Fluoroquinolone Side Effects Risk Calculator
Your Risk Assessment
This tool helps you understand your risk of tendon rupture or nerve damage when taking fluoroquinolone antibiotics (ciprofloxacin, levofloxacin, moxifloxacin). Based on your medical history, it calculates your risk level.
Risk Assessment Results
After entering your information, results will appear here.
Fluoroquinolone Antibiotics Can Cause Permanent Tendon and Nerve Damage
If you’ve been prescribed ciprofloxacin, levofloxacin, or moxifloxacin for a sinus infection, urinary tract infection, or bronchitis, you might think it’s just another antibiotic. But here’s the truth: these drugs carry risks that can change your life forever. Tendon rupture. Nerve damage. Chronic pain. These aren’t rare side effects - they’re well-documented, serious, and often irreversible. And they can happen even after you’ve stopped taking the pill.
The FDA added a black-box warning to all fluoroquinolones in 2008. By 2016, they made it clear: fluoroquinolone antibiotics should only be used when no other option exists. Yet, many doctors still prescribe them for simple infections. Millions of people have taken these drugs without knowing the hidden dangers. If you’ve had unexplained tendon pain or tingling in your hands and feet after taking one of these antibiotics, you’re not alone - and you’re not imagining it.
How Fluoroquinolones Damage Tendons
Fluoroquinolones don’t just kill bacteria - they disrupt collagen, the protein that holds your tendons together. This isn’t a mild soreness. It’s a breakdown of the tissue itself. The Achilles tendon is hit hardest - 90% of cases involve this one. But shoulders, hands, and knees can also fail.
Studies show tendon rupture happens in about 40% of people who develop fluoroquinolone-related tendinopathy. And half of those ruptures occur after you’ve finished the course. One man in Seattle took levofloxacin for a sinus infection. Twelve days later, both his Achilles tendons snapped while walking to his car. He needed surgery. Eleven months of rehab. He’s 52. No prior injuries. No sports. Just a 7-day antibiotic.
Onset timing is unpredictable. Most people feel pain within 6 days. But some don’t notice anything until 150 days later. That’s why doctors miss it. Patients blame aging. Physical therapy. Arthritis. But if you took a fluoroquinolone in the last six months and your tendon hurts - stop. Don’t stretch it. Don’t push through it. Get off your feet. See a specialist.
Who’s at Highest Risk
Not everyone gets tendon damage. But certain people are in the danger zone:
- Over 60 years old - your tendons naturally weaken, and fluoroquinolones speed up the process
- Taking steroids (like prednisone) - this combo increases rupture risk by 46 times
- Diabetic - high blood sugar already stresses connective tissue
- Have kidney disease - your body can’t clear the drug properly
- Had a prior tendon injury - your tendons are already vulnerable
These aren’t just theoretical risks. In FDA reports, 38% of tendon rupture cases involved people over 60. Nearly 17% were on corticosteroids. And 29% had kidney problems. If you fit even one of these categories, fluoroquinolones should be off the table.
Nerve Damage Isn’t Just Tingling - It’s Permanent
Peripheral neuropathy is another hidden danger. It starts with numbness, burning, or electric shocks in your feet or hands. It’s often called ‘pins and needles.’ But with fluoroquinolones, it doesn’t always go away. Up to 10% of patients develop long-term nerve damage that affects walking, balance, and daily life.
A 2021 study found symptoms appeared within the first month in most cases. But here’s the kicker: in 22% of cases, nerve pain didn’t show up until after the antibiotic was stopped. One woman in New Zealand took ciprofloxacin for a UTI. Three weeks later, her feet felt like they were wrapped in sandpaper. She couldn’t wear shoes. Her doctor said it was ‘stress.’ It took six months to get a diagnosis. Two years later, she still has chronic pain.
Unlike muscle soreness, nerve damage doesn’t heal quickly. The nerves don’t regenerate well. Some patients never recover fully. That’s why the FDA says these drugs can cause ‘disabling and potentially permanent’ side effects. This isn’t a side effect you can ‘tough out.’

Why Doctors Still Prescribe Them
Fluoroquinolones are fast, broad-spectrum, and cheap. For a doctor under time pressure, they’re tempting. But here’s what most don’t tell you: for 90% of cases, they’re unnecessary.
