Naloxone Readiness Plan Checklist
Naloxone Readiness Plan Checklist
Assess your readiness for opioid overdose response with this interactive checklist. Complete all items before an emergency happens.
When someone is prescribed opioids for pain, the risk of overdose doesn’t disappear just because they’re following their doctor’s instructions. Opioids slow breathing - sometimes so much that it stops. And when that happens, minutes matter. Naloxone isn’t a cure for addiction. It’s a safety net. A simple, fast-acting tool that can bring someone back from the edge. But having it isn’t enough. You need a naloxone readiness plan.
Why a Naloxone Readiness Plan Isn’t Optional
Naloxone reverses opioid overdoses by kicking the opioids off the brain’s receptors. It works in 2 to 5 minutes. It’s safe. It doesn’t work on non-opioid overdoses - so if you give it to someone who hasn’t taken opioids, it does nothing. No harm. No side effects. That’s the beauty of it. But here’s the problem: most people don’t know how to use it. Or they don’t have it nearby. Or they wait too long to call 911. In 2022, the CDC found that nearly 9 out of 10 opioid overdose deaths happened to people who weren’t even on a prescription at the time. That means the danger isn’t just for people with addiction. It’s for anyone taking opioids - even for a week after surgery. A readiness plan isn’t about fear. It’s about control. It’s knowing exactly what to do before the emergency happens.What’s in a Naloxone Kit? (And How Much Do You Need?)
There are two main types of naloxone kits used today: nasal spray and injection.- Nasal spray (NARCAN®): One 4mg dose. Easy to use - no needles. Just insert the nozzle into one nostril and press the plunger. FDA approved for over-the-counter sale in March 2023. Retail price: $130-$150 without insurance.
- Intramuscular injection: Two 0.4mg vials with a syringe. Cheaper - about $25-$40 per dose - but requires training. Used in clinics and by first responders.
How to Use Naloxone: A Step-by-Step Guide
Time is everything. Here’s what to do when someone isn’t responding:- Check for signs: Unresponsive to shaking or shouting. Slow, shallow, or stopped breathing. Blue lips or fingertips. Pinpoint pupils.
- Call 911 immediately. Even if you give naloxone, they still need medical care. Overdose can cause other complications like aspiration or muscle breakdown.
- Give naloxone: For nasal spray: Tilt head back, insert nozzle fully into one nostril, press plunger firmly. For injection: Inject into the outer thigh - through clothing if needed. Use a 22-25 gauge needle at a 90-degree angle.
