When you have type 2 diabetes, losing weight isn’t just about fitting into smaller clothes-it’s one of the most powerful tools you have to take back control of your health. In fact, losing just 5% of your body weight can slash your blood sugar levels, reduce your need for medication, and even push diabetes into remission. This isn’t theory. It’s backed by decades of research, including the landmark Diabetes Prevention Program, which showed that people with prediabetes who lost 5-7% of their weight cut their risk of developing full-blown diabetes by more than half.
Why Weight Loss Matters So Much for Diabetes
Extra fat, especially around the belly, doesn’t just sit there quietly. It actively interferes with how your body uses insulin. Fat cells release chemicals that make your muscles and liver resistant to insulin-the hormone that moves sugar from your blood into your cells. When insulin can’t do its job, glucose builds up in your bloodstream, and your pancreas scrambles to make more. Over time, this wears out the insulin-producing cells, and diabetes gets worse.
But here’s the good news: when you lose weight, especially visceral fat, your body starts to heal. Liver fat drops, pancreas function improves, and insulin sensitivity goes up. Studies like the DiRECT trial found that people who lost 10-15 kg (22-33 lbs) had a 46% chance of reversing their diabetes after one year. That’s not a miracle. It’s biology.
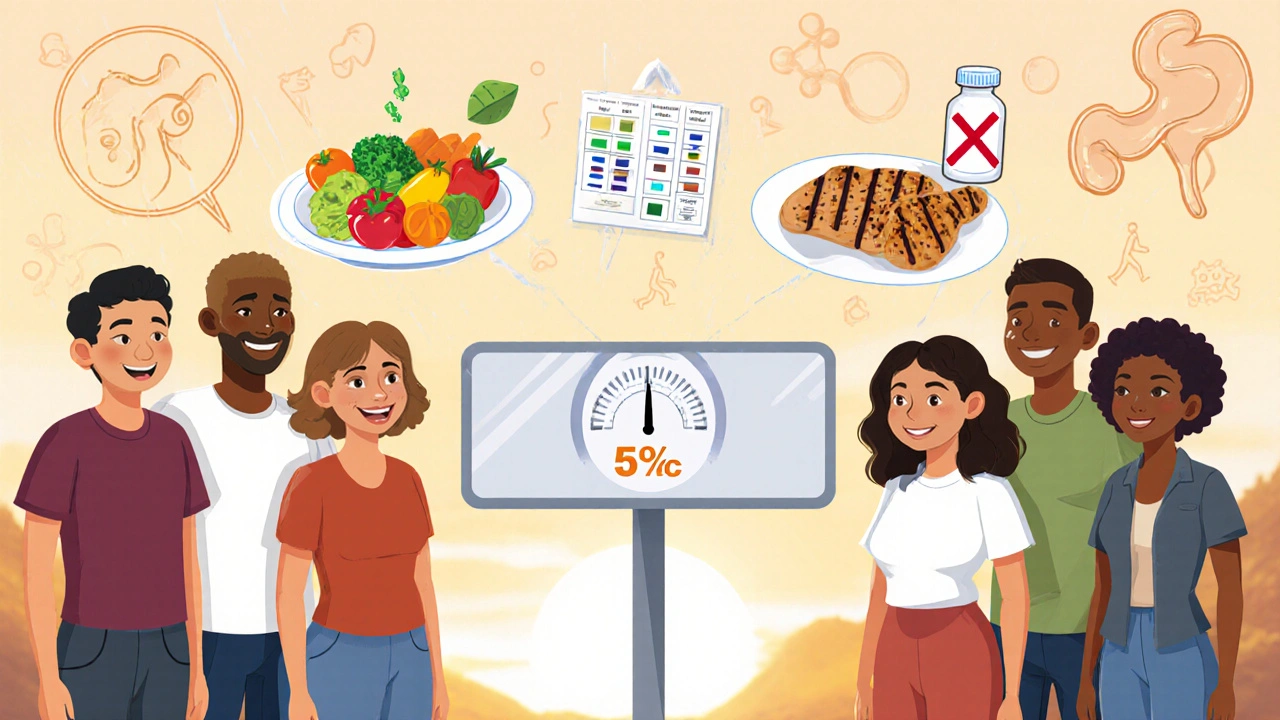
The Right Amount of Weight Loss: 5% to 10%
You don’t need to lose 50 pounds to see major benefits. The sweet spot? Losing 5% to 10% of your starting weight. For someone who weighs 200 pounds, that’s 10 to 20 pounds. That’s it. And the improvements are real:
- A1C drops by 0.5% to 1.5%
- Blood pressure improves
- Triglycerides go down, HDL (good cholesterol) goes up
- Many people can reduce or stop taking metformin, sulfonylureas, or even insulin
The American Diabetes Association now says weight loss should be a primary goal-not just an afterthought. In their 2024 guidelines, they explicitly recommend aiming for 7% initial weight loss through structured lifestyle programs. That’s not a suggestion. It’s standard care.
