Why Drug-Drug Interactions Are a Silent Threat for Seniors
Imagine taking five pills every morning - one for blood pressure, another for arthritis, a third for sleep, a fourth for acid reflux, and maybe a fifth for cholesterol. Now imagine one of those pills makes another less effective. Or worse - causes dizziness, confusion, or a dangerous drop in blood pressure. This isn’t rare. It’s everyday life for millions of older adults.
Drug-drug interactions (DDIs) happen when two or more medications react in a way that changes how they work. In younger people, these reactions are often mild or unnoticed. In seniors, they can land someone in the hospital - or worse. About 35% of hospital admissions for people over 65 are linked to medication problems, and half of those could have been avoided.
Why? Because aging changes how the body handles drugs. The liver slows down. Kidneys filter less. Body fat increases, water decreases. All of this means medications stick around longer, build up, and hit harder. Older adults are up to 50% more likely to have a bad reaction than younger people. And with 40% of seniors taking five or more prescriptions, the odds of a dangerous mix go up fast.
The Most Dangerous Drug Mixes for Seniors
Not all drugs are equally risky. Some combinations are like matchsticks near gasoline. The most common and dangerous interactions happen with drugs that affect the heart and brain.
- Heart drugs + blood thinners: Mixing warfarin with certain antibiotics or NSAIDs like ibuprofen can cause dangerous bleeding.
- Sedatives + opioids: Combining sleep aids like zolpidem with painkillers like oxycodone increases the risk of falls, breathing problems, and even death.
- Anticholinergics + dementia meds: Medications like diphenhydramine (Benadryl) or oxybutynin can worsen memory and confusion in people with Alzheimer’s or mild cognitive impairment.
- Diuretics + NSAIDs: Taking water pills with ibuprofen or naproxen can suddenly crash kidney function - a silent but deadly combo.
According to the Beers Criteria a list of medications to avoid or use with extreme caution in adults 65 and older, updated every two years by the American Geriatrics Society, over 30 drug classes are flagged as risky for seniors. These include certain antipsychotics, benzodiazepines, and even some over-the-counter sleep aids.
The STOPP criteria a validated tool that identifies 114 potentially inappropriate prescriptions for older adults, with 94% accuracy in spotting risks adds even more detail - like warning against prescribing proton pump inhibitors longer than eight weeks without review, or using multiple drugs that all slow the heart rate.
Why Seniors Get Too Many Medications
It’s not that doctors are careless. It’s that the system is broken.
Most seniors see multiple doctors - a cardiologist, a rheumatologist, a neurologist, a primary care provider. Each one treats a single condition. Few ask: "What else is this patient taking?" And even fewer talk to each other.
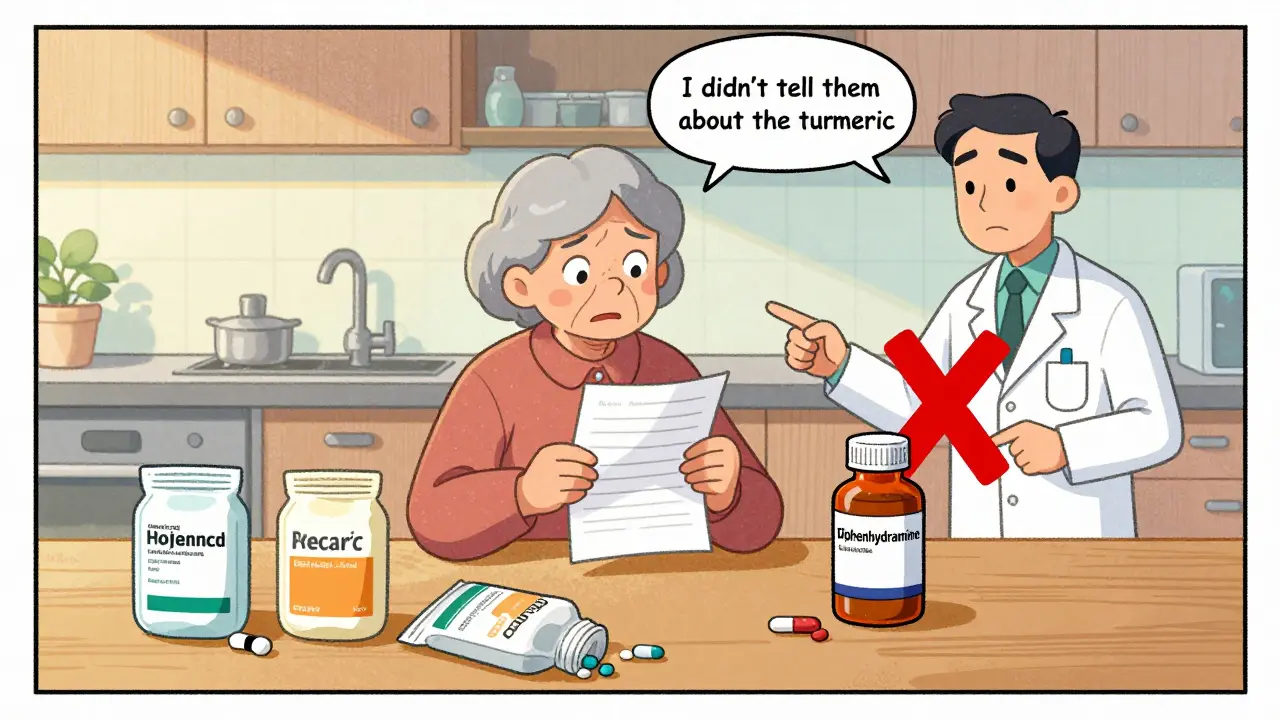
More than two-thirds of older adults use multiple pharmacies. One fills the blood pressure script. Another fills the painkiller. No one sees the full picture. And patients rarely mention what they buy over the counter - like melatonin, turmeric, or fish oil. In fact, 68% of seniors don’t tell their doctor about supplements, even though many interact with prescriptions.
