Missing a dose of your blood pressure pill or forgetting to take your insulin isn’t just a slip-up-it’s a risk. In the U.S., about half of people don’t take their medications as prescribed, and that leads to 125,000 preventable deaths every year. It’s not about laziness or forgetfulness. It’s about complexity, cost, and confusion. The good news? There are tools that actually work. Not just flashy apps or fancy pill boxes. Real solutions that fit into your life, not the other way around.
Why Medication Reminders Matter More Than You Think
Let’s be clear: forgetting to take your meds isn’t a minor issue. It’s a public health crisis. The Centers for Disease Control says medication non-adherence causes up to 25% of hospital stays. That’s not just inconvenient-it’s expensive. The U.S. spends $300 billion a year on avoidable costs tied to people not taking their pills correctly. And it’s not just seniors. People in their 30s and 40s with diabetes, asthma, or mental health meds are just as likely to miss doses. The problem isn’t memory. It’s overload. Too many pills. Too many times a day. Too many confusing instructions.
Studies show that when people have a reliable reminder system, adherence jumps by 15% to 20%. But not all systems are equal. Some apps nag you until you turn them off. Some pill boxes get jammed. Some alarms go off at 3 a.m. because you set them wrong. The goal isn’t to add another chore. It’s to make taking your meds effortless.
App-Based Reminders: The Digital Pillbox
Smartphone apps have become the most common tool for medication reminders. They’re cheap, easy to set up, and often free. But not all apps are built the same. The best ones don’t just buzz you at 8 a.m. They learn.
Medisafe is the most downloaded app, with over 5 million users. It’s popular because it does more than remind you. It checks for dangerous drug interactions using a database of FDA-approved medications. One pharmacist test showed it flagged interactions with 99.2% accuracy. But it’s not perfect. Users report false alerts-like warning that prenatal vitamins conflict with Tylenol-which wastes time and causes stress. It also pushes premium upgrades hard. The free version works fine, but you’ll see pop-ups every few days.
MyTherapy stands out for people managing chronic conditions. It tracks not just pills, but symptoms, mood, and even blood pressure if you use a compatible device. It’s FDA-cleared for health data integration, which means it’s built for clinical use. Younger users love the streak-tracking feature-like a fitness app for meds. If you’re on a long-term treatment plan, this one helps you see progress, not just reminders.
EveryDose uses an AI assistant named Maxwell to answer questions like, “Can I take this with coffee?” It pulls from a database of over 10,000 medications. But users say the interface feels clunky. Seniors struggle to navigate it. It’s powerful, but not intuitive.
And now, Apple’s Medications app (built into iOS 17.2) is changing the game. It syncs with your Health app and flags interactions using CDC data. No download needed. Just open Health, tap Medications, and scan your prescription labels. Over 12 million people used it in the first month. It’s simple, private, and doesn’t sell your data.
Physical Organizers: When Tech Isn’t Enough
Not everyone wants to stare at a phone all day. Some people, especially older adults, prefer something they can hold. That’s where physical pill organizers come in.
PillDrill’s Smart Medication System is one of the most advanced. It’s a plastic box with 28 compartments, each with a light that blinks when it’s time to take a pill. It syncs with an app, so caregivers can get alerts if a dose is missed. It costs $129.99. That’s steep, but for someone on five different meds, it’s worth it. Users report fewer missed doses and less anxiety about running out.
But there’s a catch. Loading the box is tricky. One study found 29% of users made mistakes when filling it for complex regimens-like taking different pills at different times. If you’re not careful, you can end up with two doses in one slot. It’s not foolproof.
Hero’s Pill Dispenser is another option. It’s a motorized box that opens compartments automatically. It costs $99.99 upfront, then $30 a month to use. It’s designed for Medicare users and has shown a 92% adherence rate in clinical trials. But the monthly fee adds up. And if your Wi-Fi goes out, it stops working.
Simple, low-tech organizers still have value. A plastic box with seven slots-one for each day-is cheap, reliable, and doesn’t need batteries. If you’re only taking one or two pills a day, this might be all you need.
Alarms and Notifications: The Oldest Trick That Still Works
Before apps, people used alarms. Still do. And surprisingly, the built-in alarm apps on your phone are more effective than you think.
A Duke University study found that using iOS Reminders or Android Clock alarms improved adherence by 43%. That’s not bad. But here’s the problem: 68% of people with cognitive issues-like early dementia or brain injury-can’t use them properly. They forget to set them. Or set them for the wrong time. Or turn them off because they go off too often.
