Why Timing Matters More Than You Think When Flying
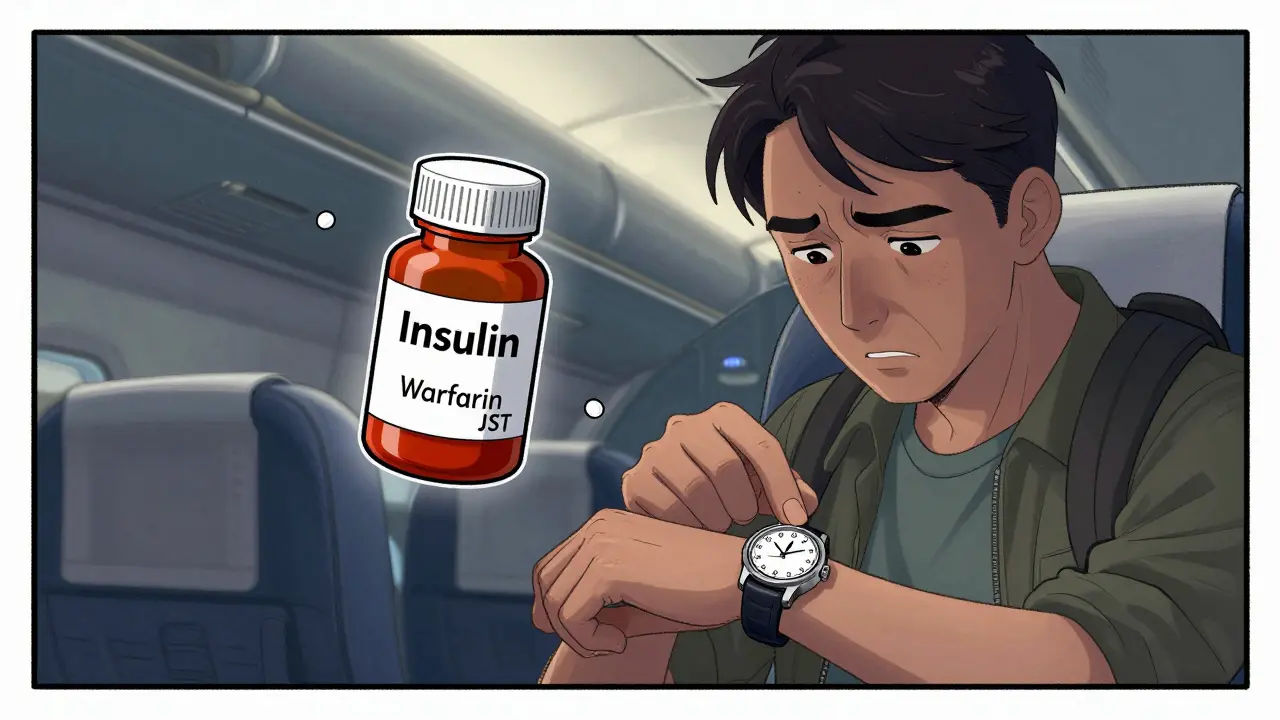
Skipping a pill by an hour might seem harmless-but for some medications, even a 30-minute delay can throw your whole system off. If you’re taking drugs like insulin, warfarin, anti-seizure meds, or immunosuppressants, your body relies on strict timing to stay stable. Flying across time zones? That’s when things get risky. The CDC says 62% of travelers crossing five or more time zones struggle with medication timing, and for some, it leads to hospital visits. This isn’t about forgetting your pills. It’s about understanding how your body reacts when your clock changes but your meds don’t.
Know Your Medication’s Risk Level
Not all time-sensitive meds are the same. The key is figuring out how narrow your medication’s therapeutic window is. Drugs with half-lives under 8 hours need to be taken twice a day-and missing a dose by even a few hours can drop your levels too low. Insulin is one of the most common. If you take it every 4 hours and miss one because of a flight delay, your blood sugar can crash. Warfarin? Your INR levels can swing dangerously if you take it at the wrong time relative to meals or other meds. Anti-epileptics like phenytoin or levetiracetam can trigger seizures within 12-24 hours of a missed dose. Immunosuppressants like tacrolimus or cyclosporine? A single late dose can make your body reject a transplanted organ.
