Every year, millions of American men get a simple blood test called PSA screening. It’s meant to catch prostate cancer early. But here’s the problem: for every life it saves, it can cause a lot of unnecessary stress, biopsies, and even permanent side effects from treatments that weren’t needed. This isn’t just a medical debate-it’s a real-life dilemma for men and their doctors. And the answer isn’t more testing. It’s better conversations.
What PSA Screening Actually Measures-and Why It’s Flawed
The PSA test measures a protein made by the prostate gland. High levels can mean cancer, but they can also mean a swollen prostate, an infection, or even riding a bike too hard. That’s the core issue: the test isn’t specific. About 75% of men with a PSA between 4.0 and 10.0 ng/mL don’t have cancer, yet they still get sent for painful biopsies. Meanwhile, 15% of men with aggressive cancer have PSA levels under 4.0. That means the test misses some of the worst cases.
Doctors tried to fix this by adjusting the threshold based on age. For example, a 55-year-old with a PSA of 3.5 might be fine, but that same number for a 40-year-old could raise red flags. Even then, it’s not reliable. A 2021 study in European Urology showed that using PSA alone leads to over 100 false positives for every 1,000 men screened over 10 years. And for every 1,000 men screened, only 1 or 2 prostate cancer deaths are prevented. That’s a tiny benefit for a lot of risk.
The Big Studies That Changed Everything
In 2012, the U.S. Preventive Services Task Force (USPSTF) told doctors to stop routine PSA screening. Why? Two massive studies gave conflicting answers. The European study found a 21% drop in prostate cancer deaths with screening. But the U.S.-based PLCO trial showed no benefit at all. The difference? In the U.S. study, many men in the "no screening" group still got tested anyway, muddying the results. Still, the harm was clear: thousands of men were diagnosed with cancers that would never have hurt them. These are called "overdiagnosed" cancers. The Cochrane Collaboration estimates that 17% to 50% of all prostate cancers found through PSA screening fall into this category.
By 2018, the USPSTF changed its stance. Instead of saying "don’t screen," they said: "Screen only if you and your doctor talk about the risks and benefits." That’s the shift to shared decision-making. It’s not about whether screening works-it’s about whether it’s the right choice for you.
What Happens After a High PSA?
If your PSA is high, the next step used to be a biopsy. Now, it’s not that simple. Many doctors are using multiparametric MRI (mpMRI) first. This non-invasive scan can show if a tumor is likely to be aggressive. The PRECISION trial found that using MRI before biopsy cut unnecessary biopsies by 27% without missing dangerous cancers.
There are also newer blood tests like the 4Kscore and urine tests like PCA3. They look at multiple markers, not just PSA. The 4Kscore, for example, combines four different proteins with your age and family history. A 2018 study showed it correctly identifies 95% of men who are at low risk for high-grade cancer. That means fewer men get scared or treated for something harmless.
And if cancer is found? Not every case needs surgery or radiation. Active surveillance-where doctors monitor the cancer with regular PSA tests and MRIs-is now standard for low-risk cases. The ProtecT trial showed that after 10 years, survival rates were the same whether men had surgery, radiation, or just watched the cancer. That’s huge. It means many men can avoid incontinence, erectile dysfunction, and other side effects without risking their lives.
Why Shared Decision-Making Isn’t Just a Buzzword
Shared decision-making isn’t about handing a pamphlet to a patient and saying, "You decide." It’s a structured conversation. A 2022 study at Mayo Clinic found that primary care doctors spend just 3.7 minutes on average talking about PSA screening. That’s not enough. The American College of Physicians says you need 15 to 20 minutes to cover the real trade-offs.