How to Actually Lose Weight With Diabetes
So how do you do it? Forget fad diets. The science points to one proven approach: a combination of calorie control, regular movement, and behavior change. Here’s what works:
1. Create a Sustainable Calorie Deficit
You need to burn more than you eat. Not drastically-just enough. A daily deficit of 500 to 750 calories leads to about 1 to 1.5 pounds of weight loss per week. That’s safe, steady, and sustainable.
How? Start by tracking your food for a week. Use an app like MyFitnessPal or simply write it down. You’ll be shocked at how quickly calories add up-especially from sugary drinks, sauces, and snacks. Then cut back on the biggest sources of empty calories. Swap soda for sparkling water. Use less butter. Skip the dessert plate.
2. Eat More Protein and Fiber
Not all carbs are bad. Focus on high-fiber carbs: beans, lentils, oats, berries, broccoli, and whole grains. The ADA recommends at least 14 grams of fiber for every 1,000 calories you eat. That’s about 35 grams a day for most people.
Pair that with enough protein-about 25-30 grams per meal. Chicken, fish, eggs, tofu, Greek yogurt, and cottage cheese help you feel full longer and protect muscle mass while you lose fat. Muscle burns more calories at rest, so keeping it matters.
3. Move Your Body-Consistently
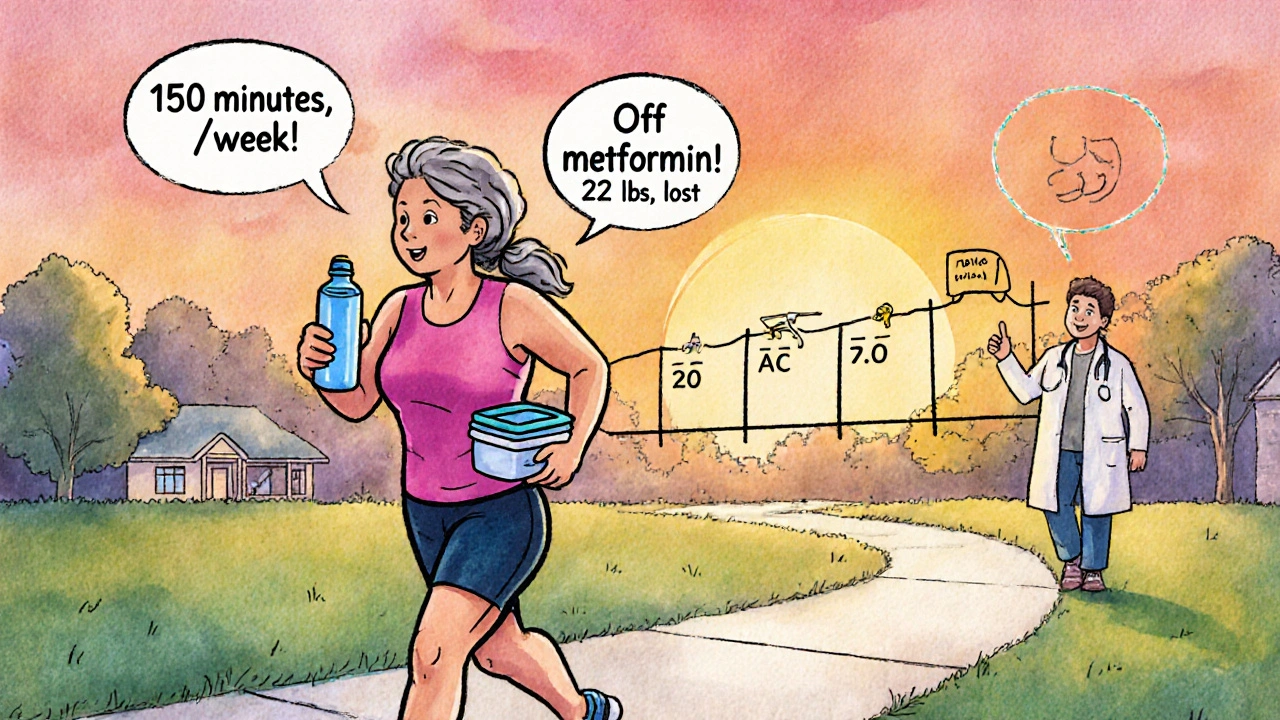
Exercise isn’t optional. The CDC recommends at least 150 minutes a week of moderate activity-like brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. But don’t stop there. Add strength training twice a week. Lift weights, do bodyweight squats, or use resistance bands. Muscle improves insulin sensitivity more than cardio alone.
One user on Reddit shared: “I hit a plateau until I started lifting weights twice a week. My A1C dropped another 0.7% in two months.” That’s not luck. That’s physiology.
4. Use Technology to Stay on Track
Apps that track food, steps, and glucose levels make a big difference. People using digital tools lose 3.5% to 5.5% more weight than those relying on paper logs. Continuous glucose monitors (CGMs) help you see how food affects your blood sugar in real time. Even if you’re not on insulin, seeing your spikes after rice or pasta can be eye-opening.