Here’s the quick breakdown:
- High risk (exact timing needed): Insulin, warfarin, anti-seizure drugs, immunosuppressants, oral chemotherapy
- Moderate risk (1-2 hour window okay): Antibiotics, blood pressure meds, thyroid pills, some antidepressants
- Low risk (flexible): Vitamins, most OTC pain relievers, antihistamines (except sedating ones)
Check with your pharmacist or doctor before you go. If you’re on any of the high-risk meds, don’t guess-plan.
Stick to Home Time for the First 48 Hours
Most people think they should switch to local time right away. That’s not always right. For meds with short half-lives, experts at Johns Hopkins recommend staying on your home time zone schedule for the first 48 to 72 hours after landing. Why? Your body hasn’t adjusted yet. Your liver, kidneys, and metabolism are still running on your original clock. Taking insulin at 8 a.m. local time when your body expects it at 5 a.m. home time? That’s asking for trouble.
Example: You fly from Seattle (PST) to Tokyo (JST)-that’s 17 hours ahead. If you normally take your insulin at 7 a.m. and 7 p.m. Seattle time, keep doing it at those times-even if it’s 12 a.m. and 12 p.m. in Tokyo. Use your phone’s world clock app to track your home time. After 2-3 days, once your body starts adjusting to the new rhythm, slowly shift your doses by 1-2 hours per day until you’re synced with local time.
This doesn’t apply to all meds. If you’re on a long-acting drug like once-daily statins or some blood pressure pills, you can switch immediately. But if your med has to be taken multiple times a day and you feel shaky, dizzy, or off-chances are your timing’s off.
Use a Travel Medication App (And Don’t Rely on Memory)
Trying to calculate time zones in your head while jet-lagged? Bad idea. Apps like Medisafe (used by over 1.2 million people) automatically adjust your dosing schedule based on your flight itinerary. You enter your departure, arrival, and medication times, and it sends alerts in your home time zone until you’re ready to switch. Some even let you share your schedule with a family member or caregiver.
For those who prefer a physical tool, the MedTime Zone Watch ($34.99) shows two time zones at once-your home and destination. It’s simple, doesn’t need Wi-Fi, and works during long flights when your phone dies. No excuses.
Pro tip: Set two alarms for each dose-one for home time, one for local time. That way, if you accidentally switch time zones on your phone, you’re still covered.

Bring the Right Storage Gear for Temperature-Sensitive Meds
Insulin, some biologics, and certain antibiotics need to stay between 35°F and 46°F. A regular cooler won’t cut it. You need a medical-grade portable cooler that uses phase-change gel packs. The Travelport 3.0 keeps meds cold for up to 48 hours without power and is trusted by diabetics and transplant patients.
TSA lets you bring these through security-even if the ice packs are melted. Just tell the officer they’re for medical use. Keep your meds in their original bottles with labels. Don’t put them in checked luggage. Temperatures in the cargo hold can drop below freezing or rise above 100°F. One patient lost a month’s supply of insulin in 2023 because their bag was stored under the plane. Don’t be that person.
Know the TSA and FAA Rules-Before You Go
TSA allows all prescription and over-the-counter meds in your carry-on, no matter the quantity. Liquids over 3.4 oz are fine if they’re for medical use. You don’t need a doctor’s note, but having one helps if you’re questioned. Always keep meds in original containers with your name on the label. That’s non-negotiable.
FAA rules are stricter for pilots-but they matter for passengers too. Never fly after taking a new medication for the first time. Wait at least 48 hours to see how your body reacts. If you’re on sedating antihistamines like Benadryl or Unisom, wait 60 hours. These drugs can linger in your system and make you drowsy during or after the flight. That’s not just unsafe-it’s dangerous if you need to move quickly in an emergency.
