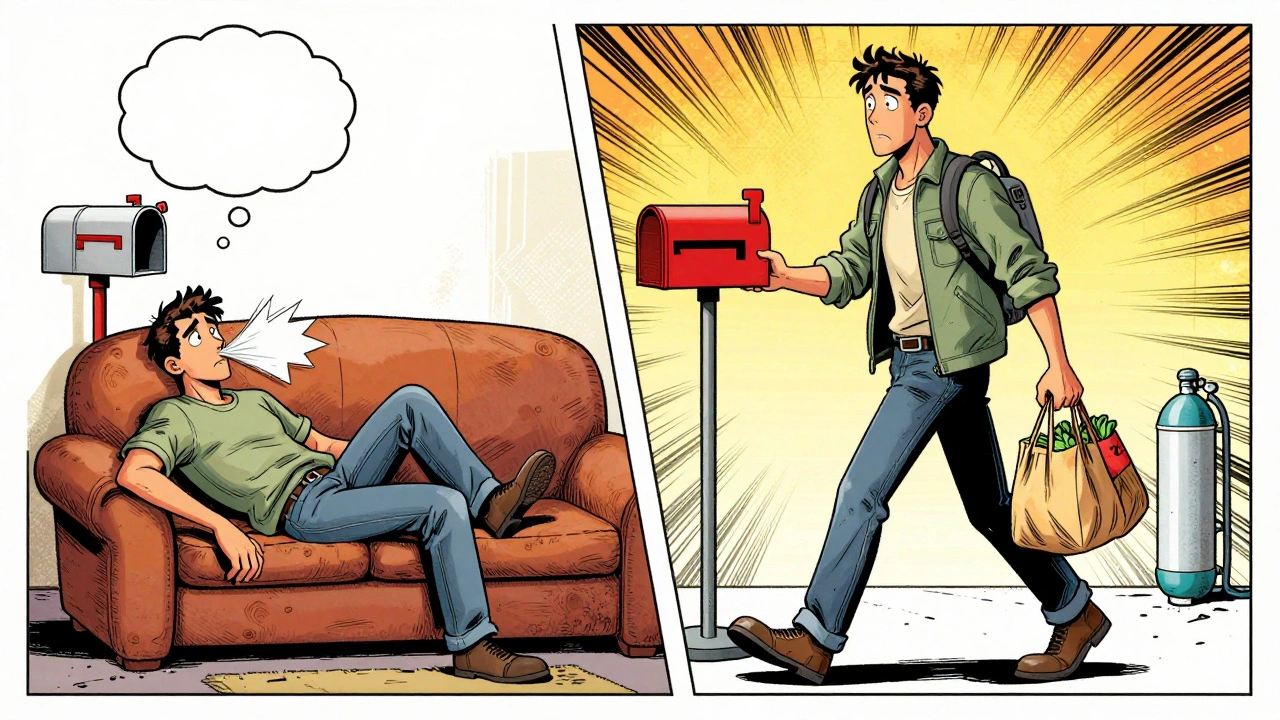
When you have a chronic lung disease like COPD, interstitial lung disease, or bronchiectasis, everyday tasks can feel impossible. Walking to the mailbox, carrying groceries, or even getting dressed leaves you breathless and exhausted. Medications help, but they don’t fix the weakness, the fear, or the isolation that comes with struggling to breathe. That’s where pulmonary rehabilitation changes everything.
What Pulmonary Rehabilitation Really Does
Pulmonary rehabilitation isn’t just exercise. It’s a full-time support system designed for people whose lungs no longer work the way they should. The American Thoracic Society and European Respiratory Society define it as a tailored program that combines exercise, education, and emotional support to help you live better with chronic lung disease. It’s not a quick fix - it’s a long-term strategy that gives you back control.
