Every year, more than 100,000 people in the U.S. die from opioid overdoses. Most of these deaths are preventable. The key? Knowing how to use naloxone before it’s too late.
What Naloxone Does and How Fast It Works
Naloxone is not a cure for addiction. It’s a rescue tool. When someone overdoses on heroin, fentanyl, oxycodone, or any other opioid, their breathing slows or stops. Naloxone flips the switch back on. It binds to the same brain receptors as the opioid-but instead of causing sedation, it kicks the opioid out and blocks it from coming back in.
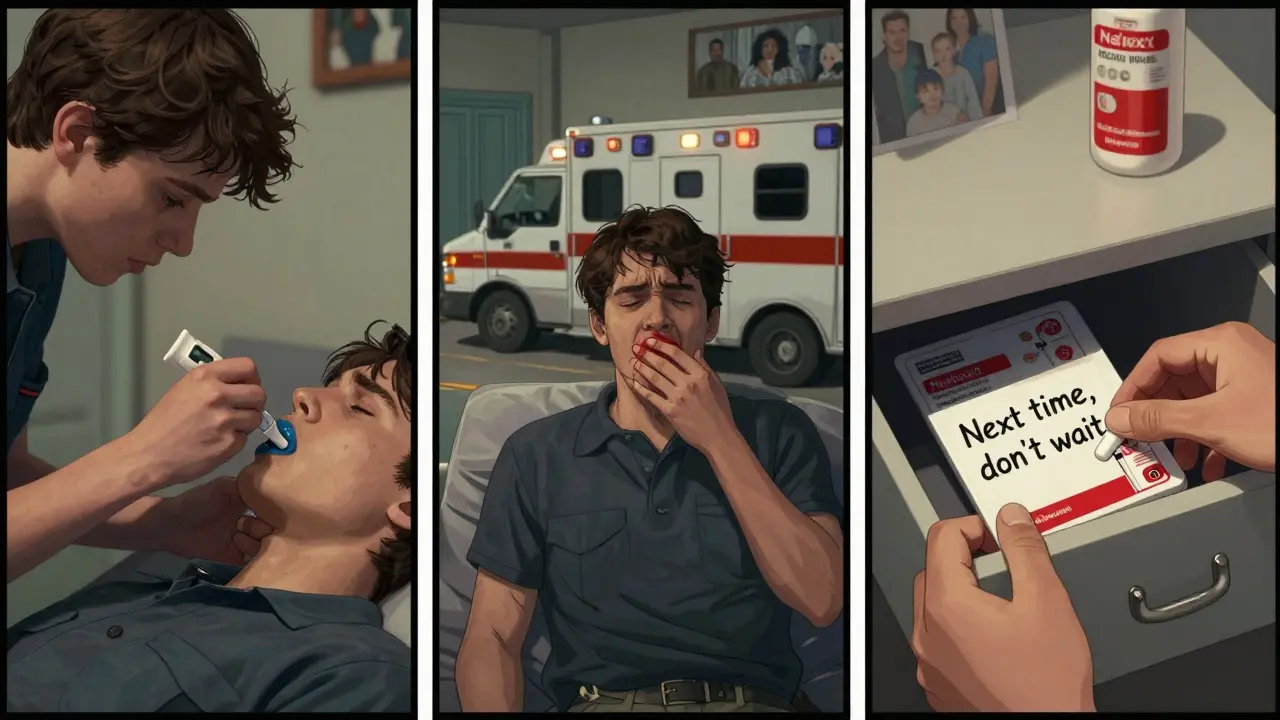
This isn’t magic. It’s science. Within 3 to 5 minutes of being injected or sprayed into the nose, naloxone starts reversing the overdose. Breathing returns. Consciousness comes back. Studies show it works in 95% of cases-if given fast enough.
But here’s the catch: naloxone doesn’t last long. Its effects wear off in 30 to 90 minutes. Many opioids, especially fentanyl, stay in the body much longer. That means someone can start to slip back into overdose after naloxone wears off. That’s why calling 911 is non-negotiable-even if the person seems fine after the first dose.
Why Fentanyl Makes Overdoses So Dangerous
Fentanyl is 50 to 100 times stronger than morphine. A tiny amount-less than two grains of salt-can kill. And it’s everywhere. In 2022, fentanyl was involved in 80% of all opioid overdose deaths in the U.S.
Because it’s so potent, one dose of naloxone often isn’t enough. The CDC found that 40% of fentanyl overdoses require two or more doses of naloxone to reverse. That’s why having more than one kit on hand matters. If you’re helping someone, give the first dose right away. If they don’t respond within 3 minutes, give a second. And if they still don’t wake up, give a third.
Don’t wait. Don’t hesitate. Every second counts. A 2022 study in Addiction showed survival rates dropped from 95% to 65% when naloxone was given after five minutes instead of two.
Nasal Spray vs. Injection: Which Is Better?
There are two main ways to give naloxone: nasal spray and injection. The nasal spray (like Narcan) is easier for most people to use. You don’t need training. You don’t need needles. Just tilt the head back, insert the nozzle, and press the plunger.
Studies show nasal spray has an 85% success rate when used by laypeople. Injection works just as well-but only if you can do it correctly under stress. In real-life emergencies, people panic. They fumble with syringes. They miss the muscle. That’s why nasal spray is now the go-to recommendation for families, friends, and community members.
The FDA approved the first over-the-counter nasal spray in March 2023. Since then, it’s been available in pharmacies without a prescription in all 50 states. You can buy it next to pain relievers and allergy meds. No ID. No paperwork. Just grab it.
