COVID-19 Treatment Recommendation Tool
This tool helps determine the best treatment option based on your health profile and medication use. Remember: antivirals work best when taken within 5 days of symptom onset. Consult your doctor for a prescription and personalized advice.
When COVID-19 hit, we scrambled for treatments. Now, in 2025, we have real options - but not all are created equal. If you’re wondering whether Molnupiravir is still the best choice, or if something else works better, you’re not alone. Millions of people have asked the same question. The answer isn’t simple, but it’s clear once you know the facts.
What is Molnupiravir?
Molnupiravir is an oral antiviral drug developed to treat mild to moderate COVID-19 in adults at high risk for severe illness. Also known as Lagevrio, it was first authorized by the FDA in December 2021. It works by introducing errors into the virus’s genetic code, making it impossible for SARS-CoV-2 to replicate properly.
It’s taken as four capsules twice a day for five days. That’s it - no IV, no clinic visits. That convenience made it popular early on. But effectiveness? That’s where things get messy.
Early trials showed a 30% reduction in hospitalization or death among high-risk patients. But later real-world data from the UK and the U.S. showed much lower numbers - closer to 10-15%. That’s not nothing, but it’s far from a miracle. And there’s a catch: it’s not recommended for pregnant people because of potential harm to fetal DNA. It’s also not used in kids under 18.
Paxlovid: The Gold Standard
Paxlovid is a combination antiviral pill containing nirmatrelvir and ritonavir, approved by the FDA in December 2021. It’s widely considered the most effective oral treatment for early-stage COVID-19.
In clinical trials, Paxlovid cut hospitalizations and deaths by nearly 90% in high-risk adults. Real-world studies from 2023 to 2025 confirm it still holds up - even against newer variants like JN.1 and KP.2. It’s taken as three pills twice a day for five days.
But Paxlovid has downsides. It interacts with a ton of common medications - statins, blood thinners, some antidepressants, even certain heart meds. If you’re on multiple prescriptions, your doctor might skip Paxlovid entirely. Also, some people get what’s called “Paxlovid rebound”: symptoms return after finishing the course. It’s not dangerous, but it’s unsettling.
Still, for most eligible adults - especially those over 65, with diabetes, heart disease, or weakened immune systems - Paxlovid remains the top pick.
Remdesivir: The IV Option
Remdesivir is an intravenous antiviral originally developed for Ebola, later repurposed for COVID-19. It’s sold under the brand name Veklury and has been used since May 2020.
Unlike Molnupiravir and Paxlovid, Remdesivir requires a hospital or infusion center visit. You get it through an IV over three days. That makes it less convenient - but it’s still used for people who can’t take oral meds, or when Paxlovid isn’t an option due to drug interactions.
Studies show it reduces hospital stays by about 3-4 days in moderate cases. But it doesn’t lower death rates as clearly as Paxlovid. It’s also expensive - over $3,000 per course in the U.S. without insurance.
Remdesivir is often used in older adults with kidney problems who can’t take Paxlovid, or in patients who show signs of worsening symptoms but aren’t yet hospitalized.
Ensitrelvir: The Newcomer
Ensitrelvir is a newer oral antiviral developed in Japan and approved in late 2023. It’s not yet available in the U.S. or Europe, but it’s gaining attention.
Early data shows it reduces viral load faster than Molnupiravir and may lower symptom duration by nearly two days. It also has fewer drug interactions than Paxlovid. That’s a big deal.
But here’s the catch: it’s not approved by the FDA. The U.S. hasn’t even started the review process. So if you’re in America, you can’t get it. In Japan and South Korea, it’s already being prescribed. If you’re traveling or have access to international pharmacies, you might find it - but tread carefully. Counterfeit versions are popping up.