For those who can use them, the trick is consistency. Set alarms for the same time every day. Don’t just set one. Set two. One at 8 a.m. and another at 8:15 a.m. That way, if you sleep through the first, the second catches you. Label each alarm with the pill name. “AM Insulin” instead of “Alarm 1.”
Smart speakers help too. Amazon’s Alexa skill for PillPack lets you say, “Alexa, did I take my blood pressure pill?” and it checks your schedule. In trials, it cut errors by 31%. Voice reminders work best for people who already use Alexa or Google Assistant daily.
What Actually Works? The Real Rules
After reviewing hundreds of user reports and clinical studies, here’s what consistently leads to better adherence:
- Use a weekly pill checker. Every Sunday, sit down with your meds and make sure your organizer matches your prescription. This reduces errors by 53%.
- Enroll a caregiver. If someone else-your spouse, child, or friend-gets alerts when you miss a dose, your 90-day adherence jumps from 62% to 88%.
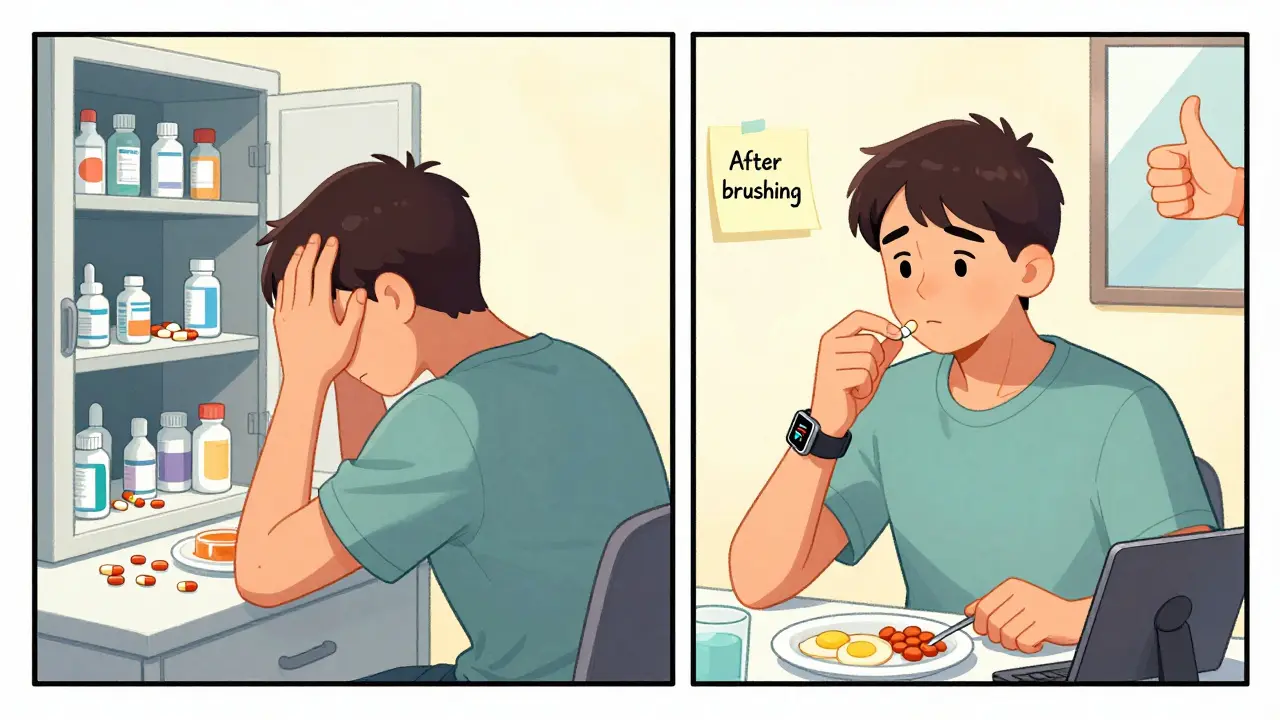
- Link your meds to a daily habit. Take your pill right after brushing your teeth or with your morning coffee. That habit sticks better than an alarm.
- Use biometric integration. If you wear an Apple Watch or Fitbit, sync your meds to it. Users who do this are 22% more consistent.
- Don’t rely on one method. Use an app and a pill box. Or an alarm and a caregiver. Redundancy saves lives.