Studies show that after a 6- to 12-week program, people with moderate to severe COPD can walk 38.5 meters farther on the 6-minute walk test - that’s the distance of a football field. That’s not just a number. It means you can finally walk to the store without stopping. It means you can play with your grandkids without gasping. It means you stop feeling like your body is betraying you.
The Four Pillars of a Real Pulmonary Rehab Program
A quality pulmonary rehab program has four key parts, and skipping any one of them cuts your results in half.
- Exercise training - This isn’t just walking on a treadmill. It’s a mix of aerobic work (like cycling or walking) and strength training for your arms and legs. Sessions are built around your current ability, not someone else’s. If you can only walk 100 meters before stopping, that’s your starting point. The goal is to slowly push past that limit, safely. Most programs include resistance training using light weights or resistance bands, targeting muscles that help you breathe and move.
- Education - You’ll learn how your lungs work, what your medications actually do, how to recognize when you’re having a flare-up, and how to avoid triggers like smoke or cold air. Knowing what’s happening in your body reduces fear. Fear makes breathing harder. Education helps break that cycle.
- Psychological support - Anxiety and depression are common in people with chronic lung disease. You’re not alone if you feel this way. Rehab programs include counselors or psychologists who help you manage worry, sleep problems, and the loneliness that comes with being limited by your health.
- Regular monitoring - Your progress is tracked using tools like the 6-minute walk test and the St. George’s Respiratory Questionnaire. These aren’t just paperwork - they show you how far you’ve come. Seeing your numbers improve is a powerful motivator.
Who Can Benefit - It’s Not Just for COPD
Most people think pulmonary rehab is only for COPD. That’s outdated. The 2023 guidelines now recommend it for anyone with a chronic lung condition that limits their daily life. That includes:
- Interstitial lung disease (ILD)
- Pulmonary hypertension
- Bronchiectasis
- Cystic fibrosis
- People waiting for or recovering from a lung transplant
Even if your lung function test says you’re in the mild range, if you’re tired all the time, avoid stairs, or skip social events because you’re afraid of getting out of breath - you’re a candidate. The European Respiratory Society says: if you’re limited by symptoms, you deserve rehab, no matter what your spirometry says.
How It Compares to Just Taking Pills
Medications like inhalers and steroids help open your airways. But they don’t rebuild muscle. They don’t teach you how to breathe better. They don’t give you confidence.
Here’s what the data shows:
| Outcome | Pulmonary Rehab Improvement | Medication Improvement (Bronchodilators) |
|---|---|---|
| Exercise capacity (6-minute walk test) | 38.5 meters | 17.2 meters |
| Dyspnea (breathlessness) | 0.8-point drop on MRC scale | 0.3-point drop |
| Quality of life (SGRQ score) | 8.7-point improvement | 4.1-point improvement |
Rehab doesn’t replace your inhalers - it makes them work better. You’re not just treating your lungs. You’re rebuilding your whole body’s ability to handle daily life.
Where You Can Get It - And the Big Problem
Most programs happen in outpatient clinics, hospitals, or rehab centers. But 78% of U.S. counties don’t have one. That’s a huge barrier. Even if your doctor recommends it, you might have to drive an hour or more to get there.
Telehealth rehab is changing that. A 2023 study in JAMA Network Open found that home-based programs using video calls and wearable monitors delivered results just as good as in-person sessions. You can do your exercises at home, get feedback from your therapist, and still track your progress.
But here’s the catch: only 3.2% of eligible patients in the U.S. actually complete a full program. Why? Three big reasons:
- Doctors don’t refer enough - many still don’t know rehab works.
- Transportation is hard - no car, no ride, no program.
- People think it’s too expensive - but Medicare covers 36 sessions a year.
Medicare pays $125 per session, but the real cost to run a program is closer to $180. That’s why many clinics struggle to stay open. You might have to wait for a spot. You might have to fight for a referral. But it’s worth it.