Then there’s the "prescribing cascade." A side effect - say, dizziness from a blood pressure drug - gets treated with another drug, like an anti-nausea pill. That pill causes dry mouth, so they get a saliva substitute. Now they’re on five drugs for one original problem.
And it’s not just prescriptions. The average senior takes 14 different medications a week - including vitamins, OTC pain relievers, and herbal products. None of this is tracked in one place.
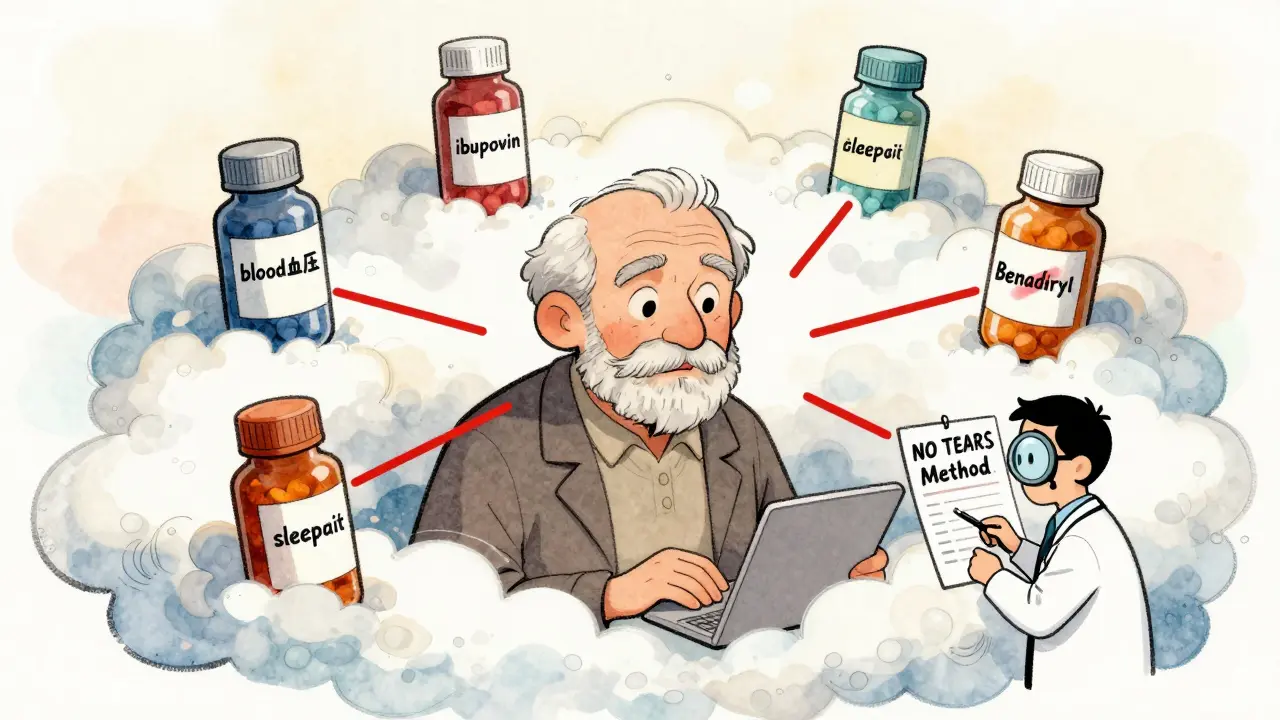
The NO TEARS Method: A Simple Way to Cut Unnecessary Meds
There’s a tool that works - and it’s not high-tech. It’s called NO TEARS a seven-step framework for reviewing medications in older adults. It’s designed for busy clinicians but can be used by families too.
