When your doctor hands you a prescription for a generic drug, what do you think? Maybe you wonder if it’s the same as the brand-name version. Maybe you’ve heard stories about generics not working as well. You’re not alone. Nearly 54% of patients say their doctors never or seldom explain why they’re switching to a generic. And that silence isn’t harmless-it directly shapes whether you’ll take the medicine, stick with it, or stop altogether.
Why Patients Doubt Generics-Even When They’re Safe
Most people don’t realize that the FDA requires generic drugs to meet the same strict standards as brand-name drugs. To get approved, a generic must contain the same active ingredient, work the same way in the body, and be absorbed at the same rate and extent. The FDA’s acceptable range for bioequivalence is 80% to 125%. That means a generic can be slightly less or more absorbed than the brand, but still be just as effective and safe. This isn’t a loophole-it’s science. Yet, a 2015 study found that nearly 30% of patients believed brand-name drugs were more effective. Why? Because they’ve been told-directly or indirectly-that they are. Pharmaceutical marketing, vague warnings from pharmacists, and even TV ads that highlight brand names over generics have built a quiet but powerful narrative: if it’s cheaper, it must be worse. The real problem isn’t the drug. It’s the conversation-or lack of one-that happens before you leave the office.Communication Is the Biggest Factor in Acceptance
Here’s the surprising truth: It’s not cost, not side effects, not even past experiences that most influence whether you’ll take a generic. It’s what your clinician says-or doesn’t say-when they prescribe it. A 2011 study of nearly 2,000 patients found that the single strongest predictor of generic acceptance was whether the provider talked about it. Patients who received even a brief explanation were 37% more likely to fill and keep taking their generic prescription. That’s bigger than any price discount. Bigger than any marketing campaign. And it’s not just doctors. Pharmacists matter too. When a pharmacist explains the switch, 92% of patients accept the generic. When they don’t? That number drops to 68%. That’s a 24-point gap from one conversation. It’s not enough to say, “We’re switching you to the generic.” That’s like handing someone a new pair of shoes and saying, “They’re cheaper.” Without context, the brain fills in the blanks-and often, it assumes the worst.What Effective Communication Actually Sounds Like
Good communication isn’t just about facts. It’s about tone, timing, and trust. Research shows that the most effective messages include four key elements:- “This generic has the same active ingredient as the brand.” Not “it’s similar.” Not “it’s close.” Same. Identical. That word matters.
- “The FDA requires it to work the same way in your body.” Mentioning the FDA isn’t just about authority-it’s about trust. People know the FDA doesn’t approve things lightly.
- “It saves you about 80%-so you’re not paying more than you need to.” Cost matters, but only when it’s framed as a benefit, not a compromise.
- “Some people worry about generics because they’ve heard rumors. I’ve seen them work just as well for years.” This addresses the elephant in the room: the nocebo effect.
One Doctor’s 10-Minute Talk Changed Everything
On Reddit, a patient shared this story: “My cardiologist sat down for 10 minutes. Showed me the FDA bioequivalence data. Said he takes generics himself. Told me why it’s not a downgrade-it’s the same medicine.” That patient has been on the generic for two years with no issues. Compare that to a Healthgrades review: “My pharmacist just handed me a different pill. When I got headaches, he said, ‘Some people react to generics.’ I stopped taking it for three weeks.” The difference? One conversation built confidence. The other built fear. Analysis of over 4,200 patient reviews found that 78% of positive experiences mentioned clinician communication as the turning point. Meanwhile, 89% of negative experiences blamed poor or missing communication. It’s not about being perfect. It’s about being present.