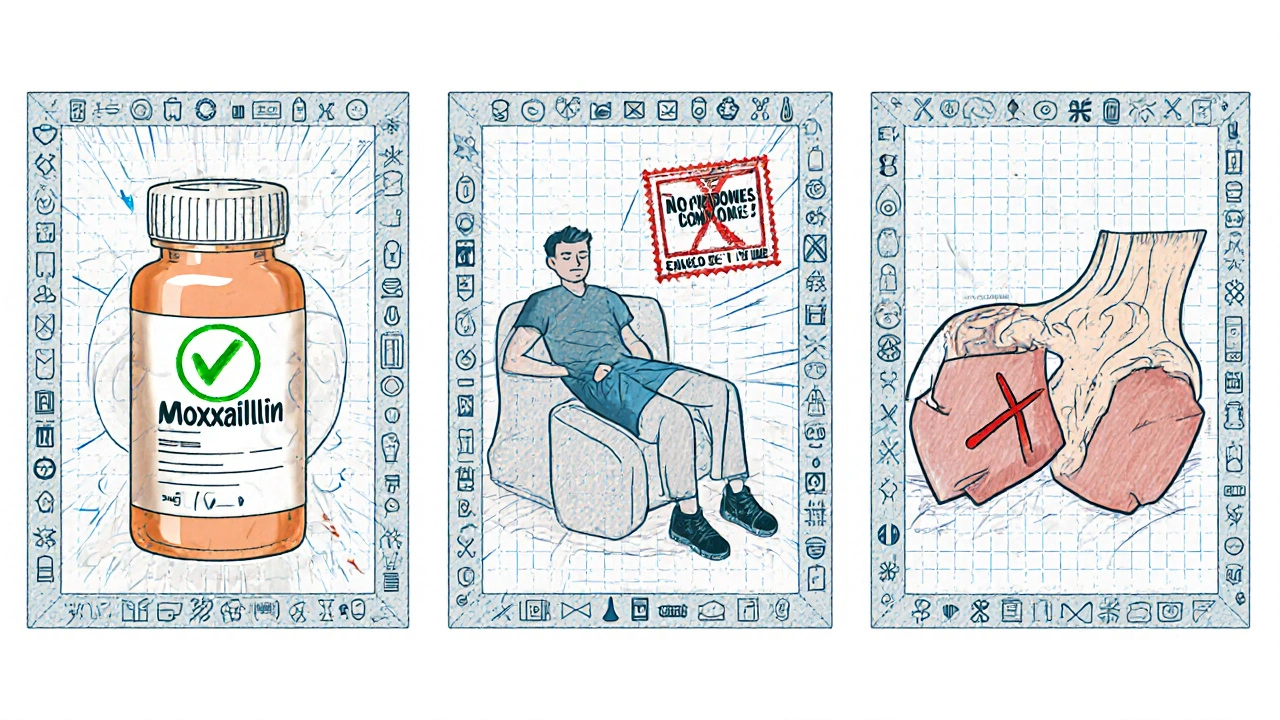
For uncomplicated UTIs, amoxicillin or nitrofurantoin work just as well - with far fewer risks. For sinus infections, amoxicillin-clavulanate is the first-line choice. For bronchitis, most cases are viral and don’t need antibiotics at all.
Prescribing rates have dropped since 2016. In the U.S., fluoroquinolone use for UTIs fell from 17% to just 5% by 2022. But many doctors still default to them. Why? Lack of awareness. Outdated training. Or pressure from patients who want a quick fix.
Don’t let that be you. If your doctor says, ‘This is the strongest antibiotic,’ ask: ‘Is there a safer option?’ If they say no, get a second opinion.
What to Do If You’ve Already Taken One
If you’ve taken ciprofloxacin, levofloxacin, or moxifloxacin - even months ago - watch for these signs:
- Sudden, sharp pain in your heel, shoulder, or wrist
- Swelling or warmth around a tendon
- Tingling, burning, or numbness in your hands or feet
- Weakness when walking or gripping things
If you notice any of these, stop all physical activity. Don’t ice it. Don’t stretch. Don’t wait. See a doctor who knows about fluoroquinolone toxicity. Bring this information. Many primary care providers still don’t recognize it.