- Need - Is this drug still needed? Maybe the arthritis pain is gone. Maybe the sleep aid was only meant for three weeks.
- Optimization - Is the dose right? Many seniors need lower doses because their bodies process drugs slower.
- Trade-offs - Do the benefits outweigh the risks? Is that statin really worth the muscle pain and memory fog?
- Economics - Can the patient afford it? If they’re skipping doses because of cost, it’s not working.
- Administration - Are they taking it right? Are pills too big? Do they need a pill organizer?
- Reduction - Can we stop one? Start by cutting the lowest-value drug - often the one with the most side effects.
- Self-management - Do they understand why they’re taking it? If not, they won’t stick with it.
A 2021 study found that using NO TEARS during hospital discharge reduced medication errors by 41% in patients over 75. It doesn’t require fancy tech. Just time, questions, and a willingness to say: "Maybe we don’t need this anymore."
How to Talk to Your Doctor About Meds
If you’re caring for an older adult, here’s what to do at the next visit:
- Bring a complete list of everything: prescriptions, OTC drugs, vitamins, herbs, even eye drops and patches.
- Ask: "Which of these can we stop?" Don’t assume everything is necessary.
- Request a medication review - specifically ask for a check using the Beers Criteria or STOPP.
- Insist on one pharmacy for all prescriptions. That way, the pharmacist can flag interactions.
- Ask if any new drug is being added because of a side effect from another. That’s a red flag.
- Set a 3-month check-in for any new medication. If it’s not helping, it’s probably hurting.
Doctors need 15 minutes per visit just to review meds for seniors on five or more drugs. If your appointment is 10 minutes, ask for a longer one. Or schedule a separate medication management visit.

The Role of Technology - And Its Limits
Hospitals are starting to use AI tools that scan every prescription against a database of known interactions. Adoption jumped from 22% in 2020 to 47% in 2023. These tools can catch things humans miss.
But they’re not perfect. Most are trained on data from younger, healthier people. They don’t fully account for how aging changes drug metabolism. And they can’t tell if a patient is skipping pills because they can’t afford them - or if they’re taking a neighbor’s leftover painkiller.
Even worse: only 28% of drug labels include specific interaction warnings for older adults. The FDA requires interaction info, but doesn’t require it to be clear for seniors. So a doctor might see a warning - but not realize it applies to someone with kidney disease or low body weight.
That’s why tech can help - but can’t replace human judgment. The best system is still a doctor who knows the patient, listens, and asks the right questions.
What’s Changing - And What’s Still Broken
The good news? Things are slowly improving.
The FDA now recommends including older adults in clinical trials - but only 18% of new drug applications between 2018 and 2022 actually did. That means we’re still guessing how most new drugs work in seniors.
The 2025 update to the Beers Criteria will add 15 more medications requiring kidney-based dose adjustments. That’s progress.
Medicare’s Medication Therapy Management program has helped 11.2 million people since 2022, reducing hospitalizations by 15.3%. But only a fraction of eligible seniors enroll.
The biggest gap? Education. Only 38% of U.S. medical schools have a dedicated course on geriatric pharmacology. By 2026, that should rise to 65% - but that’s still too little, too late for millions now on dangerous mixes.
Until doctors are trained to think holistically - not just by organ system - and until patients feel safe telling the truth about what they’re taking, DDIs will keep hurting seniors.
What You Can Do Today
You don’t need a degree to prevent a deadly drug interaction. Here’s your action plan:
- Make a real list - every pill, patch, drop, and supplement. Write it down. Don’t rely on memory.
- Take it to one pharmacy - and ask the pharmacist to review it.
- Ask your doctor: "Which of these can I stop?" Be ready for them to say: "Maybe none." Push back if you feel something isn’t helping.
- Watch for new symptoms - dizziness, confusion, fatigue, nausea - and link them to recent med changes.
- Use a pill organizer. Set phone alarms. Ask a family member to help check doses.
- Never start a new drug without asking: "What’s the plan if this doesn’t work?"
Medications aren’t harmless. They’re powerful tools - and like any tool, they can hurt if used wrong. For seniors, the stakes are higher. But so is the power of a simple conversation, a clear list, and the courage to ask: "Do I really need this?"

All Comments
Kunal Majumder January 11, 2026
Man, I’ve seen this play out with my dad. Five pills at breakfast, three at night, and he swears he’s fine. Then he starts nodding off in the chair and we find out he’s been taking Benadryl for allergies on top of his sleep med. No one ever asked him about the OTC stuff. Just started using NO TEARS last month - cut two meds already. He’s walking better, not dizzy. Simple stuff, but nobody talks about it.
