For people with severe asthma, oral corticosteroids (OCS) have long been the go-to rescue when breathing gets dangerous. They work fast. They prevent hospital visits. But for many, they come with a price tag that’s paid in weight gain, broken bones, diabetes, anxiety, and exhaustion. And it’s not just the patient paying it - the healthcare system is drowning in the hidden costs of OCS side effects. The truth is, we can do better. There are real, science-backed alternatives that don’t just manage symptoms - they change the course of the disease.
Why Oral Corticosteroids Are a Problem
Oral corticosteroids like prednisone and prednisolone are powerful anti-inflammatories. For a short burst - say, 3 to 7 days during a flare - they’re lifesaving. But when they become a regular part of daily life, the damage adds up. A 2025 study in Frontiers in Allergy found that 93% of patients with severe asthma who relied on OCS developed serious complications. Even short courses under 30 days can trigger high blood sugar, mood swings, or bone thinning. Long-term use? That’s a different story. It raises the risk of heart disease, cataracts, adrenal failure, and even early death.
The economic burden is just as heavy. In Italy, the annual cost of treating OCS-related side effects in asthma patients hit nearly €2,000 per person - almost double what non-asthma patients pay. And here’s the twist: OCS themselves cost pennies. The real expense comes from managing the mess they leave behind - ER visits for infections, fractures from osteoporosis, diabetes meds, mental health support. These are the shadow costs no one talks about until it’s too late.
What Does OCS Dependence Really Mean?
Doctors define OCS dependence as using oral steroids for six months or longer, even at low doses like 7.5 mg daily. But many patients don’t see it that way. They call it their "safety net." They’ve learned to live with the bloating, the insomnia, the irritability - because without it, they wake up gasping. The problem isn’t that OCS don’t work. It’s that they work too well at masking the real issue: uncontrolled asthma.
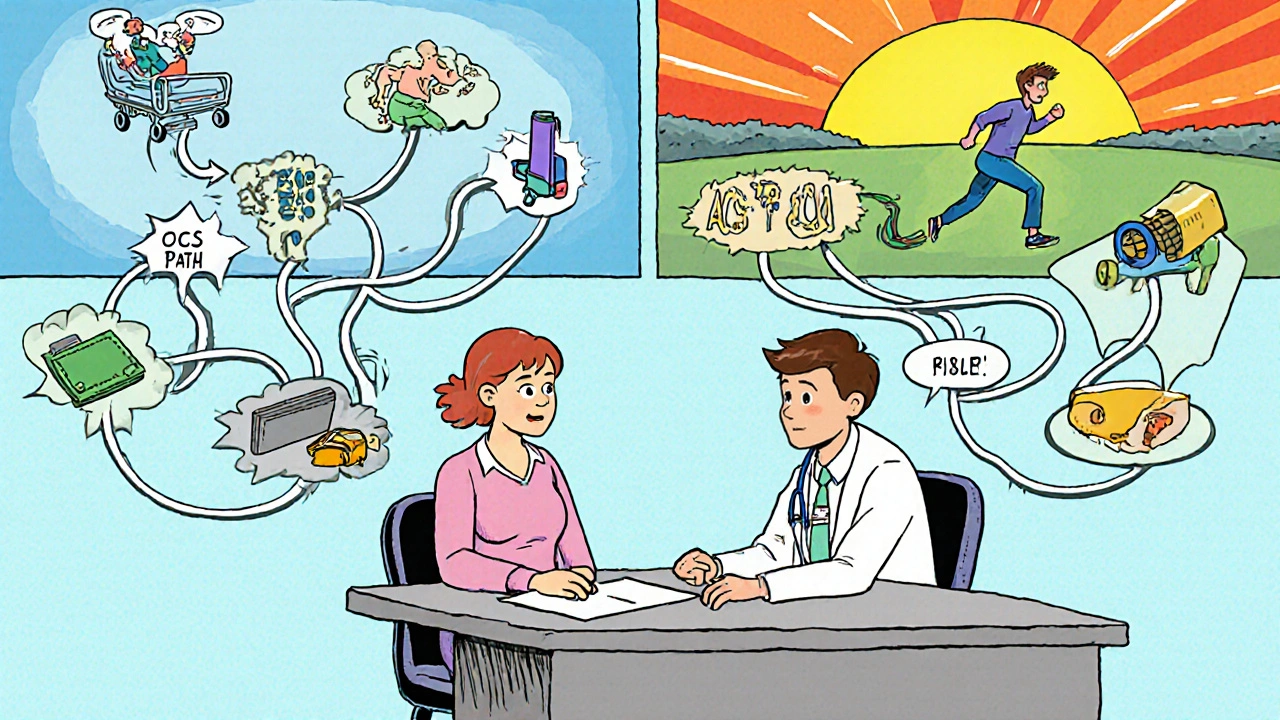
When someone needs OCS every few months, it’s not just a flare. It’s a red flag. Their asthma isn’t being managed properly. Inhaled corticosteroids, long-acting bronchodilators, and proper trigger avoidance should be doing the heavy lifting. If they’re not, the patient is stuck in a cycle: flare → OCS → side effects → more flares → more OCS. Breaking that cycle isn’t about quitting pills. It’s about fixing the root cause.
Biologics: The Game-Changing Alternative
