What Is Peripheral Neuropathy?
Peripheral neuropathy isn't one disease-it's a group of conditions caused by damage to the nerves outside your brain and spinal cord. These nerves control sensation, movement, and even automatic functions like digestion. When they get damaged, you might feel tingling, burning, or sharp pain, usually starting in your feet or hands. Over 20 million Americans live with this condition, and for many, it’s linked to something preventable or treatable.
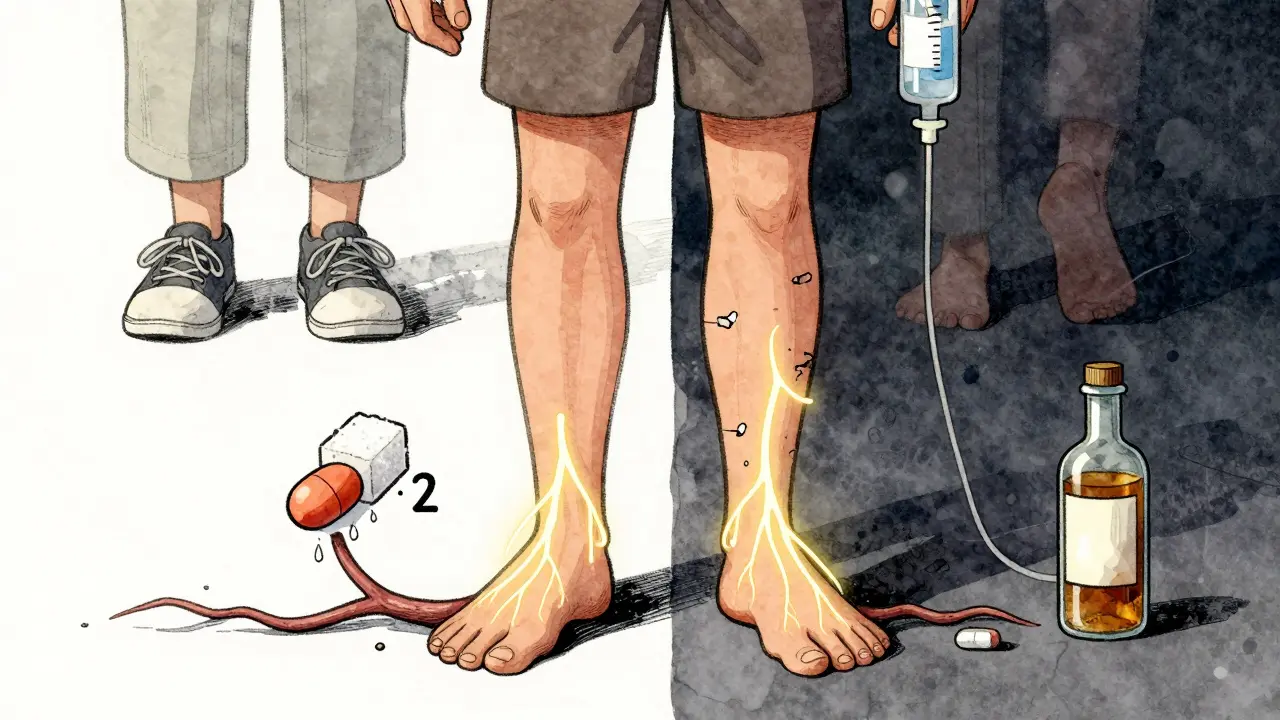
Diabetes is the biggest culprit. About half of all people with diabetes develop some form of nerve damage over time. But it’s not the only cause. Vitamin B12 deficiency, chemotherapy, alcohol misuse, autoimmune disorders, and even certain infections can trigger it. In about 20% of cases, doctors can’t find a clear cause-these are called idiopathic neuropathies.
Symptoms don’t show up overnight. They creep in slowly. You might notice your toes going numb, or your feet feeling like they’re wrapped in plastic. Walking becomes tricky because you can’t feel the ground. Some people describe it as a constant electric buzz or a burning sensation that won’t quit. At night, it can wreck sleep. The pain isn’t just discomfort-it changes how you live.
Why Do Nerves Get Damaged?
Not all nerve damage is the same. The type depends on what’s causing it and how many nerves are involved. Most people (75%) have polyneuropathy-widespread damage affecting nerves symmetrically, usually starting in the feet. Others have mononeuropathy, where just one nerve is hurt, like in carpal tunnel syndrome.
High blood sugar is the #1 enemy. When glucose levels stay elevated, it damages the tiny blood vessels that feed nerves. Without proper blood flow, nerves starve and start misfiring. That’s why keeping your HbA1c below 7% cuts the risk of nerve damage by 60%, according to long-term studies like the DCCT.
Vitamin B12 is another silent killer. It’s essential for nerve repair. A deficiency-common in older adults, vegans, or people on metformin-can cause numbness, balance issues, and even memory problems. A simple blood test can catch this early. If found, a weekly B12 injection can reverse symptoms in weeks.
Chemotherapy drugs like paclitaxel and vincristine are notorious for damaging nerves. Up to 40% of cancer patients on these drugs develop neuropathy. It’s often unavoidable, but doctors can adjust doses or switch medications if symptoms get too bad.