What should that conversation include? Three things:
- How many men benefit? (About 1-2 out of 1,000 screened avoid death from prostate cancer)
- How many get harmed? (About 100 get false positives, 80-100 get cancers they don’t need to treat)
- What are the alternatives? (MRI, newer blood tests, active surveillance)
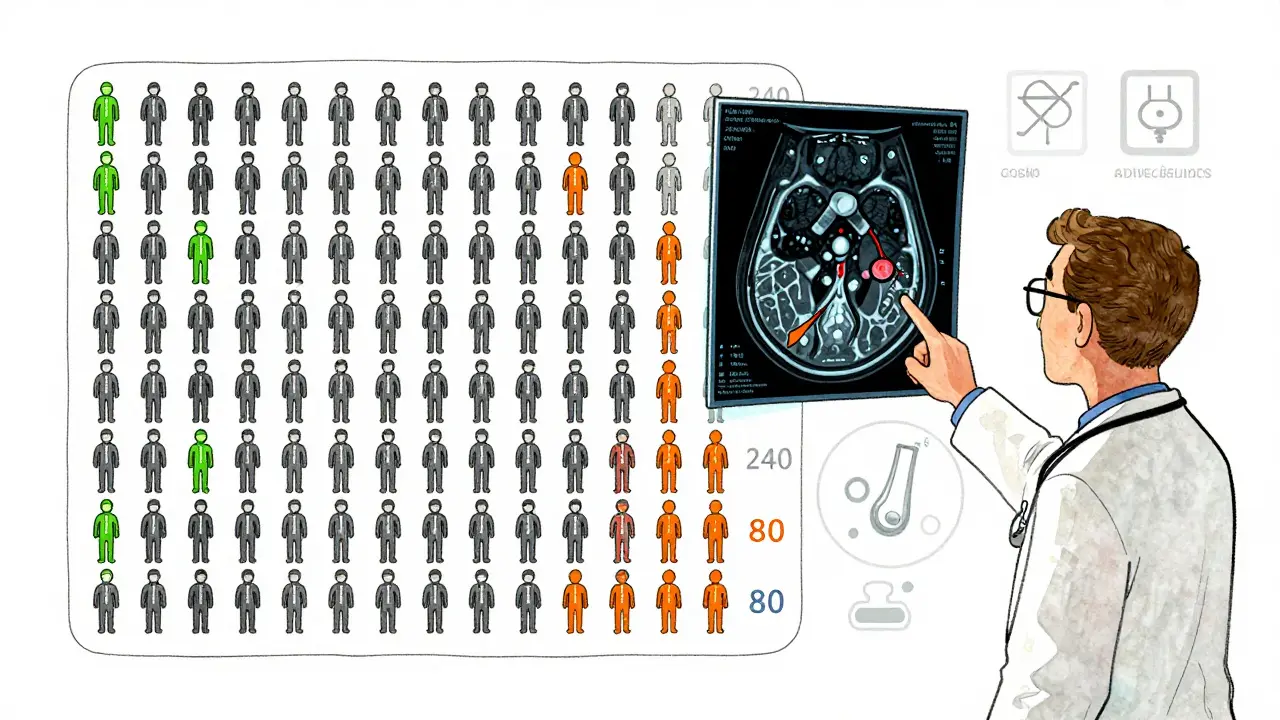
Decision aids help. The Mayo Clinic’s tool uses simple visuals: a grid showing 1,000 men. One box is colored to show who avoids death. Two hundred and forty boxes show who get unnecessary biopsies. It’s eye-opening. Studies show these tools reduce decision-making stress by 35%.
Who’s at Highest Risk-and Who Might Not Need Screening
Not all men are the same. African American men have more than double the risk of dying from prostate cancer compared to white men. Yet, a 2022 study found they’re 23% less likely to have a real discussion about screening. That’s a gap that needs closing.
On the flip side, some men have almost no risk. If a man has a PSA under 1.0 ng/mL at age 45-50, his chance of dying from prostate cancer in the next 20 years is less than 1%. Dr. Peter Carroll at UCSF says these men can safely wait 10 years before testing again. That’s a game-changer for men who want to avoid unnecessary testing.
And what about men over 70? The USPSTF says the harms outweigh the benefits. Most prostate cancers grow slowly. If you’re 75, you’re more likely to die with prostate cancer than from it. Screening at that age rarely helps-and often causes harm.

What’s Changing in 2026?
The future of PSA screening isn’t more tests. It’s smarter ones. The FDA approved IsoPSA in 2021, a new version of the PSA test that claims 92% accuracy for detecting aggressive cancer-compared to just 25% for the old one. That’s a big leap.
Artificial intelligence is stepping in too. MIT researchers built an algorithm that looks at routine blood test data and predicts prostate cancer risk with 85% accuracy. It could cut unnecessary PSA tests by 30%. Meanwhile, the National Cancer Institute’s P4 study is testing whether measuring PSA once at age 45 can identify who needs lifelong monitoring and who doesn’t.
Genetic testing is also becoming part of the picture. The BARCODE1 study found that men with certain inherited gene mutations benefit far more from screening. In the future, your risk might be calculated based on your DNA, your PSA, your family history, and your race-all together.
What Should You Do?
Here’s the bottom line:
- If you’re under 40, don’t get screened unless you have a strong family history or genetic risk.
- If you’re 40-54, talk to your doctor about your risk. If your PSA is under 1.0, you can likely wait until 50.
