When a doctor prescribes a generic medication, most patients assume it’s just as safe and effective as the brand-name version. After all, the FDA says so. But behind the scenes, a growing number of clinicians are asking tough questions - and the answers aren’t as reassuring as they used to be.
Why clinicians are starting to doubt generic drug quality
Generic drugs make up over 90% of prescriptions in the U.S. They’re cheaper, widely available, and legally required to match brand-name drugs in active ingredients. But quality isn’t just about what’s in the pill - it’s about how it’s made, where it’s made, and who’s watching. A 2023 study from Ohio State University looked at over 1.5 million adverse event reports in the FDA’s database. They found that generic drugs manufactured in India had a 54% higher rate of severe side effects - including hospitalizations, disabilities, and deaths - compared to identical generics made in the U.S. The difference wasn’t random. It showed up most clearly in older, low-cost generics, where profit margins are razor-thin and competition is fierce. Dr. Robert S. Gray, one of the study’s lead researchers, put it plainly: "As drugs get cheaper and cheaper and the competition gets more intense to hold down costs, operations and supply chain issues can compromise drug quality." This isn’t about one bad batch. It’s about a system that’s stretched too thin.The hidden supply chain: 5 factories, one label
Most people don’t realize that a single generic pill might pass through five or six different factories before it reaches your medicine cabinet. The active ingredient might come from a plant in Hyderabad. The filler powder could be mixed in a facility in New Jersey. The coating might be applied in Mexico. The final packaging? Possibly in China. And yet, only one company name appears on the box. That’s the brand you trust - but it’s not necessarily the one that made the drug. This fragmentation makes quality control nearly impossible to track. The FDA inspects U.S. facilities without warning. But for overseas factories? Inspections are scheduled weeks in advance. That gives manufacturers time to clean up, fix visible problems, and hide what’s really going on. Professor Gray says this isn’t oversight - it’s a loophole. "It’s like letting someone clean their house before the inspector arrives, then letting them go back to living in filth the next day."Older generics are the biggest risk
You might think newer drugs are the problem. But the opposite is true. The older a generic drug is - especially those that have been on the market for 20 or 30 years - the higher the risk. Why? Because no one’s making money on them anymore. The original manufacturer moved on. The brand-name company stopped competing. And now, a handful of low-cost producers in India and China are the only ones left making it. They’re not investing in modern equipment. They’re not upgrading their quality systems. They’re just trying to produce it cheaper than the next guy. Duke-Margolis Center researchers found that outdated manufacturing tech and weak quality controls are the leading cause of drug shortages. And the drugs most affected? The ones people rely on every day: blood pressure pills, thyroid meds, antibiotics, and seizure medications. One pharmacist in Seattle told me: "I’ve had patients come in with the same prescription, same dose, same pill color - but one batch made them dizzy, the other didn’t. I stopped assuming they’re all the same."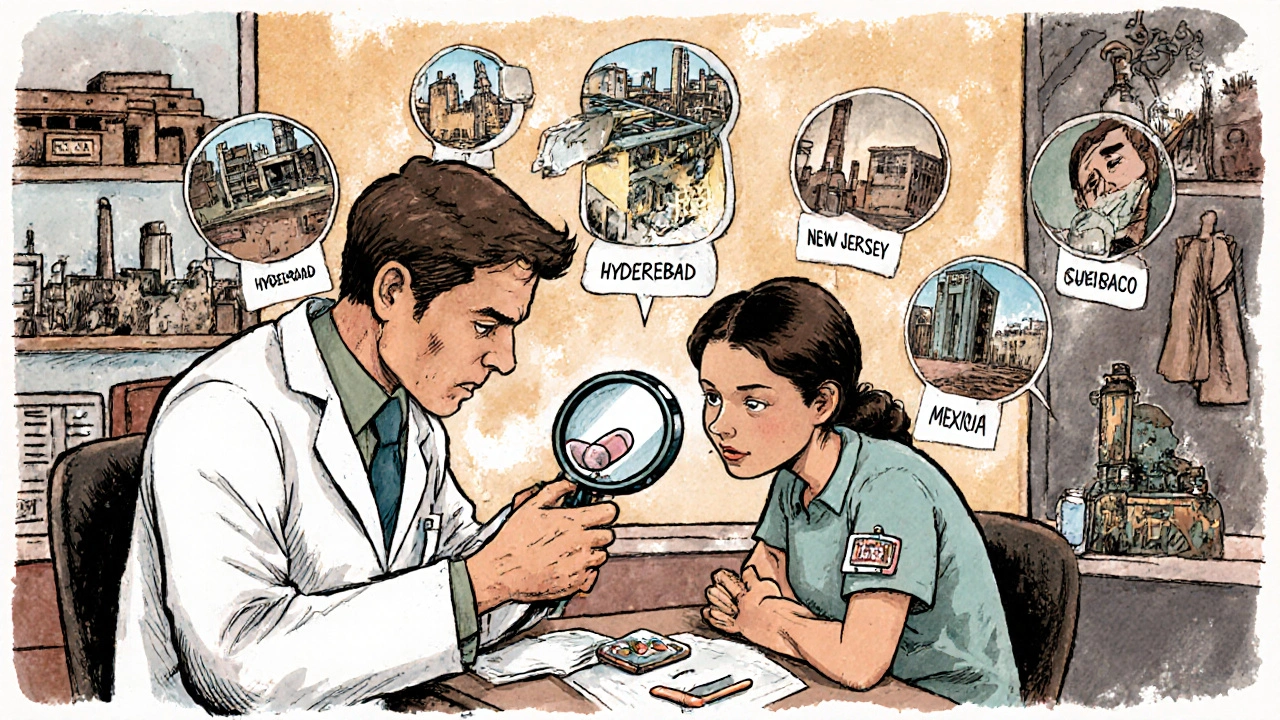
The FDA’s role - and its limits