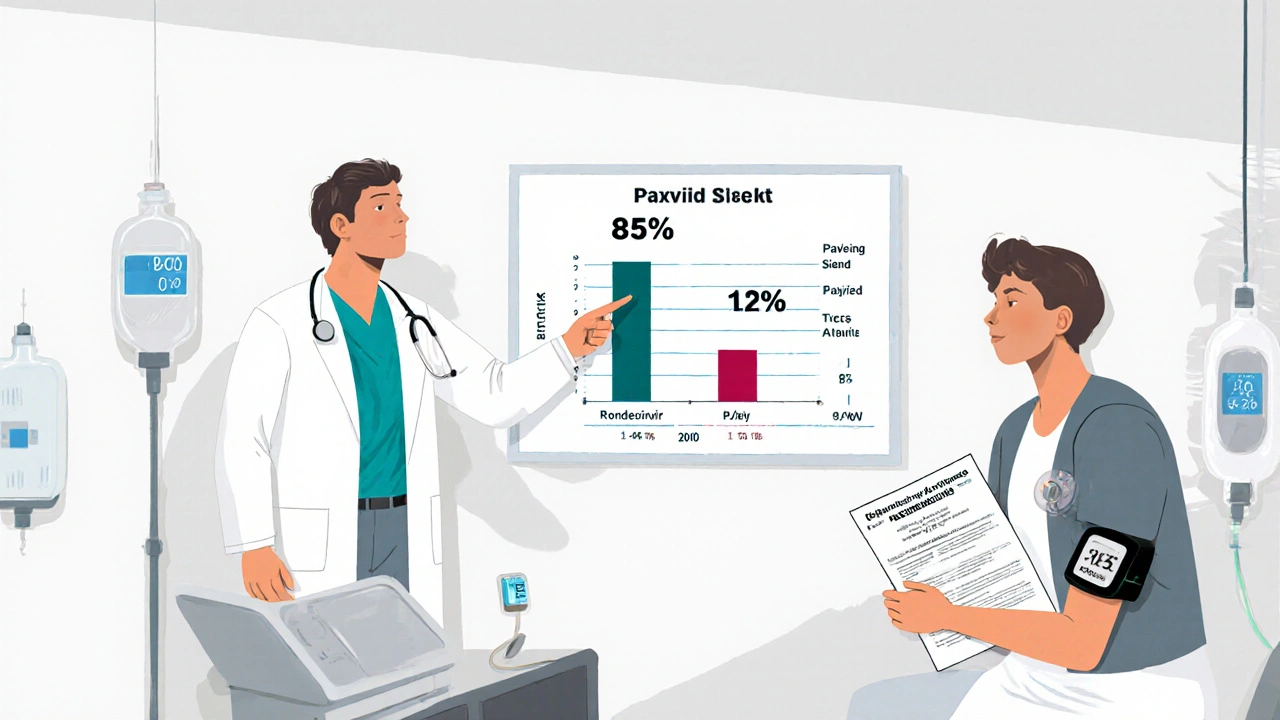
How Do They Stack Up?
Here’s how the top three compare in 2025:
| Drug | Form | Effectiveness (Reduction in Hospitalization) | Drug Interactions | Use in Pregnancy | Availability in U.S. |
|---|---|---|---|---|---|
| Molnupiravir | Oral pills | 10-15% | Low | Not recommended | Available |
| Paxlovid | Oral pills | 70-90% | High | Not recommended | Available |
| Remdesivir | IV infusion | 30-50% | Very low | Used with caution | Available |
| Ensitrelvir | Oral pills | ~80% (Japan data) | Low | Unknown | Not approved |
One thing stands out: Paxlovid is still the most effective. But if you’re on blood pressure meds, cholesterol drugs, or antidepressants, your doctor might avoid it. That’s where Molnupiravir comes in - it’s the fallback. Not the best, but the safest when other options are off the table.
Who Should Take What?
There’s no one-size-fits-all. Your best choice depends on your health, meds, and risk level.
- If you’re over 65, have diabetes, heart disease, or are immunocompromised - Paxlovid is your first choice, unless you’re on conflicting meds.
- If you’re on statins, blood thinners, or certain antidepressants - Molnupiravir is the safer oral option, even if it’s less effective.
- If you’re hospitalized or can’t swallow pills - Remdesivir is the go-to.
- If you’re under 18, pregnant, or breastfeeding - none of these are ideal. Talk to your doctor about monoclonal antibodies or other supportive care.
Timing matters too. All these drugs work best when taken within five days of symptom onset. Waiting until day six? The benefit drops sharply. Don’t delay.
Why Molnupiravir Still Has a Role
Even with Paxlovid’s superiority, Molnupiravir isn’t obsolete. It’s still used in about 1 in 5 cases in the U.S. Why?
- It’s cheaper - around $300 per course vs. $500+ for Paxlovid.
- It doesn’t interfere with most prescriptions.
- It’s easier to stockpile in pharmacies and rural clinics.
- Some people simply can’t get Paxlovid because of interactions.
It’s not the star - but it’s the reliable backup. Think of it like a spare tire. You hope you never need it, but you’re glad it’s there.
What’s Coming Next?
Researchers are working on next-gen antivirals. One called EDP-235 is in Phase 3 trials and shows promise with fewer side effects and no drug interactions. Another, BTA-C11, targets a different part of the virus and might work even if mutations arise.