- If you’re 55-69, this is the age group where screening might help. But only if you understand the trade-offs. Ask for a decision aid. Ask about MRI before biopsy. Ask about active surveillance.
- If you’re 70 or older, screening is unlikely to help. Focus on quality of life, not extra tests.
Don’t let fear or silence make the decision for you. Ask your doctor: "What are the chances this test will help me live longer? What are the chances it will lead to treatment I don’t need?" If they can’t answer clearly, ask for a referral to a urologist or a decision aid. You deserve to know what you’re signing up for.
Why This Matters More Than You Think
PSA screening isn’t just about a blood test. It’s about how medicine treats men’s health. For decades, men were told to get tested because it "might save your life." No one told them it might ruin your sex life, your bladder control, or your peace of mind. Now, we’re moving toward a better model: personalized, informed, and respectful.
Men are living longer. Prostate cancer is often slow. We don’t need to treat every case. We need to treat the right cases-and leave the rest alone. That’s what shared decision-making is for. It’s not about avoiding the test. It’s about making sure the test is worth it-for you.
Is PSA screening still recommended for men over 70?
No. The U.S. Preventive Services Task Force (USPSTF) recommends against PSA screening for men 70 and older. Most prostate cancers grow slowly, and men in this age group are more likely to die from other causes than from prostate cancer. Screening at this age rarely improves survival but often leads to unnecessary biopsies, treatments, and side effects like incontinence or erectile dysfunction. The harms outweigh the benefits.
What’s the difference between overdiagnosis and overtreatment?
Overdiagnosis means finding a cancer that would never have caused symptoms or shortened life. These are slow-growing tumors that might never spread. Overtreatment is what happens after overdiagnosis-when men get surgery, radiation, or hormone therapy for a cancer they didn’t need to treat. Both are common with PSA screening. Studies estimate that 17% to 50% of prostate cancers found through screening are overdiagnosed, and most of those lead to overtreatment.
Are newer tests like 4Kscore or IsoPSA better than regular PSA?
Yes, they’re more accurate. Traditional PSA has a high false-positive rate-about 75% of men with PSA levels between 4.0 and 10.0 don’t have cancer. The 4Kscore combines four different proteins with age and family history to better predict aggressive cancer risk. IsoPSA, approved in 2021, measures a different form of PSA and claims 92% accuracy for detecting high-grade cancer, compared to just 25% for standard PSA. These tests reduce unnecessary biopsies and help avoid treating harmless cancers.
Why are African American men at higher risk, and are they getting better care?
African American men have a 70% higher chance of being diagnosed with prostate cancer and more than double the death rate compared to white men. The reasons include genetics, access to care, and possible biological differences in tumor behavior. Unfortunately, a 2022 study found they’re 23% less likely to have a shared decision-making conversation before getting screened. This gap in communication contributes to both underuse and misuse of screening in this high-risk group.
Can I avoid a biopsy if my PSA is high?
Yes. Many doctors now use multiparametric MRI (mpMRI) before recommending a biopsy. If the MRI shows no signs of aggressive cancer, you may avoid the biopsy entirely. If it shows a suspicious area, doctors can target the biopsy to that spot, making it more accurate and less invasive. The PRECISION trial showed this approach cuts unnecessary biopsies by 27% without missing dangerous cancers.
What is active surveillance, and is it safe?
Active surveillance means monitoring a low-risk prostate cancer with regular PSA tests, MRIs, and occasional biopsies-instead of immediately treating it with surgery or radiation. The ProtecT trial, which followed over 1,600 men for 10 years, found that survival rates were nearly identical between men who chose active surveillance, surgery, or radiation. For men with low-risk cancer, active surveillance is now the standard of care. It avoids side effects like incontinence and impotence while still catching any changes early.
How long should a shared decision-making conversation take?
Experts from the American College of Physicians recommend 15 to 20 minutes for a full shared decision-making discussion. This includes explaining the benefits, risks, and alternatives, answering questions, and using decision aids. In practice, most primary care visits only last 3.7 minutes for PSA screening, which is far too short. If your doctor rushes you, ask for more time, or request a referral to a urologist or a decision aid tool.
Do I need to get screened every year?
No. Annual screening is outdated. For men who decide to screen, most guidelines now recommend testing every 2 years, or even less frequently. Men with low PSA levels (under 1.0 ng/mL) at age 45-50 may only need testing every 5-10 years. The goal isn’t frequent testing-it’s smart, personalized monitoring based on your risk level and PSA trend over time.