Real People, Real Results
One 68-year-old man in Cleveland had been stuck at home for five years. He couldn’t walk to the grocery store without needing oxygen. After 12 weeks of rehab, his 6-minute walk distance jumped from 182 meters to 327 meters. He started buying his own food again.
A woman on Reddit shared that after rehab, she went from needing 1 liter of oxygen all day to being off it during daily activities. She didn’t need it anymore - not because her lungs healed, but because her body learned to use what it had better.
89% of participants say their most meaningful win was being able to walk to the mailbox without stopping. That’s not a statistic. That’s dignity.

What to Expect When You Start
Getting started is easier than you think:
- Ask your doctor for a referral. If they say no, ask why. If they say it’s not covered, ask for a copy of the Medicare policy.
- Call the American Lung Association at 1-800-LUNGUSA. They can help you find a program near you.
- Be ready for an assessment. You’ll do a breathing test, a walk test, and answer questions about your daily life.
- Start slow. The first week is about learning, not pushing hard.
- Attend every session. Missing one session doesn’t ruin progress, but missing too many makes it harder to get back on track.
Most programs run 2-3 times a week for 6-12 weeks. You’ll have homework - breathing exercises, walking logs, journaling. It’s not optional. It’s part of the work.
What Happens After the Program Ends?
Rehab doesn’t end when the 12 weeks are over. That’s when the real work begins. The goal is to make these habits last. Many programs offer maintenance sessions once a week or monthly check-ins. Some people join local walking groups. Others keep using the home exercise plan they learned.
Studies show that people who keep exercising after rehab stay stronger, have fewer hospital visits, and live longer. One 2023 analysis found that rehab cut all-cause mortality by 18.2% in people who’d been hospitalized for COPD.
You’re not just getting better. You’re preventing worse.
Final Thoughts: It’s Not a Luxury - It’s a Lifeline
Pulmonary rehabilitation isn’t a second-choice treatment. It’s the most effective non-drug therapy we have for chronic lung disease. It’s not magic. It’s hard work. But it’s work that gives you back your life.
If you or someone you love has a chronic lung condition and struggles to breathe through daily tasks, don’t wait. Don’t assume it’s too late. Don’t think meds are enough. Ask about pulmonary rehab. Push for it. Find a program. Show up. Your future self will thank you.
Is pulmonary rehabilitation only for people with COPD?
No. While COPD is the most common reason, pulmonary rehab is now recommended for anyone with a chronic lung disease that limits daily life - including interstitial lung disease, pulmonary hypertension, bronchiectasis, cystic fibrosis, and even before or after a lung transplant. If you’re short of breath during normal activities, you’re likely a candidate.
Does Medicare cover pulmonary rehab?
Yes. Medicare covers up to 36 sessions over 12 weeks, with the possibility of 36 more if your doctor certifies medical necessity. Sessions must be supervised by qualified staff in an approved setting. You’ll pay your usual 20% coinsurance unless you have supplemental insurance.
How long does it take to see results from pulmonary rehab?
Most people start noticing changes in 4 to 6 weeks - less breathlessness during daily tasks, more energy, better sleep. The biggest gains in walking distance and quality of life typically happen by week 8 to 12. But the benefits last longer if you keep exercising after the program ends.
Can I do pulmonary rehab at home?
Yes. Telehealth pulmonary rehab has been proven just as effective as in-person programs for improving exercise capacity and reducing breathlessness. You’ll use video calls with therapists, wearables to track your heart rate and oxygen, and follow a personalized home plan. It’s a great option if travel is difficult.
What if my doctor won’t refer me to pulmonary rehab?
Many doctors still don’t know how effective rehab is. Bring printed guidelines from the American Thoracic Society or the Global Initiative for Chronic Obstructive Lung Disease (GOLD). Ask for a referral in writing. If your doctor refuses, contact the American Lung Association’s Lung HelpLine at 1-800-LUNGUSA - they can help you advocate for yourself and find programs that accept self-referrals.
Are there any risks with pulmonary rehab?