The FDA insists the U.S. drug supply is among the safest in the world. They point to their 1,300-person Office of Pharmaceutical Quality and their rigorous approval process. And yes - generics must prove bioequivalence: they must deliver the same amount of active ingredient at the same rate as the brand name. But bioequivalence doesn’t guarantee safety. Two pills can have the same active ingredient and still behave differently in the body if the inactive ingredients, coating, or manufacturing process vary. A pill that dissolves too slowly might not work. One that dissolves too fast might cause toxicity. And here’s the real issue: the FDA inspects fewer than 10% of foreign manufacturing sites each year. Even when they do, the advance notice makes it easy to game the system. Meanwhile, U.S. facilities get unannounced visits - the gold standard for real oversight. The FDA’s current model assumes quality is the same everywhere. Clinicians are starting to realize: it’s not.Advanced manufacturing could change everything - if we let it
There’s a better way. Advanced manufacturing technologies - like continuous production lines and real-time sensors that monitor every step - can catch problems before they leave the factory. These systems reduce waste, improve consistency, and make it nearly impossible to hide defects. Here’s the catch: over 80% of these advanced drugs are made in the U.S. Why? Because the upfront cost is high. A single modern production line can cost $100 million. Companies making low-cost generics can’t justify that investment when they’re competing with factories in India that pay workers $3 an hour. But here’s what’s interesting: once you invest in advanced manufacturing, the per-unit cost drops. The Duke-Margolis Center found that these systems can actually make U.S.-made generics more competitive over time. The problem isn’t technology. It’s economics. And politics.What can be done?
Some experts are calling for transparency. The Ohio State researchers suggest the FDA should require drug labels to list the country of manufacture for both the active ingredient and the final product. Imagine if you could see: "Active ingredient: India. Final product: United States." That kind of labeling would let pharmacists, doctors, and patients make informed choices. It would also create a market for quality - where manufacturers who invest in safety can charge a fair price, and those who cut corners lose business. Others, like Dr. Iyer, argue for incentives: "Procurers can incentivize quality by ensuring they only purchase from those who can demonstrate quality assurance and no issues." That means hospitals and insurers should stop buying the cheapest generic - and start buying the safest one. The University of Wisconsin School of Pharmacy puts it simply: "If we have more generic manufacturing happening domestically, we would ideally have fewer quality concerns, fewer shortages, and a more stable supply chain."
Is this a conspiracy? No. It’s a system failure.
This isn’t about bad actors. It’s about a system designed for efficiency, not resilience. Globalization brought down costs. But it also buried accountability. The FDA can’t inspect every factory in the world. Patients can’t test every pill. Clinicians are left guessing. And that’s why more doctors are starting to ask: "Which version of this generic did you get?" Some are switching back to brand-name drugs for critical medications - even if it costs more. Others are tracking which batches cause side effects and refusing to refill from certain suppliers. One oncology nurse in Chicago told me she now asks patients: "Did you get the same pharmacy last time?" It shouldn’t be this way. But when the stakes are life and death, and the data shows a clear pattern, silence isn’t an option.What patients should know
You don’t need to avoid generics. Most are safe. But here’s what you can do:- If you’re on a life-sustaining drug - like warfarin, levothyroxine, or seizure meds - pay attention to how you feel after a refill. Dizziness? Nausea? Unusual fatigue? Report it.