Who’s Most at Risk-and Why
Not everyone reacts the same way. A 2016 NIH survey found that non-Caucasian patients were 1.7 times more likely to distrust generics. Patients with annual incomes under $30,000 were 2.3 times more likely to prefer brand names. This isn’t about intelligence or education. It’s about history. Marginalized communities have been overprescribed, under-treated, and misled by the healthcare system for decades. When a new pill is handed to them without explanation, it’s easy to see it as another form of neglect. Culturally competent communication-using the right language, acknowledging past harm, and listening without judgment-reduces skepticism by 41% in these groups. That’s not just good practice. It’s essential.Barriers Doctors and Pharmacists Face
You might think, “Why don’t they just explain it?” The answer is complicated. Time is a big one. A 2020 study found doctors spend an average of just 1.2 minutes per patient on generic discussions-less time than it takes to fill a prescription. Many clinicians also lack confidence. Only 54% of physicians correctly answered basic questions about FDA bioequivalence standards in a 2019 survey. Nearly 40% admitted they weren’t sure if generics worked as well for conditions like epilepsy or heart disease. And then there’s the fear of backlash. Some providers worry that pushing generics will upset patients-or make them feel like they’re being cheapened. But research shows the opposite. Patients appreciate honesty and clarity. They don’t mind being offered a lower-cost option. They mind being talked to like they’re a number.What’s Working: Real Solutions That Deliver Results
Kaiser Permanente’s “Generic First” program didn’t just encourage doctors to prescribe generics. It trained them to explain them. They created standardized scripts, embedded prompts in electronic records, and made communication part of performance reviews. Result? 94% generic utilization. $1.2 billion saved per year. The American Pharmacists Association developed a 15-minute training module for pharmacists. After the training, patient understanding jumped from 42% to 87%. Communication time dropped by 38%. Even tech is helping. Epic Systems launched the “Generic Confidence Score” in April 2024. When a provider opens a prescription, the system asks: “Did you explain the FDA bioequivalence? Did you mention cost savings? Did you address concerns?” It doesn’t force the conversation-but it nudges it into the room.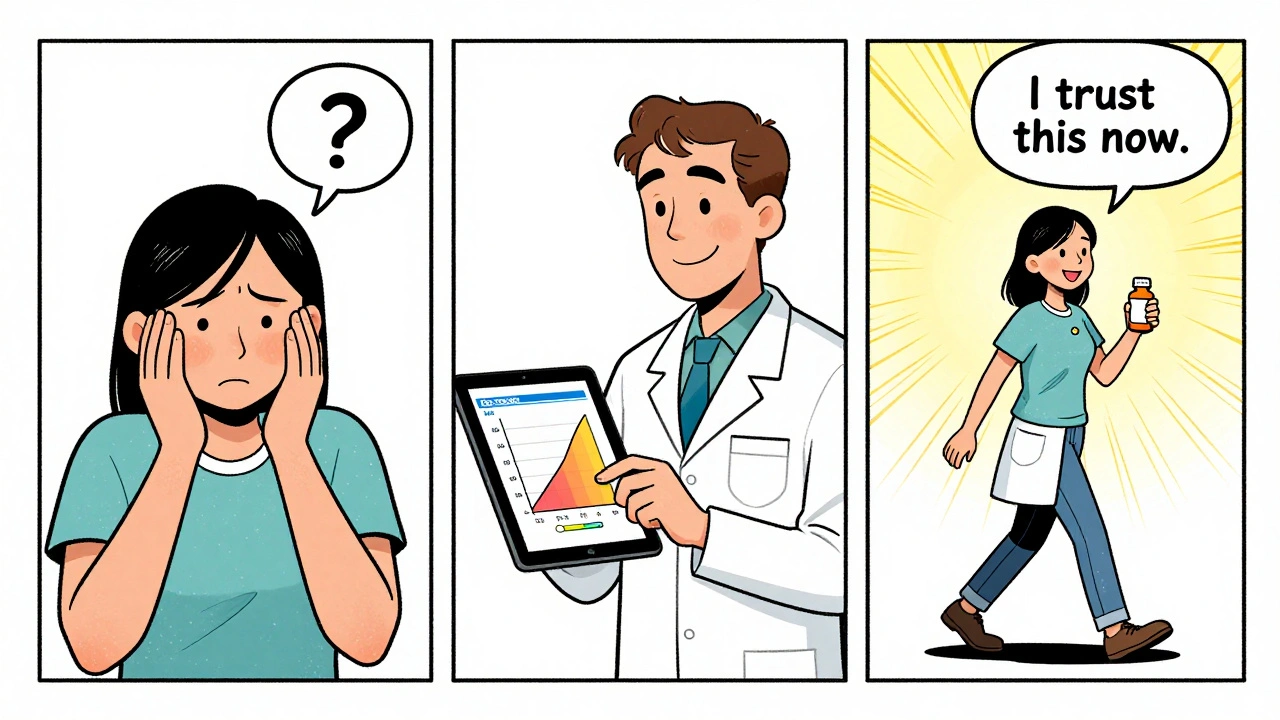
Why This Matters Beyond the Prescription
Generics make up 90% of all prescriptions filled in the U.S. But they cost only 23% of what brand-name drugs do. That’s $37 billion saved every year. Yet, brand-name preference requests have doubled since 2010-from 12% to 23%. That’s not because generics are failing. It’s because communication is failing. The FDA, AMA, and CDC are now treating clinician communication as a public health priority. In 2025, Medicare Part D will start tying reimbursement to how well providers explain generics. That’s a game-changer. This isn’t about saving money. It’s about saving health. When patients stop taking their meds because they don’t trust them, hospitalizations go up. Complications rise. Costs soar.What You Can Do
If you’re prescribed a generic:- Ask: “Is this exactly the same as the brand?”
- Ask: “Has the FDA approved it to work the same way?”
- Ask: “Why are we switching?”
- Ask: “Have you taken this yourself?”
- Don’t assume they know. Most don’t.
- Use clear, confident language. Avoid “try this” or “see how it goes.”
- Address fears head-on. Say: “I know some people worry about generics. Here’s why they’re safe.”
- Use the FDA’s free patient materials-they’re written at a 6th-grade reading level and translated into 12 languages.
Final Thought
A pill is just a pill. But the story behind it? That’s what sticks. When clinicians take five minutes to explain, they’re not just prescribing medicine. They’re prescribing trust. And trust? That’s the most powerful drug of all.Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generics to contain the same active ingredient, work the same way in the body, and be absorbed at the same rate as the brand-name version. The acceptable range for bioequivalence is 80% to 125%, meaning the body processes them identically for therapeutic purposes. Thousands of studies confirm they are equally effective and safe.