What Naloxone Can’t Do
Naloxone only works on opioids. That’s it. If someone overdoses on alcohol, benzodiazepines, cocaine, or methamphetamine, naloxone won’t help. Giving it to someone who didn’t take opioids won’t hurt them-it has zero effect. But it also won’t save them.
That’s why recognizing the signs of an opioid overdose is critical:
- Unresponsive to loud noises or shaking
- Slow, shallow, or stopped breathing
- Blue or gray lips and fingernails
- Pinpoint pupils
- Gurgling or snoring sounds (like they’re choking)
If you see these signs, assume it’s an opioid overdose. Give naloxone. Call 911. Start rescue breathing if needed. Don’t wait for confirmation. Don’t wait for a test. Act.

Side Effects: Withdrawal Isn’t the Enemy
When naloxone kicks an opioid out of the brain, it can cause sudden withdrawal. That’s not a side effect-it’s proof it’s working. Symptoms include:
- Nausea and vomiting (25% of cases)
- Agitation or anxiety (45%)
- Sweating, shaking, or muscle aches
- Increased heart rate
It’s scary to watch someone wake up screaming and thrashing. But this is better than death. Experts like Dr. Lewis Nelson from NYU warn that too much naloxone can make withdrawal worse-but that’s rare. The real danger is not giving enough.
One Reddit user wrote: “I gave my brother two doses. He woke up furious, punching the wall. I thought I messed up. Then he hugged me and said, ‘You saved my life.’”
Safe Storage: Keep It Accessible, Not Hidden
Naloxone doesn’t need refrigeration. It’s stable at room temperature. But people often store it where no one will think to look-like the back of a medicine cabinet, tucked under a pile of old prescriptions.
Here’s what works better:
- Keep it with your car keys or wallet
- Store it in your purse, backpack, or bedside drawer
- Give one to a friend who uses opioids
- Keep one in your glovebox or work bag
Expiry dates matter. Most kits last 18 to 24 months. Check the label. Replace expired ones. Some community programs offer free replacements. Call your local health department.
And don’t let cost stop you. While retail price can be $130-$150, many pharmacies offer discounts. Free kits are available through state programs, needle exchanges, and nonprofits. If you can’t afford it, ask. You’re not alone.
What to Do After Giving Naloxone
Once you give naloxone, you’re not done. Here’s your checklist:
- Call 911 immediately. Even if they wake up.
- Place them in the recovery position: on their side, one leg bent, head tilted back. This prevents choking if they vomit.
- Stay with them. Monitor breathing. Be ready to give more naloxone if they relapse into overdose.
- Don’t let them leave. They may feel fine, but the opioid is still in their system.
- Hand over the used kit to EMS. They’ll need to know what you gave and how much.
One common mistake? People give naloxone, wait for the person to wake up, then let them go home. That’s how people die twice. The opioid comes back. The naloxone wears off. No one’s there to help.
Who Should Have Naloxone?
You don’t need to be a doctor. You don’t need to be a first responder. If you know someone who uses opioids-even if they’re in recovery-you should have naloxone.
So should:
- Family members of people with opioid use disorder
- People who take prescription opioids long-term
- Friends of people who use drugs
- Teachers, coaches, librarians, and anyone who works with at-risk youth
- Anyone who lives in a community with high overdose rates
The CDC says for every 10% increase in naloxone distribution, overdose deaths drop by 2.3%. That’s real. That’s measurable. That’s hope.
What’s Next for Naloxone?
Researchers are working on longer-lasting versions. One new drug, nalmefene, lasts up to 11 hours-twice as long as naloxone. It’s not approved for overdose yet, but trials are promising.
The FDA just approved an 8 mg nasal spray in April 2024-double the strength of the standard version-for use against powerful fentanyl analogs. The Biden administration is funding $200 million to get 2 million free kits into communities by 2026.
But technology alone won’t fix this. People will. Friends will. Strangers will. The person who buys naloxone because they’re scared. The one who learns how to use it in a 15-minute training. The one who keeps it in their pocket.
That’s what saves lives.
Can naloxone hurt someone who didn’t take opioids?
No. Naloxone has no effect on people who don’t have opioids in their system. It won’t cause drowsiness, addiction, or withdrawal. It’s safe to use even if you’re unsure whether an overdose is opioid-related.
How many doses of naloxone should I keep on hand?
At least two. Fentanyl and other potent opioids often require multiple doses. One kit typically contains one or two doses. If you’re helping someone at risk, keep two kits available. Many state programs give out kits in pairs for this reason.
Is naloxone legal to carry without a prescription?
Yes. All 50 states allow naloxone to be purchased over the counter at pharmacies without a prescription. Some states even allow pharmacies to give it away for free. You can legally carry it anywhere, even in public spaces or vehicles.
Can I use naloxone on a child or teenager?
Yes. Naloxone is safe for all ages, including infants and teens. The dose doesn’t change based on weight. Use the same dose for adults and children. If a child overdoses on opioids, giving naloxone immediately could save their life.
Where can I get free naloxone?
Many local health departments, harm reduction centers, and pharmacies offer free naloxone kits. You can also call the National Harm Reduction Coalition or visit NIDA’s website for a list of free distribution sites near you. Some programs mail kits directly to your home.
What if I’m afraid to call 911 because of legal trouble?
All 50 states have Good Samaritan laws that protect people who call for help during an overdose. These laws shield you from arrest for drug possession if you’re seeking help. The priority is saving a life. Emergency responders are trained to focus on medical care, not law enforcement.
Final Thought: Be the Person Who Acts
Most opioid overdoses happen at home. With friends. With family. With people who care. That’s why naloxone isn’t just for hospitals or clinics. It’s for your kitchen counter. Your car. Your coat pocket.
You don’t need to be brave. You just need to be ready.

