Every year in the U.S., about 2 million fractures happen because bones have become too weak. Most of these aren’t from car crashes or sports injuries-they’re from simple falls, like stepping off a curb or slipping in the bathroom. These are called fragility fractures, and they’re a direct result of bone loss, often from osteoporosis. The good news? Many of these fractures can be prevented. The bad news? A lot of the advice people follow is outdated, misleading, or even harmful.
Calcium and Vitamin D: The Basics You’ve Heard Before (But Probably Got Wrong)
You’ve seen the ads: “Take calcium and vitamin D to keep your bones strong.” It sounds simple. But here’s the truth: taking low doses of these supplements-like 400 IU of vitamin D and 1,000 mg of calcium-does almost nothing to prevent fractures in healthy, community-dwelling adults. That’s not opinion. That’s what the U.S. Preventive Services Task Force found after reviewing 8 major studies. Their conclusion? Don’t waste your money on low-dose supplements if you’re not at high risk.
So when do they work? Only in people who are truly deficient. If your blood level of vitamin D is below 20 ng/mL, or you’re not getting enough calcium from food (less than 700 mg/day), then adding 800-1,000 IU of vitamin D3 and 1,000-1,200 mg of calcium daily can reduce your risk of hip fractures by up to 16%. That’s not magic-it’s fixing a deficiency.
The problem? Most people who take supplements don’t know their levels. They’re guessing. And that’s where things go wrong. The Women’s Health Initiative, which tracked over 36,000 postmenopausal women, found no reduction in fractures with low-dose supplements. In fact, those taking calcium had a 17% higher risk of kidney stones. And a 2022 study showed that 18% of adults over 50 in the U.S. are taking more than the safe upper limit of 4,000 IU of vitamin D daily-without medical supervision.
Who Actually Needs Supplements? (It’s Not Everyone)
Not every older adult needs supplements. But some groups absolutely do:
- People living in nursing homes or long-term care facilities
- Those with a history of falls or previous fractures
- Individuals with very low sun exposure or dark skin (which reduces vitamin D production)
- People who don’t eat dairy, leafy greens, or fortified foods regularly
- Anyone with a blood test showing vitamin D below 20 ng/mL
The landmark 1992 study by Chapuy in France showed a 43% drop in hip fractures among nursing home residents who got 800 IU of vitamin D and 1,200 mg of calcium daily. Why? Their baseline vitamin D was only 12.3 ng/mL-severely deficient. That’s not the average American. That’s someone who rarely leaves their room, eats processed meals, and has no sunlight.
But if you’re active, eat a decent diet, and get outside a few times a week, you likely don’t need supplements. Your body can make enough vitamin D from 15-20 minutes of sun on your arms and face. And calcium? A cup of yogurt, a serving of kale, or a few ounces of canned salmon with bones gives you more than enough.
Bone-Building Medications: The Real Game-Changers
If supplements are the foundation, bone-building medications are the reinforcement. These aren’t “miracle cures,” but they’re the only treatments proven to dramatically reduce fracture risk in people with osteoporosis.