McCarthy Halverson January 11, 2026
One pharmacy. Always. And bring the actual bottles. Doctors don’t believe lists. Pills in hand? That’s the only proof that sticks.
Aurora Memo January 12, 2026
I appreciate how this breaks it down without fear-mongering. My mom’s on seven meds and I’ve been too scared to ask if any could go. This gives me a real script to use at her next appointment. Thank you for the NO TEARS framework - it feels doable now.
Ian Cheung January 13, 2026
Look I get it meds are dangerous but come on we’re talking about people who’ve lived 70+ years they’ve probably taken worse than ibuprofen with warfarin back in the day like when they were popping aspirin like candy and smoking three packs a day with no lab tests or pill organizers
Now we’re treating them like glass figurines and blaming the system when they just need to toughen up a little
My grandma took digoxin and lisinopril and a whole bunch of junk for 20 years and she’s still gardening at 92 so maybe it’s not the drugs it’s the fear
Christine Milne January 15, 2026
It is an egregious failure of American healthcare infrastructure that geriatric pharmacology is not a mandatory component of medical education. The FDA's lack of enforceable labeling standards for elderly-specific interactions constitutes a de facto negligence protocol. Furthermore, the reliance on the Beers Criteria - a non-binding guideline developed by a private society - is statistically indefensible as a clinical standard. This article, while well-intentioned, dangerously underestimates the systemic malfeasance embedded in our pharmaceutical regulatory framework.
neeraj maor January 16, 2026
Did you know that 87% of these 'drug interactions' are fabricated by Big Pharma to sell more pills? The liver doesn't slow down with age - it's just been poisoned by decades of processed food and glyphosate. The real problem? The FDA approves every new drug with a hidden trigger that makes seniors dependent on more meds. That's why they keep adding new warnings - it's not to help you, it's to keep you buying.
And don't get me started on pharmacies. They're all owned by the same 3 corporations that also make the drugs. Your 'one pharmacy' solution? It's a trap. They're logging everything. They're selling your data. You think your pill organizer is safe? It's probably transmitting your meds to a server in Switzerland.
Jake Kelly January 17, 2026
I’ve been using the NO TEARS method with my aunt since last winter. We started with the ‘Need’ step - turned out she’d been taking melatonin for 4 years because she thought it was ‘natural’ and therefore safe. Turns out it made her dizzy and she’d been falling. Stopped it. No more falls. No more new meds to fix the side effects. Just simple, quiet adjustments.
Ashlee Montgomery January 18, 2026
It’s not just about the drugs. It’s about who gets to decide what ‘necessary’ means. A 78-year-old woman on a fixed income is told she needs a $300/month statin to prevent a heart attack that may never come. Meanwhile, her loneliness, her lack of movement, her diet of canned soup - none of that gets addressed. We treat symptoms like puzzles to solve with pills, not symptoms of a life lived in isolation and neglect.
Maybe the real DDI is between medicine and meaning.
Dwayne Dickson January 20, 2026
Let’s be honest - the entire geriatric pharmacology industry is a profit engine disguised as care. The Beers Criteria? A marketing tool. The STOPP guidelines? A bureaucratic checkbox. And yet, here we are, praising a seven-step checklist as if it’s revolutionary. The real innovation would be paying doctors to spend 45 minutes with each elderly patient - not 10. But that would require dismantling fee-for-service. And nobody wants that. Not the insurers. Not the hospitals. Not even the patients who think more pills = better care.
Ritwik Bose January 21, 2026
Thank you for this thoughtful and meticulously researched piece. 🙏 The NO TEARS framework is a compassionate and pragmatic approach that aligns with the dignity of aging. I have shared this with my elderly uncle in Kolkata - he has been on six medications for five years. We are scheduling a pharmacist review next week. Small steps, but meaningful ones. 🌿
Paul Bear January 23, 2026
There is a statistically significant correlation between polypharmacy and cognitive decline, particularly when anticholinergic burden exceeds 100 DDDs per day. The prescribing cascade is not anecdotal - it is a documented iatrogenic phenomenon. Furthermore, the underrepresentation of elderly cohorts in phase III trials violates the Belmont Principle of Justice. The FDA's failure to mandate age-stratified interaction labeling constitutes a breach of the 2018 Geriatric Medication Safety Act. This is not a matter of opinion - it is a failure of regulatory oversight.
Bradford Beardall January 24, 2026
Hey, I’m from the Philippines and we don’t have all this fancy Beers Criteria stuff. But my abuelita? She takes three pills - one for blood pressure, one for sugar, and one for her knees. And she’s fine. Why? Because she eats rice, walks every morning, and talks to her neighbors. Nobody in her village has a pill organizer. They just know what works. Maybe the answer isn’t more guidelines - it’s more community. We’ve lost that.