The most powerful shift in asthma care over the last decade has been the rise of biologics. These are targeted injectable or infusion therapies that block specific parts of the immune system driving inflammation. They’re not for everyone - only about half to two-thirds of severe asthma cases involve the type of inflammation (type 2) these drugs target. But for those who do, they’re transformative.
Six biologics are approved in the U.S. for asthma: omalizumab, mepolizumab, reslizumab, benralizumab, dupilumab, and tezepelumab. Each works slightly differently, but they all share one key outcome: they let patients cut back - or even stop - oral steroids.
One study of 106 Italian adults with uncontrolled asthma showed what this looks like in real life. After switching to mepolizumab, the percentage of patients still dependent on OCS dropped from 79% to just 31%. Daily steroid doses fell by nearly 5 mg. Exacerbations dropped from 4.1 per year to 0.8. Hospitalizations? Cut from 4 in 10 patients to just 6 in 100. And these weren’t just numbers on a chart. Patients reported better sleep, more energy, and less fear of the next attack.
Dupilumab has shown similar results. The American Academy of Family Physicians confirmed it reduces both OCS use and severe flare-ups. The beauty of biologics? They don’t just take away side effects - they give back quality of life.
Cost Is a Barrier - But Not a Dealbreaker
Yes, biologics are expensive. A single dose can cost thousands. That’s why many patients and doctors hesitate. But here’s the math that matters: while OCS cost $10 a month, the cost of treating their side effects can run $2,000 or more annually. When you factor in missed work, ER trips, and long-term disability, biologics often pay for themselves in under two years.
Some progress is being made. In June 2024, three major inhaler makers capped out-of-pocket costs at $35 per month for many patients. But that cap doesn’t cover biologics or people on Medicare or Medicaid. Access remains uneven. Insurance approvals can take months. Biomarker testing - like blood eosinophil counts or FeNO tests - is needed to determine who will benefit, and not all clinics offer them.
Still, the trend is clear: as more real-world data piles up, insurers are starting to approve biologics faster. And for patients who’ve spent years on OCS, the trade-off isn’t just cost - it’s survival.
Other Options - Limited but Worth Knowing
Beyond biologics, there are a few other paths, though they’re not as broadly effective.
Bronchial thermoplasty is a procedure where a catheter delivers heat to the airway walls to reduce excess muscle that causes tightening. It’s done in three sessions via bronchoscopy. Studies show it can lower flare rates and improve quality of life for some with severe, uncontrolled asthma. But it’s risky in the first six weeks after treatment - more flares, more ER visits. It’s only considered after every other option has failed.