There are two main types:
- Antiresorptives (slow bone loss): Bisphosphonates (like alendronate and zoledronic acid) and denosumab
- Anabolics (build new bone): Teriparatide, abaloparatide, romosozumab
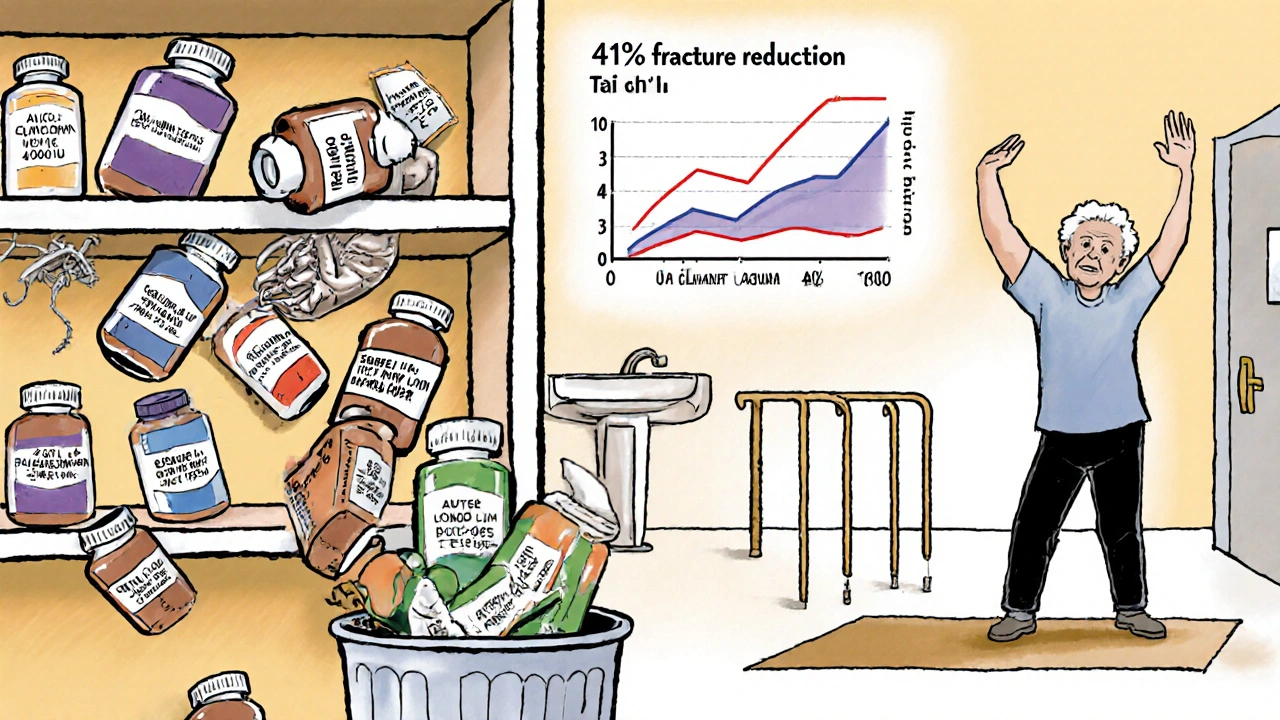
Bisphosphonates are the most common. Alendronate (Fosamax) cuts vertebral fracture risk by 44% and hip fractures by 20-50% over 3-5 years. Zoledronic acid, given as an annual IV infusion, reduces hip fractures by 41% in just 18 months. These drugs work by putting the brakes on bone breakdown.
Anabolic drugs like teriparatide (Forteo) and abaloparatide (Tymlos) do the opposite-they actually stimulate new bone growth. The 2021 DATA-Switch trial showed that starting with teriparatide for a year, then switching to an antiresorptive, led to a 73% greater reduction in new vertebral fractures than using bisphosphonates alone. These are for people with severe osteoporosis-those who’ve had multiple fractures or very low bone density.
But they’re not without risks. Bisphosphonates can rarely cause jawbone damage (osteonecrosis) or unusual thigh bone fractures after long-term use (5+ years). That’s why dentists now check your oral health before you start. And while these side effects are extremely rare (less than 1 in 1,000), they’re real. That’s why doctors don’t prescribe them to everyone.
Who Should Be on Medication? (The FRAX® Tool Explained)
Not everyone with low bone density needs medication. That’s where the FRAX® tool comes in. It’s not a fancy machine-it’s a free online calculator developed by the World Health Organization. You plug in your age, sex, weight, height, whether you’ve had a prior fracture, if you smoke, drink alcohol, or take steroids-and it gives you your 10-year risk of a major fracture.
In the U.S., if your risk is over 20%, you’re a candidate for medication. In the UK, the threshold is 15%. Why the difference? Because healthcare systems weigh risk differently. But the point is: don’t rely on your T-score alone. A low T-score doesn’t automatically mean you need drugs. Your overall risk does.