Plan Your First Dose After Landing
The most common mistake travelers make? Not knowing when to take their first dose after landing. Do you take it right away? Wait until your usual time? That’s where confusion starts.
Here’s how to decide:
- If you’re crossing 1-3 time zones: Take your next dose at your usual time, adjusted for local time. Easy.
- If you’re crossing 4-8 time zones: Stick to home time for the first 48 hours. Take your dose at your home time, even if it’s 3 a.m. local time.
- If you’re crossing 8+ time zones: Use the 1-hour-per-time-zone method. For example, flying from New York to Sydney (15-hour difference)? Adjust your dose by 1 hour each day until you’re synced. On day 1, take it 1 hour earlier than home time. Day 2, 2 hours earlier. Keep going until you reach local time.
And never double up. If you miss a dose, don’t take two to make up for it. That’s how overdoses happen. Call your pharmacy or doctor if you’re unsure.

Carry a Medication List-In Writing
Emergency rooms in 83% of U.S. hospitals say a printed medication list saves lives. Write down:
- Brand and generic names of all meds
- Dosage and frequency
- Prescribing doctor’s name and phone
- Your pharmacy’s name and number
- Any allergies or reactions
Keep it in your wallet, your phone, and give a copy to a travel companion. If you pass out or can’t speak, this list is your lifeline.
What to Do If You Mess Up
Accidents happen. You oversleep. Your flight gets delayed. You forget your pills in your checked bag. Don’t panic. Here’s what to do:
- Call your pharmacy. They can advise on safe adjustments.
- Use a telehealth service like Teladoc or Amwell-they can consult with your doctor remotely.
- For insulin: Check your blood sugar every 2 hours. If it’s below 70 or above 250, seek help.
- For warfarin: Watch for unusual bruising, nosebleeds, or dark stools. Call your doctor immediately.
- For seizures or confusion: Go to the ER. Don’t wait.
Most pharmacies offer 24/7 advice lines. Save the number before you leave.
Future Tech Is Coming-But Don’t Wait for It
The FDA is testing digital medication passports that auto-adjust dosing based on your flight. They’re promising-but they’re still in pilot mode. Don’t rely on future tech. Right now, your best tools are planning, apps, and clear communication with your care team.
Final Checklist Before You Fly
- ☑️ Confirmed with your doctor or pharmacist how to adjust your meds
- ☑️ Pack meds in carry-on, in original bottles
- ☑️ Brought a medical cooler if needed (with gel packs)
- ☑️ Set up Medisafe or similar app with flight details
- ☑️ Printed medication list with doctor and pharmacy info
- ☑️ Know your first dose time after landing
- ☑️ Avoid sedating antihistamines before flying
- ☑️ Carried extra doses in case of delays
Traveling with time-sensitive meds isn’t about being extra careful. It’s about being smart. The difference between a smooth trip and a medical emergency is often just a few hours of planning.

All Comments
Isaac Jules January 7, 2026
This is the most half-baked medical advice I've seen on Reddit. Who the hell says 'don't guess-plan'? That's not advice, that's a slogan. And why the hell are we trusting Johns Hopkins like they're the FDA? I've been on insulin for 12 years and I've never heard of this 'home time for 48 hours' crap. My pump auto-adjusts. You're overcomplicating it.
Lily Lilyy January 7, 2026
Thank you so much for this guide. 🙏 I was so nervous about flying with my warfarin next week, but now I feel so much more confident. You've made something scary feel manageable. You're helping people live better lives. Keep sharing your wisdom!