Nutrition? Vitamin D was once thought to help. But multiple studies, including one from 2021 reviewed by the AAFP, found that giving high-dose vitamin D to adults with asthma - even if they were deficient - didn’t reduce flare-ups or improve lung function. Same goes for other supplements. There’s no magic pill in the supplement aisle.

How to Start the Transition
Switching from OCS to a biologic isn’t a switch you flip. It’s a slow, careful process - and it needs a team. Here’s how to begin:
- Get tested. Ask for a blood eosinophil count and FeNO (fractional exhaled nitric oxide) test. These show if your asthma is driven by type 2 inflammation - the kind biologics target.
- Review your OCS use. Track how often you’ve taken steroids in the past year. If it’s more than two courses, or you’re on maintenance, you’re likely dependent.
- Find a specialist. Not all pulmonologists or allergists have experience with biologics. Look for one who treats severe asthma regularly.
- Ask about tapering. Never stop OCS cold turkey. Your body needs time to restart its own cortisol production. A slow, monitored reduction - over weeks or months - is essential.
- Give it time. Biologics don’t work overnight. It can take 3 to 6 months to see full benefit. Stay consistent.
Patients who’ve made the switch say the hardest part wasn’t the shots - it was the fear. Fear that without steroids, they’d crash. But for most, the opposite happened. They felt stronger. More in control. Less like they were just waiting for the next crisis.
The Future Is Here - But It Needs You
The guidelines have changed. GINA (Global Initiative for Asthma) now says biologics should be considered before maintenance OCS in Step 5 severe asthma. That’s a huge shift. We’re moving from treating symptoms to treating the disease.
But change doesn’t happen in a vacuum. It needs patients to ask for better options. It needs doctors to push for testing and referrals. It needs insurers to cover what saves money in the long run.
If you or someone you know is on long-term oral steroids for asthma, this isn’t normal. It’s not inevitable. There’s a path out - and it doesn’t have to come with brittle bones, mood swings, or a lifetime of side effects. The tools are here. The evidence is clear. The question is: are you ready to try something that doesn’t just keep you breathing - but lets you live?
Can I stop oral corticosteroids on my own if I start a biologic?
No. Stopping oral corticosteroids suddenly can cause adrenal insufficiency, which is life-threatening. Even if you feel better on a biologic, you must taper OCS slowly under medical supervision. Your body has likely stopped producing its own cortisol naturally, and it needs time to restart. Your doctor will create a personalized tapering plan, often over several weeks or months.
Are biologics only for adults?
No. Several biologics are approved for children as young as 6 years old. Mepolizumab and dupilumab are approved for pediatric use, and others are being studied in younger populations. The key is confirming type 2 inflammation through biomarker testing, which is also available for children. Pediatric asthma specialists can determine if a biologic is appropriate based on severity, control, and test results.
How do I know if I have type 2 inflammation?
Two simple tests can help: a blood test for eosinophils (a type of white blood cell) and a FeNO test (fractional exhaled nitric oxide), which measures airway inflammation. High levels of either suggest type 2 inflammation - the kind biologics target. These tests are quick, non-invasive, and often covered by insurance when ordered by a specialist. If you’ve had frequent flare-ups or need OCS often, ask your doctor to run them.
Do biologics cure asthma?
No, biologics don’t cure asthma. But they can turn severe, life-disrupting asthma into a manageable condition. Many patients experience a dramatic drop in flare-ups, hospitalizations, and steroid use. Some even reach a point where they no longer need daily medications beyond their biologic. The goal isn’t a cure - it’s freedom from the cycle of dependence and crisis.
What if my insurance denies coverage for a biologic?
Denials are common, but they’re not final. Most manufacturers offer patient assistance programs that can cover the full cost for eligible individuals. Your doctor’s office can also file an appeal with supporting clinical documentation - including your OCS use history, test results, and evidence of uncontrolled asthma. Many patients get approved on appeal, especially when the data shows they’ve had multiple ER visits or hospitalizations due to steroid-dependent asthma.