And if you’re currently taking one - stop immediately and call your doctor. Don’t finish the course unless you have a life-threatening infection like anthrax or complicated pneumonia. For everything else, the risks outweigh the benefits.
Alternatives That Are Safer
You don’t need fluoroquinolones for most infections. Here are proven, safer alternatives:
| Infection | Recommended Alternative | Risk of Tendon/Nerve Damage |
|---|---|---|
| Uncomplicated UTI | Nitrofurantoin, Amoxicillin-clavulanate | Very low |
| Acute sinusitis | Amoxicillin-clavulanate | Very low |
| Acute bronchitis | Usually no antibiotic needed | None |
| Complicated UTI | Ceftriaxone, Piperacillin-tazobactam | Low |
| Hospital-acquired pneumonia | Meropenem, Vancomycin | Low |
These drugs may require more monitoring or IV use, but they don’t wreck your tendons or nerves. Ask your doctor to prescribe one of these instead.
What’s Being Done - And What’s Not
Regulators are catching up. The EMA banned fluoroquinolones for mild infections in 2019. The UK’s MHRA says they’re only for ‘no other options.’ The FDA now requires warning labels. But enforcement? That’s up to doctors.
Pharmaceutical companies still market these drugs aggressively. Patient advocacy groups like the Fluoroquinolone Effects Research Foundation have over 8,500 reports of long-term disability. Reddit communities like r/floxing have 14,000 members sharing stories of life-altering damage.
Yet, most medical schools still don’t teach fluoroquinolone toxicity in depth. A 2022 study found only 43% of primary care doctors could correctly identify fluoroquinolone-induced tendinopathy in a case scenario. That’s not just a gap - it’s a public health failure.
How to Protect Yourself
Here’s your action plan:
- Never take a fluoroquinolone for a cold, sinus infection, or simple UTI
- Ask: ‘Is there a safer antibiotic?’ before accepting any prescription
- If you’re over 60, on steroids, or have kidney issues - say no
- If you feel tendon pain or nerve tingling after taking one - stop the drug and get help immediately
- Report side effects to the FDA MedWatch program - your report helps others
These drugs saved lives in the 1980s. But medicine evolves. What was once considered safe is now known to be dangerous for most people. You have the right to know. You have the right to choose. Don’t let outdated practices put your mobility and health at risk.
Can fluoroquinolone tendon damage be reversed?
In some cases, yes - if caught early. Stopping the drug immediately and resting the tendon can prevent rupture. But if the tendon has torn or nerve damage has set in, full recovery is rare. Up to 10% of patients experience permanent disability, including chronic pain, reduced mobility, and difficulty walking. Early intervention improves outcomes, but there’s no guaranteed cure.
How long after taking fluoroquinolones can side effects appear?
Tendon pain can start as early as 2 days after starting the drug - or as late as 150 days after finishing it. Nerve damage often begins within the first month, but in 22% of cases, symptoms don’t show up until months later. This delayed onset is why many patients and doctors miss the connection.
Are all fluoroquinolones equally dangerous?
No, but all carry risk. Ciprofloxacin is the most commonly linked to tendon rupture, followed by levofloxacin and moxifloxacin. But the FDA’s black-box warning applies to all drugs in this class. No fluoroquinolone is safe for routine use. The differences in risk are minor compared to the shared danger of tendon and nerve damage.
Can I take fluoroquinolones if I have no other options?
Yes - but only for serious, life-threatening infections like anthrax, complicated pneumonia, or multidrug-resistant tuberculosis. For these rare cases, the benefits may outweigh the risks. But for common infections like UTIs, sinusitis, or bronchitis, there are always safer alternatives. Never accept a fluoroquinolone unless your doctor can prove no other treatment will work.
What should I do if I think I have fluoroquinolone toxicity?
Stop taking the drug immediately. Avoid all strenuous activity. Do not take corticosteroids - they increase rupture risk. See a doctor who understands fluoroquinolone toxicity. Bring printed information or research. If your doctor dismisses you, seek a second opinion from an infectious disease specialist or rheumatologist. Document your symptoms and timeline - this helps with diagnosis and future reporting.
Final Thoughts
Fluoroquinolones are not the miracle drugs they were once thought to be. They’re high-risk tools reserved for extreme cases. For the vast majority of infections, safer, equally effective options exist. The real danger isn’t the bacteria - it’s the assumption that stronger means better.
