Why Your Generic Pill Looks Different This Month
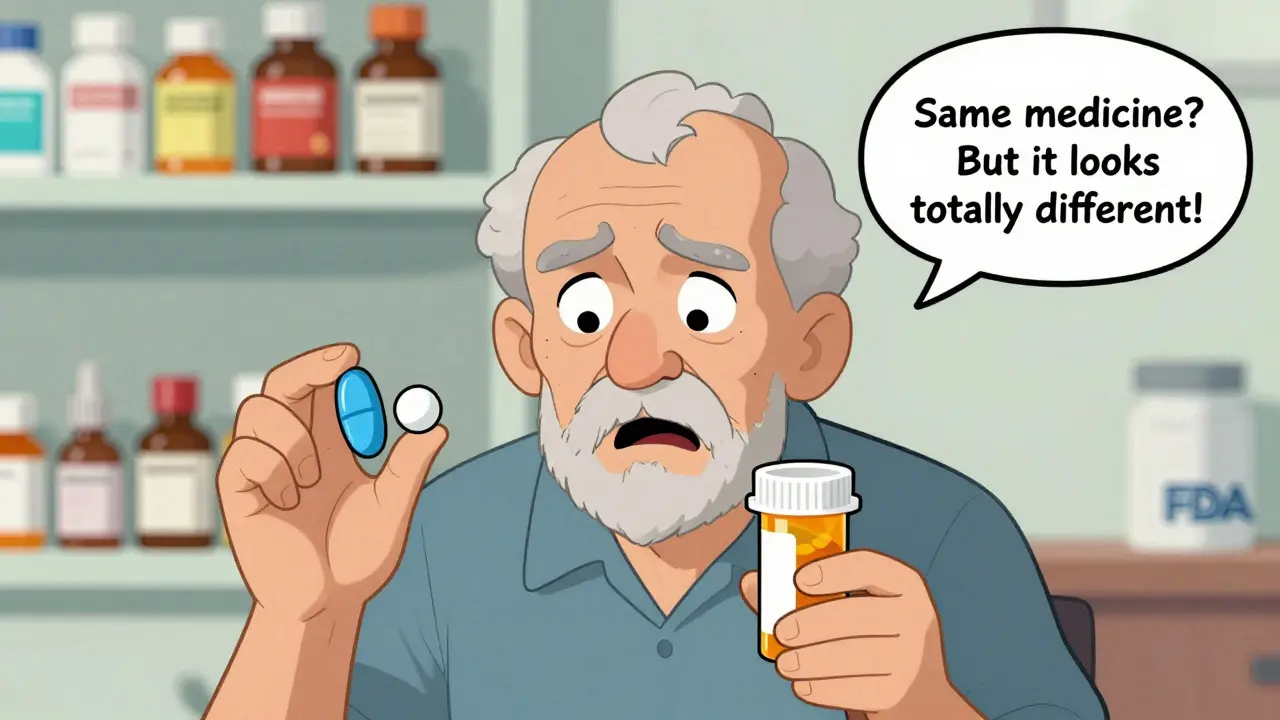
You’ve been taking the same medication for years. Then one day, you open your prescription bottle and the pill looks totally different. Maybe it’s white instead of blue. Maybe it’s oval instead of round. You pause. Did they give you the wrong drug? Is this safe? You’re not alone. Generic pill appearance changes happen all the time - and they’re completely legal. But they’re also one of the most overlooked risks to patient health.
In the U.S., over 70% of prescriptions are filled with generic drugs. These pills work the same way as their brand-name versions. Same active ingredient. Same strength. Same effect. But they don’t look the same. And that’s by design.
Why the Law Forces Generic Pills to Look Different
It’s not a mistake. It’s not a glitch. It’s the law.
Under U.S. trademark rules, generic drug manufacturers can’t make their pills look exactly like the brand-name version. That’s to avoid confusion in the marketplace - and to protect the brand’s intellectual property. So if you’ve ever taken Zoloft (blue, oval tablets), you know what the original looks like. But when you switch to a generic version, you might get a white, round pill with a different marking. Or a green capsule. Or a peach-colored tablet. All of them contain sertraline. All of them work the same. But none of them look the same.
The FDA requires generics to match brand-name drugs in active ingredients, dosage, strength, and how they’re absorbed by the body. But appearance? Not required. Color, shape, size, even the imprint code - all up to the manufacturer. And since multiple companies can make the same generic drug, your pill can change every time your pharmacy switches suppliers.
How Often Do These Changes Happen?
More often than you think.
A patient in Los Angeles reported nine different appearances for the same medication over 15 years. Another person switched from flat, neon-orange potassium pills to white, capsule-shaped ones - and thought she’d been given the wrong drug. Reddit users in r/pharmacy share stories weekly: "I almost stopped my blood pressure meds because they turned pink."
According to a study in the Annals of Internal Medicine, 34% of patients stopped taking their medication after a color change. That number jumps to 66% after a shape change. A 2022 survey by the American Pharmacists Association found that 42% of patients experienced at least one appearance change in their regular meds within a year. Nearly 30% of them were worried enough to question whether the drug still worked.