For example: A 70-year-old woman with a T-score of -2.5 (osteoporosis) but no history of falls, no smoking, and no family history of hip fracture might have a FRAX® score of 12%. She might be better off with lifestyle changes and monitoring. Another 70-year-old woman with the same T-score but a previous wrist fracture, 2 drinks a day, and steroid use? Her FRAX® score might be 35%. That’s a clear signal: medication is needed.
The Hidden Problem: People Stop Taking Their Meds
Here’s the uncomfortable truth: even the best drugs won’t help if you don’t take them. A 2022 meta-analysis found that more than half of people stop taking oral bisphosphonates within one year. Why? Side effects. Nausea, heartburn, and stomach pain are common. Some people feel fine for a few months, then think, “I don’t need this anymore.”
That’s dangerous. Bone density doesn’t rebuild overnight. You need consistent treatment for at least 3-5 years to see real fracture reduction. And if you stop, your risk goes right back up.
That’s why many doctors now prefer annual IV infusions (like zoledronic acid) for patients who struggle with pills. No daily or weekly dosing. No stomach upset. Just one 15-minute visit a year. And for those who can’t tolerate bisphosphonates, denosumab (Prolia) is given as a shot every six months.
But even these have limits. You can’t take them forever. After 3-5 years, doctors often pause treatment to reassess. That’s called a “drug holiday.” It’s not quitting-it’s smart management.
What Really Works: Beyond Pills and Supplements
Medications and supplements are only part of the story. The most powerful tool for fracture prevention is still movement.
- Weight-bearing exercise (walking, stair climbing, dancing)
- Resistance training (light weights, resistance bands)
- Balance training (Tai Chi, yoga, heel-to-toe walks)
These don’t just strengthen bones-they prevent falls. And falls cause fractures. A 2020 study showed that older adults who did balance and strength training 3 times a week reduced their risk of falling by 30%. That’s more effective than any supplement.
Also, don’t ignore your home. Over half of all fractures happen at home. Get rid of loose rugs. Install grab bars in the bathroom. Add nightlights. Wear shoes with grip, even indoors. These simple changes save lives.
What to Do Right Now
If you’re over 50 and haven’t had a bone density test, ask your doctor. If you’ve had a fracture after age 50, get tested immediately. Don’t wait. If you’re on supplements, ask for a blood test to check your vitamin D level. If it’s below 30 ng/mL, talk about higher-dose therapy. If it’s above 30, you might not need extra.
Don’t take calcium supplements unless you’re sure you’re not getting enough from food. If you are, pair it with vitamin D. And if your doctor says you need a bone-building medication, ask about the risks, benefits, and alternatives. Don’t just accept a prescription-understand why it’s right for you.
Fracture prevention isn’t about popping pills. It’s about knowing your risk, using the right tools, and staying active. The science is clear. Now it’s time to act on it.
Do calcium and vitamin D supplements prevent fractures in everyone?
No. Low-dose supplements (400 IU vitamin D and 1,000 mg calcium) don’t reduce fracture risk in healthy, community-dwelling adults. They only help people who are deficient-those with blood vitamin D levels below 20 ng/mL, low calcium intake, or who live in institutions. For others, they offer no benefit and may increase kidney stone risk.
Which bone-building medication is best?
There’s no single “best” drug-it depends on your risk level and health. For moderate risk, bisphosphonates like alendronate are first-line. For high risk or previous fractures, anabolic drugs like teriparatide or romosozumab are more effective. For those who can’t take pills, denosumab (injections every 6 months) or zoledronic acid (annual IV) are good options. Your doctor will choose based on your FRAX® score, medical history, and tolerance.
Can I get enough calcium and vitamin D from food?
Yes, for most people. One cup of yogurt has 300 mg calcium. Three ounces of canned salmon with bones has 180 mg. One cup of cooked kale has 179 mg. For vitamin D, fatty fish like salmon and mackerel are good sources, and fortified milk or orange juice help. Sun exposure (15-20 minutes on arms and face) also makes vitamin D. Supplements are only needed if your diet is poor or you’re deficient.
Are bone medications safe long-term?