Joann Absi January 7, 2026
AMERICA IS THE ONLY COUNTRY THAT DOES THIS RIGHT. 🇺🇸 Look at Europe - they just wing it with their meds and wonder why their hospitals are full. This is why we lead the world in medical innovation. If you're not using Medisafe, you're not trying. And if you're using a regular cooler? You're literally risking your life. #MedicationPatriot
Tom Swinton January 9, 2026
I just want to say, as someone who's been on cyclosporine since 2018 after my kidney transplant, this is the most comprehensive, thoughtful, and life-saving guide I've ever read on this topic. Seriously. I've been through three international trips and I wish I'd had this. The part about the 48-hour home time rule? That's gold. I didn't know that. I thought I was being careful by just taking it at the same clock time - turns out I was dangerously wrong. Thank you for taking the time to lay this out so clearly. I'm printing this out and taping it to my suitcase.
Gabrielle Panchev January 9, 2026
You say 'don't guess-plan' - but you literally just gave 12 different algorithms for when to take pills based on time zones. So which one is it? The 48-hour rule? The 1-hour-per-time-zone method? Or just 'ask your doctor'? Because if your advice is so nuanced that it needs a flowchart, maybe the problem isn't the traveler - maybe it's that the medical system doesn't give clear, unified guidance. Also, why is the FDA testing 'digital passports' and no one told us? Are we the beta testers?
Cam Jane January 11, 2026
You got this. Seriously. I used to panic every time I flew with my anti-seizure meds - until I started using Medisafe + the two-alarm trick. Set one for home time, one for local. You’ll never miss again. And don’t forget the printed list - I had mine in my wallet during a seizure in Paris. The paramedics said it saved my life. You’re not over-preparing. You’re being smart.
Dana Termini January 13, 2026
I appreciate how detailed this is. I’m on warfarin and I’ve always just winged it. Now I know I should’ve been more careful. I’m going to call my pharmacist tomorrow and get a printed schedule. I think this will help me sleep better at night.
Wesley Pereira January 14, 2026
So you're telling me I can't just take my insulin when I'm hungry on the plane? Like... that's a thing? 😏 I'm just sayin' - if your body can't handle a 2-hour shift, maybe it's not your meds that need adjusting... it's your life choices. But seriously, the MedTime Zone Watch is genius. I'm buying one. And yes, I spelled 'meds' wrong. You're welcome.
Amy Le January 16, 2026
This article is so American. 'Use a $35 watch to track time zones'? We have phones. We have AI. We have apps that can detect your location and auto-adjust. Why are we still using analog solutions? Also, 'don't put meds in checked luggage'? Newsflash: I'm flying economy with a 20lb carry-on limit. I can't carry 3 coolers, 2 watches, and a printed 12-page manifesto. This isn't advice - it's guilt-tripping.
Pavan Vora January 18, 2026
I am from India, and I take insulin. I used to be very scared to fly. But now I use my phone's world clock and set two alarms. I also carry my medicines in original bottles. Thank you for this guide. It is very helpful. I will share with my friends in Mumbai. 🙏
Stuart Shield January 18, 2026
Bloody brilliant. I’ve been on warfarin since my stroke and I’ve always thought the time zone thing was a myth - turns out I was just lucky. The part about the gel packs? Genius. I’ve seen someone’s insulin melt in a suitcase in Heathrow. It looked like soup. Don’t be that person. This is the kind of practical, no-nonsense advice that should be mandatory reading for anyone with a chronic condition.
Susan Arlene January 19, 2026
i just take my pills when i remember. sometimes i forget. sometimes i dont. sometimes i take two. sometimes i dont. life is chaos. the body adapts. maybe we're all just overthinking it.
Ashley S January 20, 2026
Why are we even letting people fly if they need this many rules? If your meds are that fragile, maybe you shouldn't be traveling at all. This isn't a travel guide - it's a 'don't leave your house' pamphlet. And why does everyone need an app? My grandma took her pills for 40 years without a smartphone. Maybe we're just getting too soft.
Jeane Hendrix January 22, 2026
I'm on tacrolimus and I just read this and I'm like... holy crap. I've been switching to local time immediately. I thought I was being smart. I just called my transplant team and they said I've been risking rejection. I'm gonna use Medisafe now and get the watch. Thank you. This literally changed my life. I'm gonna send this to my whole family.