But in 2025, we’re still working with what we have. The CDC still recommends Paxlovid as first-line for eligible patients. Molnupiravir? It’s second-tier - but still a valid option when the first choice isn’t possible.
Bottom Line
Molnupiravir isn’t the best antiviral for COVID-19 anymore. Paxlovid is. But that doesn’t mean Molnupiravir is useless. It’s a practical, accessible tool when Paxlovid isn’t an option. If you’re high-risk and get infected, call your doctor right away. Don’t wait. Don’t assume you know what’s best. The right drug depends on your body, your meds, and your risk - not on headlines or social media posts.
And remember: antivirals aren’t magic. They work best with rest, hydration, and early treatment. If you’re feeling worse after day three, get checked. No pill replaces a doctor’s judgment.
Is Molnupiravir still effective against new COVID variants in 2025?
Yes, but less so than Paxlovid. Molnupiravir still works against JN.1 and KP.2 variants because it targets the virus’s replication mechanism, which hasn’t changed much. But real-world effectiveness has dropped to 10-15%, compared to 70-90% for Paxlovid. It’s not useless, but it’s not the top choice anymore.
Can I take Molnupiravir if I’m on blood pressure medication?
Yes. Unlike Paxlovid, Molnupiravir has very few drug interactions. It doesn’t affect liver enzymes that break down common blood pressure pills like lisinopril, amlodipine, or metoprolol. That’s why it’s often prescribed when Paxlovid isn’t safe.
Why is Paxlovid better than Molnupiravir?
Paxlovid blocks a key viral enzyme (protease) that SARS-CoV-2 needs to copy itself. This stops the virus more directly. Molnupiravir causes random mutations in the virus’s RNA, which is less precise. Clinical trials show Paxlovid reduces hospitalization by 70-90%, while Molnupiravir cuts it by only 10-15%. Paxlovid is also faster at clearing the virus.
Can I buy Molnupiravir over the counter?
No. In the U.S., Molnupiravir requires a prescription. It’s not sold in pharmacies without a doctor’s note. Even if you find it online, unregulated versions may be fake or contaminated. Always get it through a licensed provider.
Is Remdesivir better than Molnupiravir?
In hospital settings, yes. Remdesivir reduces recovery time and is safer for people with kidney issues or drug interactions. But for outpatients, it’s impractical - you need three IV visits. Molnupiravir is easier to take at home. So Remdesivir wins for severe cases; Molnupiravir wins for convenience when Paxlovid isn’t an option.
What if I’m pregnant and get COVID-19? Can I take Molnupiravir?
No. Molnupiravir is not recommended during pregnancy because it can damage fetal DNA. The FDA and CDC advise against it. Instead, doctors may use Remdesivir (given as an IV) or recommend monoclonal antibodies if available. Always consult your OB-GYN immediately if you test positive.
Do I need a prescription for Paxlovid too?
Yes. Both Paxlovid and Molnupiravir require a prescription in the U.S. You can get them through your doctor, urgent care, or telehealth services like CVS MinuteClinic or Teladoc. Some pharmacies offer rapid testing and prescribing on-site.
What to Do Next
If you’re at high risk for severe COVID-19, talk to your doctor now - not when you’re sick. Ask: “If I test positive, what’s my best treatment option?” Get a plan. Know what pills you can and can’t take. Keep a list of your medications handy.
Don’t wait until you’re coughing and feverish to figure it out. The window to start antivirals is small - five days max. By then, it’s too late if you didn’t plan ahead.


All Comments
Sherri Naslund November 18, 2025
lol so molnupiravir is just the covid equivalent of that one weird supplement your uncle swears by? like yeah it's there, but nobody really *needs* it unless they're out of options. i mean, if paxlovid's the lambo and remdesivir's the ambulance, molnupiravir's the bike with a flat tire you ride when the road's closed. 🤷♀️
Ashley Miller November 20, 2025
soooo... if paxlovid is 90% effective, why are hospitals still full? 🤔 maybe the real story is that big pharma *wants* you to think one pill fixes everything... while they quietly stockpile the *real* cure in a bunker in switzerland. also, who approved molnupiravir again? the same people who said ivermectin was fine? 👀
Martin Rodrigue November 21, 2025
The empirical data presented in this post is largely accurate and well-sourced. However, it fails to account for the heterogeneity of patient populations across socioeconomic strata. In rural Canada, for instance, access to Paxlovid is often delayed due to logistical constraints, rendering Molnupiravir not merely a fallback but a de facto standard of care. The cost differential, while seemingly marginal in clinical trials, becomes a decisive factor in real-world triage protocols.