Most are safe for 3-5 years. Bisphosphonates carry a rare risk of atypical femur fractures or jawbone damage after 5+ years, so doctors often pause treatment after that. Anabolic drugs are limited to 2 years due to safety data. Regular monitoring and dental checkups reduce risks. The benefits of preventing a hip fracture far outweigh the small chance of rare side effects.
Why do so many people stop taking their bone meds?
Side effects. Oral bisphosphonates can cause heartburn, nausea, and stomach pain. Some people feel fine after a few months and assume they don’t need them anymore. But bone density doesn’t improve quickly-treatment needs to be consistent for 3-5 years. Switching to an annual IV or biannual injection can improve adherence.
Is walking enough to strengthen bones?
Walking helps, but it’s not enough on its own. To build bone strength, you need weight-bearing and resistance exercises-like lifting light weights, using resistance bands, or doing squats and step-ups. Balance training (Tai Chi, heel-to-toe walks) also reduces fall risk. Combine movement with medication and nutrition for the best protection.
What’s the ideal vitamin D level for fracture prevention?
The Endocrine Society recommends 30-50 ng/mL for fracture prevention. Levels below 20 ng/mL are considered deficient and require treatment. Levels above 50 ng/mL offer no extra benefit and may increase risks. A simple blood test can tell you where you stand.


All Comments
Ancel Fortuin November 19, 2025
Oh wow, another ‘science says’ article from the pharmaceutical lobby. Next they’ll tell us sunlight is a myth and we should all take vitamin D pills while sitting in a Faraday cage. Meanwhile, people in rural Africa and India who never saw a supplement in their life have stronger bones than my neighbor who takes 5 different pills every morning. The real fracture risk? Trusting doctors who get paid by drug companies. 🤡
Hannah Blower November 20, 2025
Let’s be brutally honest: the entire ‘supplement culture’ is a performative act of pseudo-healthiness. People take calcium because it makes them feel like they’re doing something, not because it’s biologically necessary. The real tragedy isn’t osteoporosis-it’s the delusion that swallowing a pill absolves you of responsibility. Your bones don’t care about your Instagram wellness routine. They care about load, movement, and real nutrition. You can’t supplement your way out of a sedentary, processed-food lifestyle. It’s not medicine-it’s magic thinking with a label.
Gregory Gonzalez November 22, 2025
Interesting how the article casually mentions the Women’s Health Initiative like it’s gospel, yet ignores the fact that those trials used synthetic calcium carbonate and inferior forms of vitamin D2. Real vitamin D3? From real sun exposure? Real dietary calcium from bone-in fish and fermented dairy? That’s not in the FDA-approved playbook, is it? The system doesn’t want you to know that food > pills, and movement > marketing. They profit from your ignorance. And you’re happily handing them your credit card.
Ronald Stenger November 23, 2025
Look, I get it. You wanna be ‘woke’ about health. But let’s not pretend this is some global conspiracy. In America, we have the best medical science in the world. The USPSTF isn’t some rogue group-it’s peer-reviewed, evidence-based. If you’re a 70-year-old woman who’s fallen before, you need meds. If you’re a 55-year-old who walks his dog daily and eats salmon, then sure, skip the pills. But don’t confuse your personal anecdote with population-level data. We don’t run healthcare on feelings. We run it on statistics. And the stats say: treat the high-risk, not the lucky.
Samkelo Bodwana November 24, 2025
I’ve lived in both Cape Town and Johannesburg, and I’ve seen elderly people here who’ve never taken a supplement but never fractured a bone either. They walk to market, carry heavy buckets, eat maize and beans, and get sun every day. Meanwhile, in the U.S., people sit in air-conditioned offices, drink fortified orange juice, and pop pills like candy. Maybe the problem isn’t just bone density-it’s how disconnected we are from our bodies. Movement isn’t exercise. It’s survival. And maybe, just maybe, we’ve over-medicalized something that used to be natural. Let’s not throw out science-but let’s not forget wisdom either.
