Every year, about 1 in 1,000 contact lens wearers in the U.S. ends up with an eye infection serious enough to require medical care. Many of these cases aren’t accidents-they’re preventable. The problem isn’t the lenses themselves. It’s how they’re handled. Poor hygiene, wrong solutions, and ignoring wear time rules turn a simple vision correction tool into a risk to your sight. You don’t need to be an expert to keep your eyes safe. You just need to know the basics-and stick to them.
Hand Hygiene: The First Line of Defense
Your hands touch everything: doorknobs, phones, money, your face. Then you reach for your contact lenses. That’s how bacteria, fungi, and even parasites get to your eyes. The CDC and the National Institutes of Health agree: washing your hands before handling lenses is the single most important step in preventing infection. Don’t just rinse. Don’t use hand sanitizer. Use plain soap and water. Scrub for 20 to 30 seconds-long enough to sing "Happy Birthday" twice. Pay attention to your fingertips, under your nails, and between your fingers. Dry with a clean, lint-free towel. Paper towels work better than cloth ones because they don’t shed fibers that can stick to your lenses. Why not hand sanitizer? Alcohol and fragrances in sanitizers can damage soft lenses and irritate your eyes. Even a tiny residue left on your fingers can cause burning or redness. A 2018 NIH study found that only 53% to 77% of users wash their hands properly. That means nearly half of all lens wearers are skipping this critical step.Choosing the Right Solution
Not all contact lens solutions are the same. What works for one brand or type of lens might ruin another. Your eye care professional recommends a solution for a reason. Don’t switch brands just because it’s on sale or your friend swears by it. Saline solution and rewetting drops? They’re for comfort only. They do NOT clean or disinfect. Using them to store your lenses is like putting a dirty dish in the dishwasher without detergent-nothing gets sanitized. Hydrogen peroxide systems are popular because they kill more microbes than multipurpose solutions. But they’re tricky. If you don’t let the solution neutralize completely (usually 4 to 6 hours), you risk a chemical burn to your cornea. Always follow the timer on the case. Never rinse lenses with hydrogen peroxide before putting them in. Let the case do its job. And never, ever use tap water. Not to rinse your lenses. Not to clean your case. Not even to rinse your eyes after swimming. Tap water contains Acanthamoeba-a microscopic organism that burrows into the cornea and causes a rare but devastating infection called Acanthamoeba keratitis. Treatment can cost up to $7,500 per case. Some people lose vision permanently.Case Care: The Hidden Danger
Your lens case is a breeding ground. Even if you clean your lenses perfectly, a dirty case can recontaminate them. The American Optometric Association says replace your case every three months. But here’s the truth: if you’re not cleaning it right, even a new case won’t help. After each use, empty the case. Rinse it with fresh disinfecting solution-not water. Don’t just wipe it out. Swirl the solution around for 5 seconds. Then leave it open, upside down, on a clean tissue. Air drying prevents moisture buildup, which bacteria love. Don’t cap it tightly after rinsing. That traps moisture and turns your case into a microbe hotel. Some people think they can get away with cleaning the case once a week. That’s not enough. Daily rinsing and weekly replacement of solution aren’t optional-they’re medical necessities. One Reddit user shared: "Since I started replacing my case every month and never topping off solution, I’ve had zero infections in two years." That’s not luck. That’s discipline.
Wear Time: When to Take Them Out
Your lenses have a schedule. Daily, biweekly, monthly. Stick to it. Don’t stretch them. Don’t "just wear them one more day." Even if they feel fine, the material breaks down. Protein and lipid buildup builds up. Your eyes get oxygen-starved. That’s when ulcers and infections start. Sleeping in lenses? Only if your eye doctor specifically prescribed extended-wear lenses. Even then, it’s risky. About 40% to 50% of users admit to sleeping in lenses not meant for overnight use. That’s a major red flag. Your cornea needs oxygen. When you close your eyes, airflow drops. Lenses block what little oxygen gets through. Combine that with bacteria from your pillow or eyelashes, and you’ve created the perfect storm. Water exposure? Remove lenses before showering, swimming, or even splashing your face. The FDA says swimming with contacts increases infection risk by 10 to 15 times. If you accidentally get water on your lenses, take them out immediately. Clean and disinfect them. If they’re daily disposables, toss them. No exceptions.What About Daily Disposables?