Why does this matter? Because people don’t take pills based on science. They take them based on memory, routine, and trust. If the pill doesn’t look familiar, the brain says: "This isn’t right." And for many, that’s enough to quit.

Which Medications Are Most Likely to Change?
Some drugs are notorious for appearance flips. Here are a few common ones:
- Sertraline (Zoloft): Blue, green, white, oval, round - all versions contain the same antidepressant.
- Metformin: White or pink, round or oblong. One batch might be scored, the next isn’t.
- Lisinopril: White, pink, or peach tablets. Often changes between refills.
- Gabapentin: No two manufacturers use the same shape or color. Patients report confusion even after years of use.
- Levothyroxine: Even small appearance changes can trigger anxiety in thyroid patients who rely on precise dosing.
These aren’t rare cases. They’re standard practice. The FDA approves dozens of generic versions for each drug. Pharmacies choose the cheapest option each month. And if your pharmacy switches from one manufacturer to another - even for a few cents per pill - your medication changes appearance.
Are Generic Pills Still Safe?
Yes. Absolutely.
The FDA doesn’t cut corners on safety. Every generic drug must prove it’s bioequivalent - meaning it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. The FDA tests for purity, stability, and how the drug breaks down in your body. Inactive ingredients like dyes, fillers, and coatings can differ - and that’s what changes the color or texture. But they don’t affect how the drug works.
Still, patients worry. And that worry is real. A 2023 analysis by the National Community Pharmacists Association found that 63% of independent pharmacies now have pill identification programs in place - up from 32% in 2020. Why? Because pharmacists are seeing the fallout firsthand: missed doses, ER visits, and patients who stop taking their meds altogether.
What You Can Do to Stay Safe
You can’t stop appearance changes. But you can protect yourself.
- Keep a written list of all your meds. Include the name, dose, and what each pill looks like. Take this list to every doctor’s visit. If your pill changes, you’ll have proof it’s still the same drug.
- Ask your pharmacist to explain any change. Don’t assume it’s a mistake. Say: "This looks different. Is it still the same medication?" They’re trained to answer this.
- Use online pill identifiers. Sites like Medscape’s Pill Identifier let you search by color, shape, and imprint. Just snap a photo or describe the pill - it’ll tell you what it is.
- Check your prescription label. The manufacturer name and NDC code are listed there. If the manufacturer changes, the pill will look different. That’s normal.
- Flag changes to your doctor. If you’ve stopped taking a pill because it looked wrong, tell your provider. They need to know.
Pharmacies are catching on. Since 2018, the number of pharmacies that include appearance change notices with refills has jumped from 45% to 78%. Some even print a small note on the label: "This is a different manufacturer. Same medication. Same effect."
What’s Being Done to Fix This?
Experts have been sounding the alarm for years. In a 2014 letter to the ACP Journal, Drs. Uhl and Peters wrote: "Bioequivalent generic drugs that look like their brand-name counterparts enhance patient acceptance." The FDA agrees - in theory. But they’re stuck.
Changing the law to let generics look like brand-name drugs would break trademark rules. That’s a legal minefield. But the FDA is moving slowly. The MODERN Labeling Act of 2020 gives them more power to update generic drug labels with new safety info. And in 2025, the FDA began requiring manufacturers to update labeling based on emerging safety data - a step toward better communication.
Still, the biggest barrier isn’t science. It’s law. And until trademark rules change, appearance changes will keep happening.
Bottom Line: Don’t Panic. Stay Informed.
Generic pills are safe. They’re effective. And they save patients billions of dollars each year.
But if your pill looks different, don’t assume it’s wrong. Don’t assume it’s dangerous. Don’t assume it’s the same as last time - because it might not be. But it’s still the same medication.
The real danger isn’t the pill. It’s the silence around it. If you don’t know what’s happening, you might stop taking your meds. And that’s when health risks rise.
Keep your list. Ask your pharmacist. Use the tools. And remember: a different-looking pill doesn’t mean a different drug. It just means you need to be a little more careful.

All Comments
Mandy Vodak-Marotta February 2, 2026
I swear, I thought I was going crazy last month when my levothyroxine went from white oval to this tiny peach circle. I stared at it for 20 minutes, Googled ‘is this poison?’ and nearly called 911. Then I checked the label - same NDC, same dose. My pharmacist just shrugged and said ‘different manufacturer, same magic.’ I still don’t trust it, but I take it. I keep a photo of each version on my phone now. My brain needs to see the pill before it believes it’s real. 🤷♀️
caroline hernandez February 3, 2026
From a clinical pharmacy standpoint, this is a documented adherence crisis. The bioequivalence data is solid - AUC and Cmax within 80–125% CI - but the cognitive dissonance from visual mismatch triggers non-adherence at alarming rates. We’ve implemented visual pill ID cards at our clinic: patients photograph their current script, and we archive it. When the pill changes, we cross-reference the imprint code (e.g., ‘M 15’ vs ‘E 15’) and confirm via FDA’s DailyMed database. It’s not ideal, but it’s mitigating 30% of ER visits related to ‘wrong pill’ panic.