Emily Entwistle November 25, 2025
YESSSS this is so important!! 🙌 I’m 62 and my doctor finally listened when I said I was taking 5000 IU of D3 and felt like a zombie. Got tested-my level was 48 ng/mL. She said ‘stop, you’re fine!’ and now I just eat yogurt, walk in the sun, and do yoga. No more pills. My hips feel better than they have in 10 years. 💪🌞 Also, grab bars = life saver. My aunt broke her hip because of a rug. Don’t be her. 😘
Duncan Prowel November 26, 2025
While the empirical evidence presented is largely robust, one must acknowledge the methodological limitations inherent in the cited cohort studies-particularly the homogeneity of the populations under observation. The applicability of findings derived from postmenopausal American women to, say, elderly men in South Asia or indigenous populations with distinct genetic and epigenetic profiles remains an open question. A universal protocol, while administratively convenient, risks pathologizing normal variation. Personalized medicine, grounded in biomarker assessment and functional mobility metrics, remains the ethical imperative.
Bruce Bain November 28, 2025
Man, I used to take calcium like it was candy. Then I started walking my dog every morning and doing squats while brushing my teeth. No more pills. My bones feel stronger. My doctor was shocked when I told him I stopped everything. He said, ‘Well, I guess you’re just lucky.’ I said, ‘No, I’m just not lazy.’ Simple stuff works. Don’t overcomplicate it. Walk. Eat real food. Get sun. Don’t trust ads.
Jonathan Gabriel November 28, 2025
Okay but… if you’re taking vitamin D and you’re not getting your levels checked, you’re basically playing Russian roulette with your kidneys. I had a friend who took 10,000 IU daily for 3 years because ‘more is better’-turns out his calcium was sky-high, he got kidney stones, and his parathyroid went haywire. The article’s right: test first. Don’t guess. And for god’s sake, stop taking calcium unless you’re eating like a cow. One yogurt a day > five pills. Also, teriparatide is wild-it’s basically synthetic parathyroid hormone. You’re injecting a hormone your body makes to build bone. That’s not magic, that’s biochemistry. But yeah, it’s expensive and you need to be monitored. Not for everyone. But for some? Life-changing.
Don Angel November 28, 2025
I’ve been on alendronate for 4 years. No stomach issues. No problems. My DEXA scan improved. I’m 71. I hike. I garden. I lift weights. I don’t take supplements. I eat eggs, spinach, and cheese. I take my pill every Sunday. It’s not hard. Don’t let fear of rare side effects stop you from doing what works. Your hip is worth it. And yes, I got my blood tested. My vitamin D is 38. Perfect. Don’t overthink it. Do the basics. Be consistent. That’s the real secret.
benedict nwokedi November 30, 2025
Who funds the WHO? Who funds the USPSTF? Who funds the studies that say supplements don’t work? Big Pharma. They make billions off bisphosphonates and IV infusions. They don’t want you to know that sunlight and whole foods cost nothing. They want you dependent. They want you on lifelong drugs. They want you scared of your own bones. And they’ve bought the science to prove it. The ‘evidence’ is manufactured. The truth? You don’t need pills-you need freedom from the system. Stop trusting institutions that profit from your fear.
deepak kumar November 30, 2025
In India, our grandparents never took calcium pills. They walked barefoot, drank milk from cows they raised, ate curry with leafy greens, and got sun every day. Their bones were strong. Now, urban youth take supplements because they sit all day and eat pizza. The problem isn’t the body-it’s the lifestyle. Medicine helps, yes. But movement, food, and rhythm matter more. Also, yoga and tai chi are not ‘alternative’-they’re ancient science. Use them. Not just pills.
Dave Pritchard December 2, 2025
For anyone reading this and feeling overwhelmed: you don’t have to do everything at once. Start with one thing. Walk outside for 15 minutes today. Eat one serving of yogurt. Ask your doctor for a vitamin D test. That’s it. No pressure. No guilt. Progress, not perfection. Bone health isn’t a race-it’s a lifelong habit. And you’re already ahead just by reading this. Keep going. You’ve got this.