Other causes include chronic alcohol use (which strips away vital nutrients), autoimmune diseases like Guillain-Barré or lupus, and even some inherited disorders like Charcot-Marie-Tooth disease. Infections such as shingles or Lyme disease can also attack nerves directly.
How Is It Diagnosed?
Getting a diagnosis can take time-on average, 18 months from first symptoms. Many people are told it’s just aging or stress. But there are real tests that show what’s happening inside your nerves.
The most common is the nerve conduction study. Electrodes are placed on your skin, and tiny electrical pulses are sent through your nerves. If the signal travels slower than 40 meters per second, that’s a red flag. Another test, quantitative sensory testing, measures how well you feel heat, cold, or vibration-often using a 128-Hz tuning fork on your big toe.
Doctors also check your reflexes, muscle strength, and balance. A simple test called the “timed up and go” measures how fast you can stand from a chair, walk 3 meters, turn, and sit back down. Slower times mean higher fall risk.
Blood tests are routine: glucose, HbA1c, B12, thyroid function, kidney and liver markers. If something stands out, you might get an EMG (electromyography) or even a nerve biopsy-though that’s rare.
Early diagnosis matters. If you start treatment within the first six months of symptoms, your chances of stopping further damage jump by 40%.
Medications That Actually Work
Over-the-counter painkillers like ibuprofen or acetaminophen? They barely touch neuropathic pain. You need drugs that target nerve signals, not inflammation.
Pregabalin (Lyrica) is a first-line choice. It works for about 37% of users, cutting pain by half. But it comes with side effects-dizziness, weight gain, and brain fog. Many people say it helps, but they can’t drive at first.
Duloxetine (Cymbalta) is an antidepressant that’s also FDA-approved for nerve pain. It helps 35% of people, but nausea is common in the first two weeks. Some quit because of it.
Amitriptyline, an older tricyclic antidepressant, is still widely used. It gives 50% pain relief in 41% of patients. But dry mouth affects 75% of users, and drowsiness is nearly universal. It’s cheap and effective, but not for everyone.
There’s also Qutenza, a patch with high-dose capsaicin. Applied once every 3 months in a doctor’s office, it numbs the nerve endings. Clinical trials show 31% pain reduction after 12 weeks. It’s not a cure, but for some, it’s a game-changer.
And then there’s the opioid trap. Studies show opioids only help 30% of neuropathy patients-and 15% end up addicted. Most experts now say: avoid them unless everything else fails.
Non-Drug Ways to Manage Pain
Medications aren’t the only answer. In fact, combining them with lifestyle changes gives the best results.
Scrambler therapy is one of the most promising. It uses mild electrical signals to “trick” your brain into thinking it’s not in pain. After 10 sessions, 85% of patients report 50% less pain. It’s expensive-$1,200 to $1,500 per course-but many insurance plans cover it now.
Spinal cord stimulation is another option for severe, stubborn pain. A tiny device is implanted near your spine and sends pulses that block pain signals. It works for 65% of people who’ve tried everything else.
Physical therapy is underrated. A 12-week program focused on balance, strength, and coordination can reduce fall risk by 30%. Simple exercises like standing on one foot, heel-to-toe walking, or using a balance board make a real difference.
Custom orthotics and therapeutic shoes? They’re not optional. If your feet are numb, you won’t feel blisters or sores. Special shoes with cushioned soles and wide toes prevent ulcers. One study found 82% satisfaction among users.
And don’t underestimate foot care. Check your feet twice a day-look for cuts, redness, swelling. Wash them daily, dry thoroughly, and moisturize (but not between toes). Wear socks to bed if your feet get cold. These steps prevent infections that can lead to amputations.

What You Can Do Right Now
If you have peripheral neuropathy, here’s what to do today:
- Get your blood sugar under control-if you’re diabetic, aim for HbA1c under 7%. Even small drops help.
- Ask for a B12 test-it’s cheap, easy, and reversible.
- Start walking daily-even 15 minutes improves circulation and nerve function.
- Stop smoking-it narrows blood vessels and cuts off oxygen to nerves.
- Limit alcohol-even moderate drinking can worsen damage.
- Use a mirror to check your feet-you can’t feel everything, but you can see it.
- Ask about scrambler therapy-if meds aren’t working, it’s worth a try.
Don’t wait for your next appointment. If you’re losing balance, struggling to walk, or in constant pain, speak up. Your doctor can refer you to a neurologist or a pain specialist. You don’t have to live like this.
What’s Coming Next?
The future of neuropathy treatment is moving fast. The FDA approved Qutenza in 2020, but newer options are on the horizon. Wearable nerve stimulators are in late-stage trials-they’ll deliver gentle pulses all day to keep pain at bay.
Gene therapy is being tested for inherited forms like Charcot-Marie-Tooth. Early results show nerve conduction improving by 20% in six months. And the Neuropathy Genomics Project, launched in early 2023, aims to map genetic causes of over 50 types of neuropathy by 2026.
AI tools are being trained to spot early nerve damage from simple foot scans or gait analysis. By 2025, diagnosis time could drop from 18 months to under six. That means earlier treatment-and better outcomes.