Also, avoid notification fatigue. If you’re getting 10 alerts a day, you’ll turn them all off. Start with one or two. Add more only if you need them.
The Hidden Cost: Data, Privacy, and Burnout
Free apps aren’t free. A 2023 Princeton study found 63% of free medication apps sell your data-when you took your pill, where you are, even your health symptoms. If privacy matters to you, stick with Apple’s app or paid tools like MyTherapy, which don’t monetize user data.
And don’t underestimate burnout. One Johns Hopkins study found 61% of users disable alerts within 30 days because they’re too frequent or not personalized. The best apps adjust. If you take your pill at 8:30 a.m. every day, the app should learn that and stop buzzing at 8 a.m.
What’s Next? AI, Medicare, and the Future
The market is shifting fast. In 2023, Medicare started paying $15 a month to cover FDA-approved adherence tools. That’s why apps like Care4Today Connect are being used in 89% of HIV clinics and 47% of cancer centers. They’re not just tools-they’re part of care plans.
Next year, Medisafe plans to launch “AdherenceScore,” an AI feature that predicts when you’re likely to miss a dose. It uses 27 behavioral signals-like how often you open the app, whether you respond to alerts, even your sleep patterns. It’s not perfect, but early tests show 89% accuracy.
But don’t get caught in the hype. The best tool is the one you’ll use. A $10 pill box with a sticky note on top? That’s better than a $50 app you never open.
Final Tip: Start Simple
You don’t need to overhaul your life to get better at taking meds. Try this:
- Write down every pill you take, with time and dose.
- Buy a 7-day pill organizer (under $10 at any pharmacy).
- Set one alarm on your phone labeled with the name of your most important pill.
- Ask a family member to check in once a week.
Do that for two weeks. If it works, add more. If it doesn’t, try a different tool. There’s no one-size-fits-all. But there is a solution that fits you.
What’s the best medication reminder app for seniors?
For seniors, Medisafe is the top choice because of its caregiver-sharing feature, large button interface, and 24/7 live chat support. It’s designed for people who may not be tech-savvy. The "MedFriend" option lets a family member get alerts if a dose is missed, which reduces anxiety for both the user and their loved ones. Apple’s built-in Medications app is also excellent if they use an iPhone-it’s simple, no login needed, and doesn’t track data.
Can I use my smart speaker to remind me to take my pills?
Yes, but with limits. Amazon’s PillPack Alexa skill and Google Assistant integrations can remind you to take pills and let you check your schedule with voice commands. They work best if you already use Alexa or Google Home daily. But they can’t replace a physical pill organizer or app. Voice reminders are great for confirmation-like asking, "Alexa, did I take my blood pressure pill?"-but not reliable as a primary system.
Are pill organizers worth the money?
If you take more than three pills a day at different times, yes. A simple $10 plastic organizer helps avoid mix-ups. Smart ones like PillDrill or Hero cost more but reduce errors and let caregivers monitor you remotely. For people on complex regimens-like chemotherapy or multiple chronic conditions-they’re not a luxury, they’re a safety tool. But if you only take one or two pills daily, a sticky note on your mirror or a phone alarm is enough.
Why do some medication apps give false drug interaction warnings?
Many apps use broad databases that flag any possible interaction, even if it’s harmless. For example, some apps warn that Tylenol and prenatal vitamins interact-but that’s not true. These apps are trying to be safe, not accurate. Always double-check with your pharmacist. The best apps, like Medisafe and Apple’s Medications, use CDC and FDA data and let you report false alerts, which improves accuracy over time.
How can I stop forgetting meds when I travel?
Pack your pills in a travel-sized organizer with a clear label. Use your phone’s alarm, but set it for your local time zone. If you’re on a long trip, ask your pharmacy for a 30-day supply so you don’t need refills. Apps like MyTherapy and Medisafe let you sync your schedule across devices, so your phone and tablet both remind you. And always carry a printed list of your meds and doses in your wallet.
Do Medicare plans cover medication reminder tools?
Yes, starting in 2023, Medicare Part D now covers up to $15 per month for FDA-authorized adherence tools. That includes apps like Care4Today Connect and hardware like Hero’s Pill Dispenser. You’ll need a prescription from your doctor and to use a provider approved by Medicare. Check with your plan or visit Medicare.gov to see which tools are covered in your area.


All Comments
Daniel Dover February 15, 2026
Simplest solution: pill organizer + one alarm. No app needed. No data sold. Just do it.