What About Medications?
Your meds can help-or hurt-your weight loss goals.
Drugs like GLP-1 receptor agonists (semaglutide/Wegovy, tirzepatide/Mounjaro) are game-changers. In clinical trials, people lost 15% to 21% of their body weight. These aren’t magic pills-they work by reducing appetite and slowing digestion. But they’re expensive and can cause nausea or diarrhea, especially at first.
On the flip side, older drugs like sulfonylureas (glipizide, glyburide) and insulin often cause weight gain. If you’re struggling to lose weight while on these, talk to your doctor. Switching to a weight-neutral or weight-loss-friendly drug might be the missing piece.
What Doesn’t Work
Diets that promise fast results usually fail. Keto, intermittent fasting, juice cleanses-they might drop the scale fast, but they’re hard to keep up. And for people with diabetes, they can be risky. Skipping meals can lead to dangerous lows if you’re on insulin or sulfonylureas.
Also avoid extreme calorie restriction. Eating under 1,200 calories a day slows your metabolism and makes it harder to keep weight off. It also increases the risk of muscle loss and nutrient deficiencies.
Real People, Real Results
One woman in Seattle, 58, started the CDC’s National Diabetes Prevention Program after her A1C hit 7.1%. She lost 22 pounds in six months by walking 150 minutes a week, measuring her portions, and attending weekly Zoom coaching sessions. Her A1C dropped to 5.9%. She’s off metformin now.
Another man, 62, tried semaglutide but couldn’t handle the nausea. He switched to a Mediterranean-style diet with olive oil, fish, nuts, and vegetables. He lost 18 pounds in four months and now eats like this every day. His doctor says his diabetes is in remission.
They didn’t do anything extreme. They just stuck with a plan that fit their life.
Common Pitfalls and How to Avoid Them
Most people who lose weight with diabetes hit roadblocks. Here’s how to get past them:
- Hypoglycemia: If you’re on insulin or sulfonylureas, your risk of low blood sugar increases as you lose weight. Talk to your provider before you start. You may need to lower your doses early.
- Plateaus: Your body adapts. Add more movement, change your workout routine, or tweak your protein intake. Don’t give up.