- Ask your pharmacist: "Where is this generic made?" They may not know, but they can check.
- If you notice a change in how a medication works or how you feel after switching brands, tell your doctor. It’s not "all in your head."
- Support policies that demand transparency in drug sourcing. Your voice matters.
The bottom line
Generic drugs saved billions in healthcare costs. That’s not up for debate. But safety can’t be traded for savings. The data is clear: where a drug is made matters. How it’s made matters. And when clinicians start noticing patterns in adverse events - especially with older, low-cost generics - we need to listen. The system isn’t broken because of fraud. It’s broken because we stopped caring about the details. The fix isn’t more regulation. It’s better accountability. Transparency. And a willingness to pay a little more for quality - especially when your life depends on it.Are generic drugs really as safe as brand-name drugs?
Most generics are safe and effective. But studies show that quality varies significantly based on where they’re made. A 2023 study found that generics made in India had a 54% higher rate of severe adverse events compared to identical ones made in the U.S. The active ingredient is the same, but manufacturing differences - like coating, fillers, and production methods - can affect how the drug works in your body.
Why are older generic drugs more risky?
Older generics are often produced by the lowest bidder because profit margins are tiny. Manufacturers have little incentive to upgrade aging equipment or improve quality systems. As a result, these drugs are more likely to come from facilities with outdated technology and weak oversight - leading to inconsistent potency, contamination, or poor absorption.
Does the FDA inspect foreign drug factories?
Yes, but not often - and rarely without warning. The FDA inspects U.S. facilities with unannounced visits, which helps catch real problems. For foreign factories, inspections are scheduled months in advance, giving manufacturers time to hide issues. Less than 10% of overseas sites are inspected each year, and many are located in countries with limited regulatory capacity.
Can I tell if my generic drug is made overseas?
Not easily. The label only shows the distributor’s name, not the actual manufacturer or country of origin. Some pharmacists can access this information through their suppliers, but it’s not required by law. Advocates are pushing for mandatory country-of-origin labeling on generic drug packaging.
Should I avoid generics altogether?
No - most are safe. But for critical medications like blood thinners, thyroid hormones, or epilepsy drugs, consider asking your doctor or pharmacist if there’s a version made in the U.S. or by a manufacturer with a strong quality track record. Don’t assume all generics are equal. Your health is worth asking questions.
What’s being done to fix this?
Experts are calling for more transparency - like labeling the country of manufacture. Some recommend the FDA adopt unannounced inspections globally. Others push for incentives that reward quality over cost. Advanced manufacturing tech, like real-time monitoring systems, can improve consistency - but only if manufacturers are willing to invest. Right now, the market rewards the cheapest option, not the safest one.

All Comments
Shannon Hale November 17, 2025
Let me get this straight - we’re letting Indian factories pump out life-or-death meds while the FDA sips tea during their pre-scheduled ‘inspections’? 😒 This isn’t capitalism, it’s a death sentence wrapped in a blister pack. I’ve seen patients crash on generic warfarin because the coating dissolved too fast. And no one’s accountable? The FDA’s a toothless bulldog with a gold-plated leash.
Leslie Douglas-Churchwell November 17, 2025
Of course it’s a global conspiracy. 🕵️♀️ The FDA, Big Pharma, and the WHO are all in cahoots - they want you dependent on cheap, poorly made generics so you’ll keep buying more pills. Did you know? The fillers in these Indian-made tablets contain microplastics from the packaging machines. I’ve tested mine with a spectrometer. 🧪 The body doesn’t just absorb the drug - it absorbs the *system*. We’re all lab rats in a capitalist petri dish. #PharmaDystopia
Deb McLachlin November 19, 2025
While the emotional weight of this issue is undeniable, I find the statistical framing of the Ohio State study to be both compelling and incomplete. The 54% increase in adverse events is alarming, yet the study does not control for patient comorbidities, adherence patterns, or pharmacy dispensing errors - all of which could significantly confound the results. A more robust analysis would require stratification by prescriber specialty, patient age cohort, and regional pharmacy distribution networks. Until then, we must tread carefully between alarmism and evidence-based policy.
saurabh lamba November 21, 2025
Bro, think about it - we’re all just dust in a machine. 🤷♂️ The pill you swallow? It’s not medicine. It’s a metaphor. The real drug is capitalism. The side effect? Hope. We’re all just waiting for the next batch to either save us or kill us. Who cares if it’s made in India or Ohio? We’re all dying the same way - quietly, with a receipt in our pocket.