- Start rescue breathing: Tilt head back, lift chin. Give one breath every 5 seconds. Don’t stop until they’re breathing on their own or help arrives. Brain damage can start in under 3 minutes without oxygen.
- Wait and watch: If they don’t respond in 2-3 minutes, give a second dose. Keep giving breaths. Stay with them. Monitor for at least 2-3 hours. They may need more doses.
Who Needs Naloxone? It’s Not Just for ‘Addicts’
The biggest myth? That naloxone is only for people with substance use disorder. In 2021, 38.2% of opioid overdose deaths involved prescription opioids alone - no street drugs. That’s someone taking oxycodone for back pain. Or hydrocodone after a knee replacement. Or morphine in hospice care. The CDC says you should consider naloxone for anyone prescribed more than 50 morphine milligram equivalents (MME) per day. That’s about 10 tablets of 5mg oxycodone. But many doctors don’t ask. A 2022 survey found only 32.4% of primary care providers routinely discuss naloxone with high-risk patients. The American Medical Association now says: Co-prescribe naloxone with any new opioid prescription longer than 3 days. That’s the new standard. Not a suggestion. Not an option. And it’s not just for patients. Family members, caregivers, coworkers - anyone who might be around someone taking opioids should know where the naloxone is and how to use it.Barriers Are Real - And Fixable
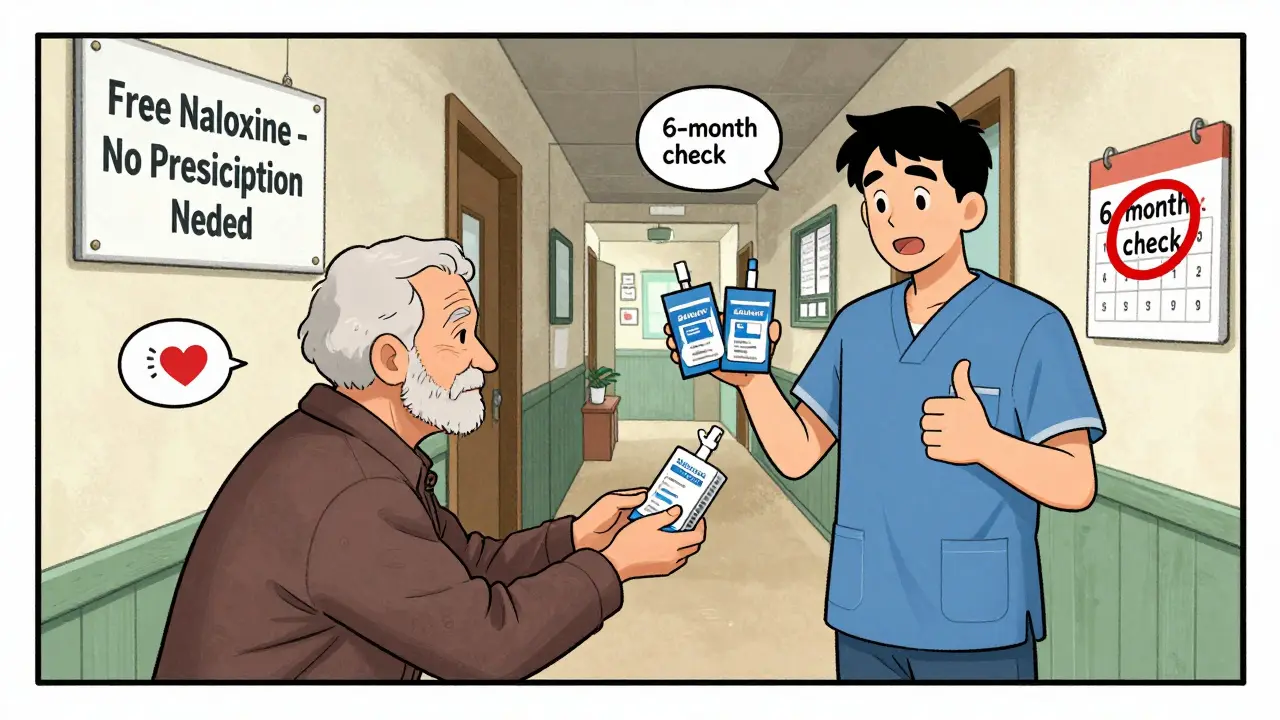
Cost is the biggest hurdle. Nearly 42% of uninsured people say they can’t afford naloxone. But help exists. Forty-seven states have laws allowing pharmacists to dispense naloxone without a prescription. Many pharmacies offer it for free or low cost through public health programs. In Pennsylvania, standing orders let pharmacies give out naloxone without individual prescriptions. In South Carolina, over 12,000 free kits were distributed in just one quarter. In Oklahoma, over 37,000 were given out in 2022. Workplaces are catching on too. OSHA now recommends naloxone in any workplace with more than 15 employees. Why? Workplace overdose deaths have jumped 619% since 2011. That’s not just a health issue - it’s a safety issue. Stigma still holds people back. Some fear that having naloxone means you’re enabling drug use. But naloxone doesn’t encourage use. It saves lives. And when someone survives, they have a second chance - to get treatment, to reconnect with family, to rebuild.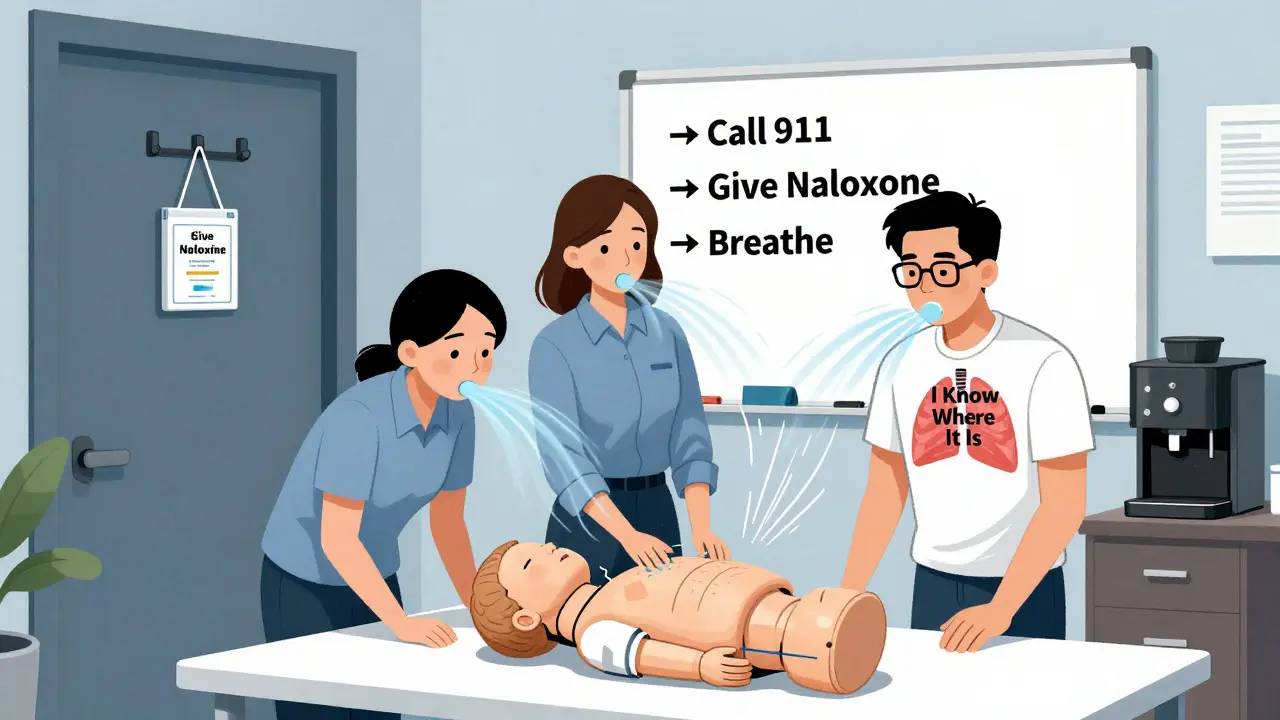
What Happens After Naloxone?