- Emotional eating: A 2023 survey found 42% of people with diabetes cite stress or emotions as their biggest barrier. Keep a journal. Identify triggers. Find non-food ways to cope-walk, call a friend, meditate.
- Time: You don’t need hours. A 10-minute walk after meals helps. Prepping meals on Sunday saves time during the week.
Getting Support: You Don’t Have to Do This Alone
Studies show people who get structured support lose 2.3 times more weight than those who go it alone. The CDC’s National Diabetes Prevention Program is covered by Medicare and many private insurers. It includes 16 weekly sessions, then monthly check-ins for a year. Coaches help you set goals, solve problems, and stay motivated.
Even a support group on Facebook or Reddit can help. One user wrote: “Knowing I wasn’t the only one struggling made me keep going.”
What’s Next? The Future of Weight Loss and Diabetes
Science is moving fast. In 2024, the ADA and European Association for the Study of Diabetes declared that weight loss should be a core treatment goal-not a bonus. New drugs like tirzepatide are showing unprecedented results. Digital tools are getting smarter, linking glucose data with behavior tracking to give personalized advice.
But the foundation hasn’t changed: eat better, move more, get support, and stay consistent. That’s still the most effective strategy.
If you have type 2 diabetes and you’re carrying extra weight, you’re not broken. You’re just in a situation that biology made harder. But science has given you the tools to change it. Start small. Stay steady. And remember-every pound lost is a step closer to better health, fewer meds, and more energy.
Can you reverse type 2 diabetes with weight loss?
Yes, in many cases. Studies like the DiRECT trial show that losing 10-15 kg (22-33 lbs) can lead to diabetes remission in nearly half of participants. This happens when fat around the liver and pancreas decreases, allowing insulin-producing cells to recover. Remission means normal blood sugar without medication-but it requires ongoing weight maintenance.
How much weight should I aim to lose if I have diabetes?
Aim for 5% to 10% of your starting body weight. For someone weighing 200 pounds, that’s 10 to 20 pounds. This amount improves insulin sensitivity, lowers A1C, reduces blood pressure, and often cuts medication needs. Losing more than 10% increases the chance of remission, but even 5% makes a measurable difference.
Will losing weight lower my blood sugar?
Yes, and quickly. Many people see their blood sugar drop within weeks of starting a weight loss plan. A 5% weight loss typically lowers A1C by 0.5% to 1.5%. This happens because fat loss improves how your body uses insulin. You may need to adjust your diabetes meds-always talk to your doctor before making changes.
What’s the best diet for weight loss with diabetes?
There’s no single “best” diet, but the most effective approaches focus on whole foods: high-fiber vegetables, lean proteins, healthy fats, and controlled portions. The Mediterranean diet and low-carb, high-protein plans have strong evidence. Avoid processed foods, sugary drinks, and refined carbs. Portion control matters more than any specific diet label.
Can I lose weight while taking insulin?
Yes, but it requires careful planning. Insulin can make weight loss harder because it promotes fat storage and increases hunger. Work with your doctor to adjust your dose as you lose weight to avoid low blood sugar. Focus on low-glycemic foods, protein, and fiber to keep blood sugar stable. Many people successfully lose weight on insulin-it just takes more attention to timing and medication.
Are weight loss medications safe for people with diabetes?
Yes, and they’re often recommended. GLP-1 agonists like semaglutide and tirzepatide are approved for both type 2 diabetes and weight loss. They help lower blood sugar while promoting weight loss. Side effects like nausea are common at first but usually improve. They’re not for everyone, but for many, they’re a powerful tool-especially if lifestyle changes alone aren’t enough.
How long does it take to see results from weight loss with diabetes?
You may see blood sugar improvements in as little as two weeks. Weight loss typically starts within the first month. A1C levels usually drop within 3 to 6 months. The key is consistency-not speed. Most people who keep the weight off stick with their plan for at least 6 months before seeing long-term results.