The risks are very low when done under supervision. Your program will start at your current ability and increase slowly. Staff monitor your heart rate, oxygen levels, and symptoms. If you feel dizzy, chest pain, or extreme shortness of breath, you’ll stop immediately. The biggest risk is not doing it - because without rehab, your strength and independence continue to decline.
For more support, visit the American Lung Association’s website or join the Pulmonary Wellness Foundation’s online community. You’re not alone in this journey.


All Comments
Deborah Jacobs December 5, 2025
After my husband started pulmonary rehab, he went from barely making it to the porch to walking two miles without stopping. I cried the first time he carried the groceries in himself. It wasn’t just about his lungs-it was about his soul coming back.
James Moore December 5, 2025
Let me tell you something-this whole 'pulmonary rehab' thing is just another government-funded boondoggle! In my day, people didn’t whine about breathing-they just breathed harder! We didn’t need fancy treadmills and therapists; we had grit! And now they want to hand out oxygen tanks like candy? I’ve seen this movie before-first it’s rehab, next it’s free oxygen for everyone who can’t climb stairs! It’s socialism disguised as healthcare!
Kylee Gregory December 7, 2025
I’ve been thinking a lot about how we define 'progress' in medicine. Is it just about how far someone walks? Or is it about the quiet dignity of being able to tie your own shoes without gasping? Rehab doesn’t cure-but it restores. And maybe restoration is the closest thing we have to healing these days.
Lucy Kavanagh December 7, 2025
Did you know that 78% of counties lack rehab centers? That’s not an accident. Big Pharma doesn’t want you getting stronger-they want you dependent on inhalers. And telehealth? That’s just the first step before they start implanting tracking chips in your chest to monitor your 'compliance.' I’ve seen the documents. They’re coming for your breath.
Michael Dioso December 8, 2025
Oh wow, another feel-good article about 'walking farther.' Congrats. Meanwhile, I’ve got a cousin who’s on oxygen 24/7 and still can’t walk to the fridge. Rehab? Sounds like a nice distraction for people who think exercise fixes everything. Spoiler: it doesn’t. Your lungs are broken. Accept it. And stop pretending a treadmill is a miracle.
Krishan Patel December 9, 2025
It is imperative to acknowledge that pulmonary rehabilitation is not merely a clinical intervention, but a moral imperative for those who have been abandoned by the capitalist healthcare apparatus. The fact that only 3.2% of eligible patients participate is not a failure of individual will-it is a systemic indictment. We must demand universal access, not because it is convenient, but because human dignity cannot be commodified.
sean whitfield December 10, 2025
Rehab. Sure. Next they’ll give you a pat on the back and a participation trophy for not dying on the couch.
Manish Shankar December 11, 2025
It is with profound respect for the medical community that I acknowledge the efficacy of pulmonary rehabilitation as outlined in this article. The structured, multidisciplinary approach aligns with the principles of holistic patient care, and the documented improvements in functional capacity are both statistically significant and clinically meaningful. I commend the authors for their thoroughness.
Katie Allan December 13, 2025
James, your rant about 'socialism' ignores the fact that Medicare covers this for a reason-it works. And Lucy, no, they’re not putting chips in your chest. That’s not how any of this works. This isn’t a conspiracy. It’s science. People are getting their lives back. You can’t argue with a man who walks to the store for the first time in five years.
Jimmy Jude December 15, 2025
I did rehab. It was great. I got better. Then my insurance dropped me. Now I’m back to gasping on the porch. So yeah, rehab works. But who cares? The system doesn’t. I’m just a statistic now. Thanks for the article. It made me cry. Again.
luke newton December 15, 2025
Everyone’s so excited about rehab, but no one talks about how it’s just a Band-Aid. You think walking farther means you’re healed? You’re not. You’re just delaying the inevitable. Meanwhile, your kids are paying for your oxygen. You think this is hope? It’s just guilt dressed up as progress.