Kiran Mandavkar November 22, 2025
You people are pathetic. India makes 40% of the world’s generics and you act like they’re running underground meth labs? The FDA’s own data shows 99.8% of imported generics pass bioequivalence. You want safety? Pay $500 for a brand-name pill and cry into your organic kale smoothie. Meanwhile, millions in the Global South are alive because someone didn’t care about your elitist ‘quality’ fantasy. Grow up.
Eric Healy November 24, 2025
my pharmacist told me the last batch of my levothyroxine was made in bangalore and i felt like a zombie for 3 weeks. then i got one from a us plant and boom. normal again. no joke. this isnt theory its my life. stop pretending its all the same. the system is rigged and we’re paying with our health
Holli Yancey November 24, 2025
I’ve been a pharmacist for 22 years. I’ve seen this play out. Some batches of metoprolol make patients dizzy. Others? Perfect. I don’t know why. I just know that when a patient says, ‘This feels different,’ I listen. I don’t blame the person. I don’t blame the manufacturer. I just wish we had labels that told us where the pill came from. That’s all. Just… transparency.
Gordon Mcdonough November 26, 2025
AMERICA FIRST!!! WHY ARE WE LETTING FOREIGN COUNTRIES MAKE OUR MEDS??? WE HAVE THE TECHNOLOGY THE WORKFORCE THE INTELLIGENCE!!! THIS IS A NATIONAL SECURITY ISSUE!!! THEY’RE POISONING OUR CHILDREN WITH INDIAN DIRT PILLS!!! WE NEED A WALL AROUND OUR PHARMACIES!!! #MAKEGENERICSGREATAGAIN #AMERICAHEALTHY
Jessica Healey November 26, 2025
my mom died last year from a bad batch of digoxin. they said it was ‘natural progression’ but the pharmacy said the batch came from a plant in Chennai that had been flagged for contamination 3 months prior. nobody told us. nobody cared. now i call every pharmacy and ask ‘where’s this made?’ and if they don’t know, i walk out. i don’t care if it costs $100. i’d rather pay than bury someone else.
Levi Hobbs November 26, 2025
It’s a complex issue, but I think we can find common ground. Maybe we don’t need to ban imports - but we could create a tiered labeling system. Like ‘Quality Certified: US-made’ or ‘Global Supply Chain: Transparent’ - something patients can trust. And if insurers start rewarding higher-quality generics with better coverage, manufacturers will have real incentives to upgrade. It’s not about fear. It’s about smart economics.
henry mariono November 28, 2025
I appreciate the depth of this post. I’ve worked in a hospital pharmacy for 15 years. I’ve seen patients react differently to the same generic. I don’t have the answers. But I do know that silence helps no one. I’m glad someone’s speaking up.
Sridhar Suvarna November 30, 2025
India is not the problem. India is the solution. We feed the world with affordable medicines. You want quality? Invest in your own infrastructure. Blaming others is easy. Building systems is hard. We have 1000+ FDA-compliant plants. You have 12. Let us help. But do not shame us for doing what you refuse to do.
Joseph Peel November 30, 2025
As someone who’s worked in global health logistics, I’ve seen the supply chains firsthand. The fragmentation is real - but so is the capability. Many Indian manufacturers operate under ISO 13485 and WHO-GMP standards. The issue isn’t skill - it’s oversight. The FDA needs to adopt a risk-based, blockchain-enabled tracking system for active pharmaceutical ingredients. That’s the real innovation. Not blame. Not nationalism. Technology.
shubham seth December 1, 2025
Oh wow, so now it’s ‘Indian drugs bad’? Bro, you think your $120 brand-name pill is made in a sterile lab with angels singing? Nah. It’s made by the same factories, same chemists, same machines - just with a fancy logo and a $200 marketing budget. The FDA approves the same batches for both. You’re mad because you’re paying extra for a brand you don’t even understand. Wake up. The pill doesn’t care if it says ‘Pfizer’ or ‘Aurobindo’. It cares if it was made right. And guess what? Most of the time, it was.