Naloxone saves breathing. It doesn’t fix the underlying problem. That’s why follow-up care matters. After reversal, patients can experience:- Withdrawal symptoms - nausea, vomiting, sweating, agitation. Pain can return sharply.
- Delayed complications - aspiration pneumonia, rhabdomyolysis (muscle breakdown), kidney injury. These caused nearly 17% of post-reversal deaths in Massachusetts in 2021-2022.
Building Your Plan: A Checklist
Here’s what your readiness plan needs:- At least two naloxone doses (nasal spray preferred)
- Stored in an easy-to-reach place - not locked up
- Check expiration dates every 6 months - replace every 18-24 months
- Everyone who might be present knows where it is and how to use it
- A written plan posted near the kit: “If unresponsive, call 911, give naloxone, start breathing”
- Annual training for caregivers, staff, or family members
- Know your local resources - where to get free kits, who to call for help
Final Thought: It’s Not About If - It’s About When
Opioids are powerful. They help. They heal. But they carry risk. A naloxone readiness plan doesn’t mean you expect an overdose. It means you’re prepared - just like you keep a fire extinguisher in the kitchen or a first aid kit in the car. In Washington State, over 28,000 overdoses were reversed with naloxone in 2022. That’s 28,000 people who went home. 28,000 families who didn’t bury someone too soon. You don’t need to be a doctor. You don’t need to be an expert. You just need to be ready.Can naloxone be given to someone who didn’t take opioids?
Yes. Naloxone only works on opioid receptors. If no opioids are present, it has no effect. It won’t cause harm, trigger withdrawal, or create side effects. Giving it to someone who didn’t overdose is safe and recommended if you’re unsure.
How many doses of naloxone should I keep on hand?
At least two doses. Many opioids - especially fentanyl - last longer than naloxone. A single dose may wear off before the opioid does, leading to a second overdose. For high-risk situations, rural areas, or workplaces, keep three or four doses. Always have extras.
Is naloxone covered by insurance?
Most insurance plans cover naloxone, especially when prescribed. Many pharmacies offer it for free or at low cost under state harm reduction programs. Even without insurance, over-the-counter NARCAN® is widely available at pharmacies like CVS, Walgreens, and Rite Aid.
Can I use naloxone on a child or elderly person?
Yes. Naloxone is safe for all ages. The dose doesn’t change based on weight or age. One nasal spray (4mg) is the standard for adults and children. If the person is unresponsive and you suspect opioid overdose, give naloxone - even if they’re a child or senior.
What if I don’t know how to use it?
Naloxone nasal spray is designed to be simple. Insert the nozzle into one nostril and press the plunger. No training is required. But practice helps. Many pharmacies offer free 5-minute demos. Online videos from the CDC or local health departments also show the steps. Don’t wait for an emergency to learn.
Where can I get free naloxone?
Many states and local health departments offer free naloxone kits. Pharmacies with standing orders can dispense without a prescription. Organizations like Harm Reduction Coalition, local syringe exchange programs, and community clinics often give them out at no cost. Search online for “free naloxone near me” or call your county health department.
Does naloxone work on fentanyl overdoses?
Yes, but it often takes more than one dose. Fentanyl is 50-100 times stronger than morphine. One 4mg nasal spray may not be enough. Be prepared to give a second or even third dose. Always call 911 - even if they wake up after the first dose.
How long does naloxone last?