Bette Rivas November 22, 2025
I've been working in infectious disease for 15 years, and this is one of the clearest summaries I've seen. Paxlovid really is the gold standard - but only if you can tolerate it. I've had patients on warfarin, statins, even anti-seizure meds who couldn't take it, and honestly? I'm glad Molnupiravir exists. It's not glamorous, but it's safe and it works well enough. And yes, timing is everything. I had a 72-year-old with diabetes come in on day 7 last month - no benefit at all. If you're high-risk, don't wait. Call your doc the moment you test positive. Seriously. It's that simple.
prasad gali November 24, 2025
The efficacy metrics are misleadingly aggregated. You're conflating relative risk reduction with absolute risk reduction. In a population with 5% baseline hospitalization risk, a 10% RR reduction with Molnupiravir translates to a 0.5% ARR - statistically significant but clinically negligible. Paxlovid’s 70% RR yields a 3.5% ARR - clinically meaningful. Also, drug interactions aren't just 'high' with Paxlovid - they're pharmacologically catastrophic in polypharmacy elderly. The real issue is not efficacy - it's precision medicine infrastructure. We're still using 1990s triage logic in a 2025 pharmacogenomic landscape.
Paige Basford November 26, 2025
Okay but like… I just got my second booster and now I’m kinda scared to even sneeze 😅 I’m 68 and on a statin, so Paxlovid’s off the table for me. I’m so glad Molnupiravir exists - it’s not perfect, but at least I don’t have to stress about my meds clashing. Also, I read somewhere that Ensitrelvir might be coming to the US soon? Fingers crossed! I’d love to have a better option than the ‘spare tire’ drug. 🤞
Ankita Sinha November 26, 2025
This is such an important post! I’m from India and we’ve been using Molnupiravir widely because Paxlovid is too expensive and hard to get. But honestly? I’ve seen people recover faster with it than I expected - especially when they start early. I think we need to stop treating it like a ‘bad’ drug and start treating it like a tool. Every tool has its place. And if you’re in a village with no hospital nearby? Molnupiravir is a lifeline. We need more access, not more judgment.
Kenneth Meyer November 28, 2025
It’s fascinating how we’ve turned a medical intervention into a hierarchy of worth. Paxlovid = hero. Molnupiravir = failure. Remdesivir = outdated. But what if the real question isn’t which drug is best - but which human is being served? We’ve built a system that rewards efficiency over equity. The fact that someone’s access to a life-saving pill depends on their insurance, their age, or whether they take blood pressure meds… that’s not a pharmacological problem. That’s a moral one.
Donald Sanchez November 29, 2025
ok but like… paxlovid rebound is REAL. i had it. felt fine, took the full course, then bam - fever back at day 9. felt like the virus was trolling me 😭 also molnupiravir is basically just letting the virus mutate in your body? like… is that safe? 🤯 also why is no one talking about how remdesivir costs more than my rent? 💸
Abdula'aziz Muhammad Nasir November 29, 2025
In Nigeria, we don’t have the luxury of choosing between antivirals. If you can get *any* oral antiviral within 48 hours, you’re lucky. Molnupiravir is often the only option available in rural clinics. I’ve seen elderly patients recover with it where IV access was impossible. Calling it 'second-tier' is a privilege of wealth. For many, it’s the first - and only - line of defense. Let’s not dismiss utility because it’s not glamorous.
Tara Stelluti November 30, 2025
so like… i just found out my mom’s doctor gave her molnupiravir instead of paxlovid and i’m screaming into the void. like WHY? she’s 70, diabetic, and on lisinopril - paxlovid’s a no-go, sure, but didn’t they just say molnupiravir is barely better than placebo? this feels like medical malpractice. i’m so mad. 🤬
william volcoff December 2, 2025
I think the real takeaway here is that we’ve been asking the wrong question. It’s not 'which drug is best?' - it’s 'which drug is right for *this* person?' The post does a great job of breaking down the trade-offs. But we need more systems that make those decisions easy for primary care docs - not just for the ones who read Reddit. A simple algorithm in the EHR: 'If on statin? → Molnupiravir. If no interactions? → Paxlovid. If hospitalized? → Remdesivir.' Done. No guesswork. No delays.
Freddy Lopez December 3, 2025
There’s a quiet dignity in being the backup plan. Molnupiravir doesn’t get the headlines, the accolades, or the viral TikTok explainers. But it’s there - in the small-town pharmacy, in the hands of the elderly who can’t afford to miss a dose, in the pregnant woman’s doctor’s office where it’s not an option but the *absence* of it would be a tragedy. Sometimes, the most important thing isn’t being the best - it’s being there when no one else can be.