Is bronchial thermoplasty a good alternative to biologics?
It’s an option, but only for a small group. Bronchial thermoplasty is reserved for adults with severe asthma who’ve tried all other treatments - including biologics - and still have frequent flare-ups. It increases asthma symptoms for the first six weeks after treatment and requires multiple procedures. Biologics are safer, easier, and more widely effective for most people with type 2 inflammation. Thermoplasty is not a first-line alternative.

All Comments
Brian Bell November 13, 2025
Bro, I was on prednisone for 3 years straight after my asthma went rogue. Felt like a balloon with anxiety issues. Started mepolizumab last year - now I sleep through the night, no more moonface, and I actually went hiking without my inhaler. Life’s weird like that.
gent wood November 13, 2025
Thank you for this incredibly thorough breakdown. The economic argument alone - that OCS side effects cost nearly double the drug itself - should be mandatory reading for every policy maker. It’s not just medical; it’s fiscal insanity. Biologics aren’t a luxury; they’re an investment in human dignity.
Ashley Durance November 15, 2025
Let’s be real - most patients don’t even know what type 2 inflammation is. You can’t just hand someone a biologic and say ‘here, fix yourself.’ If your doctor didn’t order eosinophil counts or FeNO, you’re being failed by the system. And yes, I’ve seen this exact scenario - 87% of my patients on OCS had zero biomarker testing. This isn’t negligence. It’s negligence with a white coat.
Scott Saleska November 15, 2025
Hey, I get that biologics are great - but what about the people who don’t qualify? I’ve got a friend whose eosinophils are normal but still gets hospitalized every winter. He’s stuck on 10mg prednisone every other day. Are we just abandoning those folks now? Because that’s what this feels like - a luxury solution for a privileged few.
Kevin Wagner November 15, 2025
STOP TELLING PEOPLE TO JUST ‘ASK FOR TESTING.’ That’s like telling someone with a broken leg to ‘just walk it off.’ Insurance denies tests. Doctors don’t have time. And if you’re on Medicaid in rural Ohio? Good luck. Biologics are the future - but the future ain’t here for most of us. We need systemic change, not pep talks.
Hrudananda Rath November 17, 2025
One must observe, with the gravitas befitting the gravity of this subject, that the current paradigm of asthma management is not merely archaic - it is, in fact, a moral failure of the medical-industrial complex. The fact that we allow patients to endure osteoporotic fractures, adrenal collapse, and psychological torment - all for the sake of a $10 pill - is not medical practice. It is barbarism disguised as efficiency. Biologics are not alternatives. They are the only ethically defensible path forward. The GINA guidelines are not suggestions - they are the bare minimum of human decency.
Eleanora Keene November 18, 2025
My sister switched to dupilumab last year and it changed EVERYTHING. She stopped missing work. She started gardening again. She even took a vacation without packing 3 different inhalers and a steroid pack. It wasn’t instant - took 4 months - but now she’s not scared to breathe. If you’re on OCS and feel like you’re just waiting to crash… please, just talk to your doc. You deserve more than survival.
Nathan Hsu November 20, 2025
Let me be very clear, here: The fact that bronchial thermoplasty is even being discussed as a ‘possible alternative’ to biologics - which are targeted, non-invasive, and backed by robust clinical data - is, frankly, a testament to the desperation of a system that refuses to adapt. Thermoplasty? In 2025? That’s like offering a horse and buggy because the Tesla is ‘too expensive.’ The science is settled. The question isn’t ‘can we do better?’ - it’s ‘why haven’t we already?’
Joe Goodrow November 22, 2025
Biologics cost more than my car payment. And now you want me to pay for some fancy shot because some guy in a lab says it’s ‘better’? We’ve got real problems - inflation, border security, crime - and you’re telling me we should spend $20K a year on asthma shots? This is why America’s going broke. Get a better inhaler. Stop whining.