If you’ve been prescribed one of these antibiotics, ask questions. Push back. Demand alternatives. Your tendons and nerves can’t afford to wait for the system to catch up. Your body remembers - and so should your doctor.


All Comments
Danny Nicholls November 23, 2025
Bro i took cipro for a UTI last year and thought my heel pain was just from running... turns out both tendons were inflamed. Docs said "it's just aging" 😒 I didn't know until i found r/floxing. Now i can't even walk my dog without wincing. If you're on these, STOP. Your body will thank you later. 🙏😭
manish chaturvedi November 24, 2025
It is indeed alarming that such potent antibiotics are still prescribed casually. In India, too, pharmacists hand out fluoroquinolones like candy. Patients demand "strong" medicine, and doctors, under pressure, comply. We must educate the public and train physicians better. This is not merely a medical issue-it is a cultural one.
Nikhil Chaurasia November 25, 2025
My uncle took levofloxacin for a "bad cough"... three weeks later, he couldn't stand up. Both Achilles tendons snapped. He was 68. No sports. No history. Just a prescription. Now he walks with a cane. I told my doctor last month: "If you're going to give me that, I'm walking out." I didn't get the script. I got respect.
Holly Schumacher November 25, 2025
Let me be crystal clear: if your doctor prescribes a fluoroquinolone for a sinus infection, they are either grossly negligent or dangerously uninformed. The FDA warning is not a suggestion-it’s a legal mandate. And yet, 5% of UTIs in the U.S. still get cipro. That’s not incompetence. That’s malpractice. I’ve documented 14 cases in my medical journal. None of the patients recovered fully. None.
Michael Fitzpatrick November 26, 2025
I know this sounds dramatic but I’ve been living with nerve pain for over a year now after a simple UTI. It started as tingling in my toes, then burning, then just… nothing. No feeling. I used to hike every weekend. Now I can barely stand for more than 10 minutes. I’ve seen 7 doctors. Only one knew what I was talking about. The rest told me to try yoga. I wish I’d known this info before I took the pill. I really do. I just wish more people would talk about this. It’s not just me. It’s thousands.
Shawn Daughhetee November 27, 2025
took cipro for a bladder thing last year... woke up one day and my right heel felt like it was on fire. thought it was plantar fasciitis. kept going to the gym. ended up in PT for 6 months. still feel it sometimes. if you feel weird pain after these drugs... just stop. rest. don't be a hero. your tendons aren't made for that
Miruna Alexandru November 29, 2025
It's fascinating how pharmaceutical capitalism thrives on ignorance. Fluoroquinolones are profitable, patent-protected, and easy to prescribe. Meanwhile, the long-term cost-disability, chronic pain, lost productivity-is externalized onto the patient. We're not talking about side effects. We're talking about engineered vulnerability. The system doesn't fail-it functions exactly as designed. And you? You're the cost center.
Justin Daniel November 30, 2025
lol i remember when my doc said "this is the strongest antibiotic" like it was a badge of honor. i asked "what’s the weakest one that’ll work?" and he looked at me like i asked for a unicorn. i got amoxicillin. i’m fine. he’s still prescribing cipro to 70-year-olds with UTIs. 🤡
steve o'connor December 1, 2025
My sister got moxifloxacin for a chest infection. Two weeks later, her hands went numb. Doctor said "it's anxiety." She cried for three days. Then she found this post. We went to a neurologist who actually listened. She’s improving slowly. But if we hadn’t found this info, she’d still be told she’s imagining it. Thank you for writing this.
ann smith December 2, 2025
Thank you for sharing this. I’m so glad someone is speaking up. I’m a nurse and I’ve seen too many patients come in with tendon pain and no idea why. I always ask now: "Have you taken any antibiotics recently?" It’s changed my practice. Please keep sharing your stories. We need more awareness. 💪❤️
Julie Pulvino December 3, 2025
Just wanted to say I’m 34, healthy, no steroids, no diabetes-still took cipro for a UTI. 45 days later, my shoulder seized up. MRI showed tendon degeneration. No rupture, but I can’t lift my arm above my head. I’m in physical therapy. I’m lucky. I know people who are worse. Please, if you’re reading this… don’t be like me. Ask for alternatives. Your body isn’t a lab rat.