Naloxone lasts 30 to 90 minutes. Many opioids last longer - especially fentanyl, carfentanil, or extended-release pills. That’s why monitoring for 2-3 hours after reversal is critical. The person can slip back into overdose once naloxone wears off.
Can I carry naloxone in my purse or car?
Absolutely. Naloxone is stable at room temperature. Keep it in your bag, glove compartment, or first aid kit. Don’t leave it in extreme heat (like a hot car in summer) for long periods. Check expiration dates regularly - replace every 18-24 months.
What if I’m afraid to call 911?
Many states have Good Samaritan laws that protect people who call for help during an overdose. You won’t get in trouble for calling. The priority is saving a life. Emergency responders are trained to help, not punish. If you’re unsure, call anyway - they’ve heard it all before.


All Comments
Lindsey Kidd December 24, 2025
I keep two NARCAN kits in my car and one by the front door. My brother’s on oxycodone for chronic pain, and I won’t risk not being ready. 🙏💉
Also, I taught my whole family how to use it last weekend. No shame in being prepared.
Austin LeBlanc December 24, 2025
People really think this is just for junkies? I’ve seen moms with post-surgery prescriptions OD on their couch. This isn’t about morality. It’s about dumb luck and bad timing. If you’re not keeping naloxone at home, you’re gambling with someone’s life.
niharika hardikar December 25, 2025
The empirical evidence supporting the co-prescription paradigm is unequivocal. The pharmacokinetic disparity between opioid half-lives and naloxone’s duration necessitates a multi-dose protocol, particularly in the context of fentanyl analogues. Institutional adoption of standing orders and public health distribution models represents a paradigm shift in harm reduction policy.
Rachel Cericola December 26, 2025
Let me tell you something real: I work in a rural clinic where the ambulance takes 45 minutes. We hand out three doses of naloxone with every opioid script. Why? Because last year, a 72-year-old woman came in after her husband overdosed. She had the kit. She gave two doses. She did rescue breathing for 17 minutes until EMS arrived. He’s alive today because she didn’t panic. She knew what to do. You don’t need to be a doctor. You just need to be the person who didn’t look away. And if you’re thinking, ‘But what if they’re an addict?’ - guess what? They’re someone’s parent. Someone’s sibling. Someone who just needed pain relief and got trapped. This isn’t about judgment. It’s about showing up. Keep the kit out. Train your kids. Tell your coworkers. Make it normal. Because when seconds count, the only thing worse than having it and not using it… is not having it at all.
Blow Job December 26, 2025
I’ve given naloxone twice. Both times, the person woke up confused, angry, and then cried. One guy hugged me so hard I thought my ribs would crack. He didn’t say thank you. He didn’t have to. I just sat with him until the paramedics came. That’s what this is - not a tool, not a policy. It’s a human moment you didn’t know you’d be handed.
Christine Détraz December 28, 2025
I used to think this was overkill. Then my cousin’s kid got prescribed hydrocodone after a sports injury. I asked her mom if she had naloxone. She said no, ‘it’s not like he’s doing drugs.’ I bought her a kit. Gave her the demo. She cried. Said she didn’t know she needed it. Now she keeps it next to the coffee maker. I’m not proud. I’m just glad I spoke up.
John Pearce CP December 29, 2025
This country has lost its moral compass. We hand out life-saving antidotes like candy and call it compassion. But compassion without accountability is enabling. Why are we not addressing the root causes? Why are we not enforcing stricter prescribing laws? Why are we not holding doctors accountable for overprescribing? Naloxone is a bandage on a bullet wound.
EMMANUEL EMEKAOGBOR December 30, 2025
In Nigeria, we do not have access to naloxone. But we understand the value of preparedness. When someone collapses, we act. We do not wait for permission. We do not wait for a prescription. We act. Perhaps the real lesson here is not about the drug, but about the courage to act when others hesitate.
CHETAN MANDLECHA December 31, 2025
I work in a pharmacy in Delhi. We started giving out naloxone kits last year. No script needed. People come in, ask for it, we hand it over. Some cry. Some just nod. One guy said, 'I didn't know I could get this without a doctor.' I told him, 'You didn't need one.' Simple as that.
Jillian Angus January 1, 2026
I keep one in my purse and one in my bike bag. I don’t even think about it anymore. If you’re around opioids, you’re around risk. That’s just how it is. I don’t need a lecture. I just need to be ready.
Ajay Sangani January 3, 2026
sometimes i think about how we’ve turned survival into a checklist. we have protocols and kits and training videos… but what if the real question isn’t how to use naloxone… but why we let people get this close to the edge in the first place? maybe the plan isn’t just about the kit… maybe it’s about the world that needs it.