Why do some patients feel worse after switching to a generic?
This is often the nocebo effect-when expecting side effects leads to actually feeling them. If a patient believes generics are inferior, their brain can interpret normal sensations as side effects. Studies show patients who receive clear, confident explanations from their provider report significantly fewer adverse events after switching.
Can pharmacists legally substitute generics without telling me?
In most cases, yes-unless the prescription says “dispense as written” or “no substitution.” But federal and state laws require pharmacists to offer counseling on generic substitutions. In 27 states, they’re legally required to explain the switch. Even where it’s not mandatory, best practice demands it.
Why do some doctors still prefer brand-name drugs?
Some doctors were trained when generics were less common or less trusted. Others may have been influenced by pharmaceutical marketing. A 2019 survey found only 54% of physicians correctly understood FDA bioequivalence standards. Lack of training and outdated beliefs still linger, but awareness is improving with new guidelines and training programs.
Do generics cost less because they’re lower quality?
No. Generics cost less because they don’t require expensive research, marketing, or patent protection. The active ingredient is already proven. The FDA still inspects manufacturing facilities just as rigorously as for brand-name drugs. Lower price = less overhead, not lower standards.
How can I know if my generic is FDA-approved?
All FDA-approved generics are listed in the Orange Book, which is publicly available. You can also ask your pharmacist for the manufacturer’s name and look it up on the FDA website. Look for the “AB” rating-this means it’s rated as therapeutically equivalent to the brand.
Is it safe to switch between different generic brands?
Yes. All FDA-approved generics must meet the same bioequivalence standards. Switching between different generic manufacturers is common and safe. The FDA monitors for consistency, and any significant deviation triggers an investigation. There’s no evidence that switching between approved generics causes harm.


All Comments
Maria Elisha December 11, 2025
lol i just got handed a generic pill and the pharmacist said 'it's the same' and walked away. i took it anyway. no side effects. weird.
Iris Carmen December 11, 2025
i always ask my doc if it's the same as the brand. they always say yes. i still feel like i'm getting the cheap version tho. idk man. maybe im just paranoid.
Noah Raines December 11, 2025
the nocebo effect is real af. i had migraines after switching to generic ibuprofen. stopped taking it. went back to brand. migraines gone. turned out i was just stressed and blamed the pill. dumb.
Lauren Dare December 13, 2025
the FDA's 80-125% bioequivalence window is not a scientific consensus-it's a regulatory compromise masquerading as precision. you're telling me a 20% variance in absorption is 'identical'? that's not medicine, that's actuarial math dressed in a lab coat.
and don't get me started on the 'generic first' programs. they're cost-driven, not patient-driven. the system doesn't care if you trust it-it just wants you to comply.
the real issue isn't communication-it's systemic erosion of autonomy under the guise of efficiency.
precious amzy December 13, 2025
One must consider the ontological implications of pharmaceutical equivalence: if two substances are pharmacologically indistinguishable, yet culturally perceived as ontologically disparate, does the latter not constitute a hermeneutic distortion of medical reality? The patient’s belief in inferiority, though empirically unfounded, remains phenomenologically real-a lived epistemology that transcends bioequivalence metrics. To reduce trust to a behavioral nudge is to mistake the map for the territory.
Moreover, the invocation of the FDA as an epistemic authority is itself a colonial gesture: a technocratic institution, unaccountable to the cultural epistemologies of marginalized communities, imposes its epistemic framework upon those historically disenfranchised by its very architecture. The solution is not better scripts, but epistemic justice.
And yet-how does one communicate the deconstruction of pharmaceutical hegemony in 1.2 minutes? One cannot. Hence, the system persists. Not because patients are ignorant, but because the system is designed to be inertial.
Let us not mistake clarity for coercion. Let us not mistake compliance for cure.
Trust is not a variable to be optimized. It is a covenant.
Stacy Tolbert December 15, 2025
i cried when my pharmacist explained the generic thing. not because i was happy. because no one had ever taken the time before. i've been on meds for 12 years and this was the first time someone looked me in the eye and said 'this is just as good'.
it made me feel like a person. not a number. not a cost center.
why is that so rare?
Katherine Rodgers December 17, 2025
so the solution to doctors being lazy and uninformed is... more tech nudges? epic systems is gonna save healthcare? lol. next they'll put a little checkbox: 'did you remind them generics aren't poison?'
the real problem? doctors are overworked, underpaid, and trained to treat symptoms, not people. you can't fix systemic burnout with a pop-up.
also, 94% generic use? sounds like coercion, not trust. someone's getting paid to push pills, not to talk.
Andrea Beilstein December 17, 2025
the pill doesn't care if you believe in it but your body does
we live in a world where trust is the active ingredient and science is just the label
when the system stops treating patients like customers and starts treating them like humans the generics will work better because the people will believe it
you can't fix a broken relationship with a brochure
the real generic is empathy
the brand name is control
and we're all just trying to survive the prescription