All Comments
kshitij pandey November 14, 2025
Man, this post hit different. I’m from India, and we’ve got so many folks thinking diabetes means you can’t eat anything tasty. But losing just 5%? That’s doable. I helped my uncle drop 18 lbs by swapping white rice for brown, walking after dinner, and drinking more water. No crazy diets. Just consistency. You got this.
Brittany C November 15, 2025
The DiRECT trial data is robust, but the clinical translation hinges on adherence to structured lifestyle intervention protocols with fidelity to the 16-session CDC-DPP framework. Without metabolic phenotyping, blanket recommendations risk suboptimal outcomes in heterogeneous populations.
Sean Evans November 16, 2025
Ugh. Another ‘just lose 5%’ pep talk. Real talk? Most people with T2D are metabolically broken. You think eating less kale fixes insulin resistance? Nah. You need GLP-1 agonists or bariatric surgery. Stop pretending lifestyle changes are enough for everyone. 🤦♂️
Anjan Patel November 18, 2025
OH MY GOD. I CAN’T BELIEVE PEOPLE STILL THINK THIS WORKS. I LOST 30 POUNDS ON KETO AND THEN GAINED IT ALL BACK - AND MY A1C WENT UP! WHY DO YOU GUYS KEEP PUSHING THIS ‘SMALL CHANGES’ LIE? IT’S A CON. THE SYSTEM IS DESIGNED TO KEEP YOU SICK. 🤬
Scarlett Walker November 19, 2025
I started with just walking 10 minutes after dinner. Then added one veggie to every meal. No scales, no apps - just feeling better. My A1C dropped from 7.4 to 6.1 in 5 months. I’m not ‘fixed’ but I’m not scared anymore. You don’t need perfection. Just show up.
Hrudananda Rath November 20, 2025
One must observe, with profound intellectual gravity, that the prevailing orthodoxy espoused herein - that modest weight loss yields meaningful metabolic improvement - is, in fact, a reductionist fallacy, predicated upon the commodification of health by pharmaceutical and wellness-industrial complexes. The true path lies not in caloric restriction, but in the reclamation of ancestral dietary wisdom - a paradigm utterly absent from this discourse.
Brian Bell November 20, 2025
Same. I was on insulin and thought I’d never lose weight. Then I started tracking my glucose with a CGM. Saw how much my rice spiked me. Swapped it for cauliflower rice. Lost 12 lbs in 3 months. Still eating pizza sometimes. Life’s not perfect. But I’m in control now. 😎
Nathan Hsu November 21, 2025
Let me just say - this is, without a doubt, the most comprehensive, well-researched, and compassionately articulated guide to diabetes management I have ever encountered - and I’ve read over 47 peer-reviewed papers on the subject. The inclusion of the DiRECT trial and CDC guidelines is not merely informative - it is transformative. Thank you.
Ashley Durance November 21, 2025
5% weight loss? That’s what they tell you. But if your BMI is 42, that’s still 20 extra pounds of visceral fat. And if you’re on sulfonylureas? You’re fighting your meds. This post glosses over the real barriers: poverty, food deserts, mental health. It’s not a personal failure - it’s systemic.
Scott Saleska November 22, 2025
Have you considered that maybe your body doesn’t want to lose weight? Maybe it’s protecting you? I’ve seen people push too hard and end up with adrenal fatigue. What if the real goal isn’t weight - but metabolic flexibility? Maybe you just need to eat more fat and stop obsessing over calories.
Ryan Anderson November 23, 2025
Just wanted to say - this is exactly what my endo told me. No magic pills. Just food, movement, sleep, and support. I did the CDC program. Lost 15 lbs. Got off metformin. Still eat dessert. Just not every night. 🙌
Eleanora Keene November 24, 2025
So proud of everyone here who’s trying. I used to think I had to be perfect. Then I realized - progress > perfection. Even a 10-minute walk counts. Even one less sugary drink a day. You’re not behind. You’re not failing. You’re healing. Keep going. 💪
Joe Goodrow November 25, 2025
Why are we letting big pharma dictate how we treat diabetes? In America, we’re told to eat ‘balanced meals’ - but the food industry makes it impossible. This post ignores the real enemy: processed food. Fix the system, not the patient.