Big pharma is investing heavily. The global market for neuropathy treatments is projected to hit $5.8 billion by 2028. More options are coming, but the core message stays the same: treat the cause, manage the pain, and protect your nerves before it’s too late.
Frequently Asked Questions
Can peripheral neuropathy be reversed?
In some cases, yes-if the cause is treatable. If it’s from vitamin B12 deficiency, diabetes, or alcohol use, fixing the root problem can improve or even reverse nerve damage, especially if caught early. But if nerves are severely damaged or the cause is unknown, full recovery is unlikely. The goal shifts to stopping further damage and managing symptoms.
Is neuropathy pain constant or does it come and go?
It varies. Some people have constant burning or tingling. Others get waves of pain-worse at night or after standing for long periods. In early stages, symptoms might be mild and intermittent. As damage grows, it becomes more steady. Tracking when pain flares can help your doctor adjust treatment.
Can I still drive with peripheral neuropathy?
It depends. If your feet are numb, you might not feel the pedals properly. Some people can drive safely with custom insoles or modified pedals. Others need to stop. If you’re dizzy from medication or have trouble sensing the gas or brake, it’s unsafe. Talk to your doctor and consider a driving assessment.
Do I need to see a specialist?
Yes-if you haven’t already. A neurologist can confirm the diagnosis and rule out other conditions. A pain specialist can help if medications aren’t working. A podiatrist can prevent foot injuries. And if you’re diabetic, an endocrinologist can optimize your glucose control. You don’t have to manage this alone.
What happens if I ignore it?
Ignoring it can lead to serious complications. Numb feet mean you won’t feel cuts or blisters. Those can turn into infections, ulcers, and even amputations. Poor balance increases fall risk-hip fractures are common. Untreated neuropathy also affects your mood, sleep, and ability to work. The longer you wait, the harder it is to regain function.

All Comments
Ryan van Leent December 17, 2025
I've had this for years and none of this stuff works. Just take oxycodone and call it a day. Who cares if you're addicted when your feet feel like they're on fire 24/7?
Sajith Shams December 18, 2025
You people are clueless. Diabetes isn't even the main cause. It's glyphosate in your food. Monsanto ruined your nerves. B12? Please. You need chelation therapy and bentonite clay. I've been researching this since 2012 and no doctor will admit it.
Adrienne Dagg December 18, 2025
This is so helpful!! 🙌 I just got diagnosed last week and was about to cry. B12 test?? I didn't even know that was a thing. Going to my doc tomorrow. Also low carb life for life 🥑
Erica Vest December 19, 2025
The claim that pregabalin reduces pain by half in 37% of users is misleading. The NNT (number needed to treat) for 50% pain reduction is actually 6.7, meaning most patients experience minimal benefit. Also, Qutenza’s 31% reduction is statistically significant but clinically marginal. Always contextualize efficacy with effect size, not just percentages.
Chris Davidson December 20, 2025
Scrambler therapy is a scam. You pay $1500 for placebo effect. The FDA approved it because the trials were funded by the company that makes the device. Wake up people. Big Pharma is laughing all the way to the bank
Kinnaird Lynsey December 22, 2025
I appreciate the effort put into this. Honestly though, I think the real issue is how long it takes to get diagnosed. I waited two years. By then, the damage was done. Maybe we need a public health campaign instead of just blog posts.
Andrew Kelly December 22, 2025
They say avoid opioids. But what about the people who've tried everything? The ones who can't sleep, can't work, can't even hug their kids without screaming? You want us to suffer because you're scared of addiction? That's not medicine. That's moralizing.
Isabel Rábago December 23, 2025
I’ve had idiopathic neuropathy since I was 28. Now I’m 54. No one knows why. I’ve tried everything. The only thing that gave me even a little peace was a 10mg nightly dose of CBD oil. No one talks about that. Maybe because it’s not patentable?
Anna Sedervay December 24, 2025
One must acknowledge that the current paradigm of pharmaceutical intervention is fundamentally flawed. The very notion of targeting symptoms rather than systemic bioenergetic dysregulation-particularly mitochondrial dysfunction induced by environmental xenobiotics-is a paradigmatic failure of contemporary neurology. One must consult the work of Dr. David Perlmutter on neurotoxicity cascades.
Moses Odumbe December 24, 2025
B12 shots changed my life. 🚀 Also, walk barefoot on grass every morning. Grounding = nerve healing. I swear by it. And yes, I know I sound like a cult leader but look at my feet now 👟🔥
Kelly Mulder December 25, 2025
I find it deeply offensive that you treat neuropathy like a checklist. This isn't a DIY project. It's a neurological catastrophe. And you're just throwing out 'walk more' like it's a yoga tip. Some of us are in wheelchairs.
Tim Goodfellow December 27, 2025
This post is a godsend. I’ve been yelling into the void for years that foot checks are non-negotiable. My uncle lost a toe because he thought it was just a blister. Don’t be him. Check. Your. Feet. Twice. A. Day. And if you’re diabetic, stop pretending you’re invincible. You’re not. You’re just numb.