low dose after a period of time. This should only be done under close medical supervision with regular CK monitoring. For those who need ongoing cholesterol control, non-statin options like ezetimibe or PCSK9 inhibitors may be considered, though they’re much more expensive.


All Comments
Ronald Ezamaru December 9, 2025
Statins saved my dad’s life after his second heart attack. He’s 78, on rosuvastatin, and feels better than he has in years. I get the fear-muscle pain is real-but dismissing statins because of rare side effects is like avoiding planes because of crashes. The math is clear: benefit outweighs risk by miles.
Don’t ignore symptoms, but don’t let fear make you stop what’s working.
Ryan Brady December 10, 2025
Another Big Pharma lie. They don’t care if you’re weak or in pain-they just want you hooked on pills so you keep buying them. My cousin took simvastatin and ended up in the ER. They didn’t even warn him. It’s all about profit, not health.
Raja Herbal December 11, 2025
So let me get this straight-you’re telling me a drug that costs $5 a month can literally melt your muscles, but the FDA won’t ban it because it ‘saves lives’? Sounds like a classic case of ‘better dead than broke.’
Meanwhile, in India, grandmas cure cholesterol with turmeric and yoga. Just saying.
Rich Paul December 12, 2025
bro i was on simva 40mg and got like, insane quad pain after hiking. thought it was just soreness till my ck hit 8k. doc said it was classic statin myo. switched to pravastatin and zero issues now.
also, grapefruit juice is a nightmare with statins-like, don’t even look at it. cyp3a4 is a bitch.
Delaine Kiara December 13, 2025
Okay but have you considered that maybe your body is just telling you something? I mean, think about it-your muscles are literally dissolving. That’s not just ‘side effect,’ that’s your body screaming. And then they say ‘try a different statin’ like it’s switching coffee brands.
And don’t get me started on the cost of PCSK9 inhibitors. $5,800 a year? That’s not medicine, that’s a luxury subscription. Who even has that kind of cash?
Also, I read somewhere that statins can mess with your mitochondria. Like, the energy factories in your cells. Isn’t that wild? It’s like your body’s battery is being drained by a ghost.
And why is it always older women? Is it hormones? Genetics? Or are we just more sensitive to corporate greed? I’m just saying-there’s a pattern here.
And what about the nocebo effect? Isn’t that just another way of saying ‘it’s all in your head’? But if your pain is real, then the head is just the messenger.
I’ve seen too many people quit statins and then have a stroke. And I’ve seen too many people stay on them and end up in wheelchairs. It’s a lose-lose, and nobody’s talking about the middle ground.
Also, I heard that some people get rhabdo from just one dose. One. Single. Dose. And they say it’s rare? RARE? My neighbor’s dog had more warning than that.
And what if you’re one of the 1 in 10 with the SLCO1B1 variant? You don’t know until it’s too late. Why isn’t this testing mandatory? Why is it $249? Why?
And why do they always say ‘don’t quit cold turkey’ like we’re addicts? We’re not addicts. We’re patients. And we deserve better than this.
Noah Raines December 15, 2025
My uncle had rhabdo on simva 80. Scary stuff. He’s fine now, but he switched to pitavastatin and barely touches the gym anymore. Honestly? If you’re active, go with pravastatin or fluvastatin. Less muscle drama.
Also, stay hydrated. That’s not just doctor talk-it actually helps flush out the junk.
And no, grapefruit juice isn’t just a myth. Don’t test it.
Gilbert Lacasandile December 15, 2025
I’ve been on atorvastatin for 7 years. Mild soreness sometimes, but nothing serious. I think the key is listening to your body and not pushing through pain. Also, talking to your doc before making any changes.
It’s not black and white, but it’s not as scary as some make it out to be either.
Lola Bchoudi December 15, 2025
For anyone worried about statin myopathy: get your CK checked before and after starting. Baseline matters. And if you’re on multiple meds-especially antibiotics or antifungals-ask your pharmacist about CYP3A4 interactions. It’s not just the statin-it’s the combo.
Also, CoQ10 supplementation? Evidence is mixed, but if you’re prone to fatigue or cramping, it’s low-risk and worth a try. Talk to your doc about 100–200mg/day.
And don’t skip the genetic test if you’ve got family history. SLCO1B1 isn’t just a gene-it’s a lifesaver if you catch it early.
Morgan Tait December 17, 2025
Did you know the FDA approved statins after a 3-week trial? And that the original studies were funded by Pfizer? And that the ‘1.5 cases per 100k’ number is cooked? They don’t count the ones who die quietly at home, right?
Also, the CYP3A4 enzyme? It’s not just about grapefruit. It’s about glyphosate, air pollution, and your coffee mug. Everything’s poisoning your liver now. Statins are just the tip of the iceberg.
And why do they never mention that muscle breakdown releases toxins into your brain? That’s why people on statins get ‘brain fog’-it’s not aging, it’s myoglobin poisoning.
They want you to think you’re safe. But you’re not. You’re just waiting for the next dose to be your last.
Darcie Streeter-Oxland December 17, 2025
It is, of course, imperative to acknowledge that the incidence of rhabdomyolysis remains exceedingly rare, and the risk-benefit calculus overwhelmingly favors statin use in indicated populations. That said, the anecdotal evidence presented herein, while emotionally compelling, lacks the rigour of peer-reviewed epidemiological data. One would be prudent to consult a physician prior to discontinuing pharmacotherapy based upon internet commentary alone.
Christian Landry December 17, 2025
bro i got the slco1b1 test after my knee pain got bad on simva. turned out i had the tt/c variant. switched to pravastatin and now i can lift again. totally worth the $250.
also, if you’re gonna take a statin, don’t do it on an empty stomach. eat something. it helps.
Katie Harrison December 17, 2025
My mother was on simvastatin for 10 years. No issues-until she took clarithromycin. She collapsed. CK over 15,000. ICU for a week. Now she’s on ezetimibe. It’s not perfect, but it’s safe.
Don’t assume you’re fine because you haven’t had symptoms yet. Genetics, meds, age-they all stack up. Talk to your doctor. Get tested. Don’t wait for the worst.