Daily disposables are the safest option. No case. No solution. No cleaning. You put them in the morning, throw them out at night. No chance of contamination from storage. They’ve gone from 45% of the U.S. market in 2018 to 65% today-and for good reason. They’re not cheaper upfront. But they save you money long-term. No solution bottles. No cases. Fewer doctor visits for infections. One study found users of daily disposables had 70% fewer eye infections than those using monthly lenses. If you’ve been using monthly lenses and want to switch, talk to your eye care provider. They can help you transition without wasting lenses. Many insurance plans now cover daily disposables because they reduce overall healthcare costs.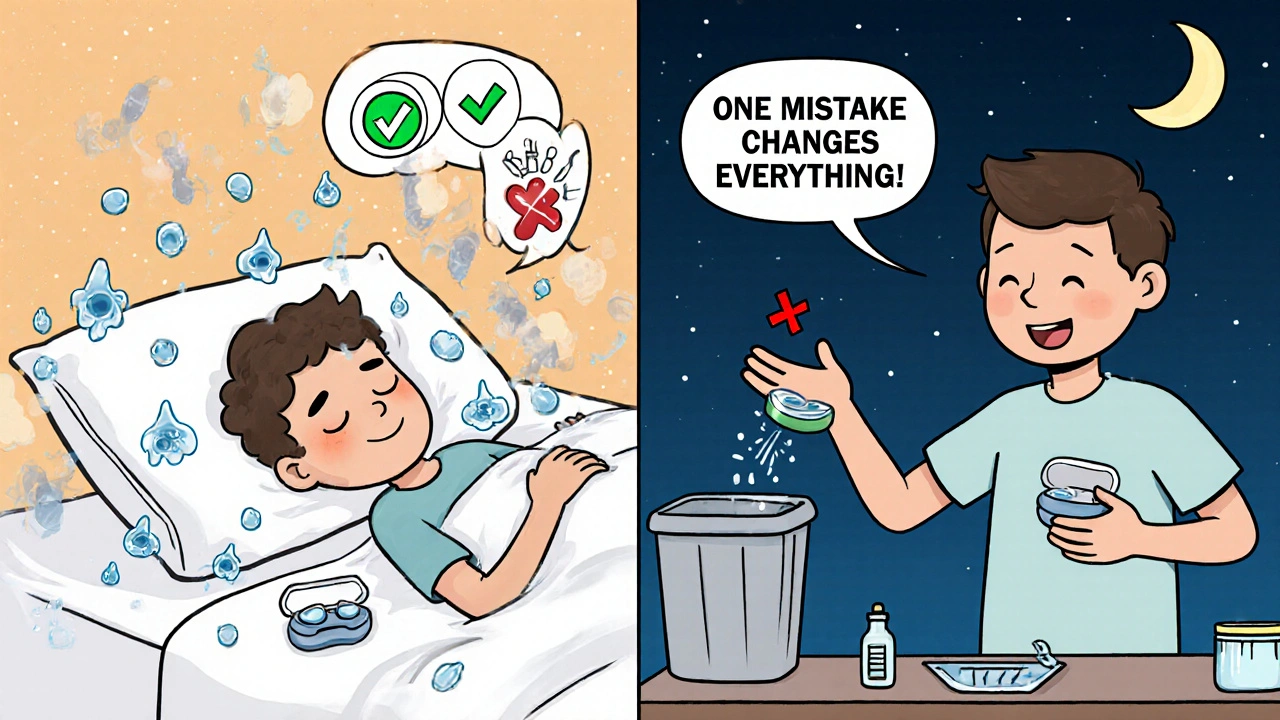
Who’s at Highest Risk?
The FDA reports that 85% of contact lens complications happen in people aged 18 to 24. Why? Young adults are more likely to skip hygiene steps, sleep in lenses, and ignore warnings. They think it won’t happen to them. Or they’re in a hurry. Or they don’t have a parent or guardian reminding them. But age isn’t the only factor. People with dry eyes, allergies, or those who work in dusty or smoky environments are more vulnerable. If your eyes feel gritty, red, or sore after wearing lenses-even for a few hours-don’t push through it. See your eye doctor. Early signs of infection include: pain, blurred vision, light sensitivity, and excessive tearing.What to Do If Something Feels Off
If your eye feels painful, unusually red, or you suddenly see spots or halos around lights, take your lenses out. Don’t put them back in. Don’t wait to see if it gets better. Call your eye care provider immediately. Don’t go to the ER unless it’s an emergency. Most eye infections can be treated quickly if caught early. Don’t use over-the-counter eye drops for redness unless your doctor says so. Some drops contain vasoconstrictors that mask symptoms but make the real problem worse. Keep a log: when you wore lenses, when you cleaned them, when you replaced your case. If you get an infection, this record helps your doctor figure out what went wrong.Final Reality Check
Contact lenses are amazing. They give freedom from glasses. They help with sports, appearance, confidence. But they’re medical devices. Not fashion accessories. Not toys. Not something you can treat casually. The science is clear. Follow the rules, and your risk of infection is extremely low. Ignore them, and you’re gambling with your vision. One mistake-one night of sleeping in lenses, one rinse with tap water, one old case-can change your life forever. You don’t need to be perfect. But you do need to be consistent. Wash your hands. Use the right solution. Replace your case. Take them out on time. That’s it. Do those five things, and you’re doing better than most.Can I reuse daily disposable contact lenses?
No. Daily disposables are designed to be worn once and thrown away. Reusing them increases the risk of infection, corneal damage, and discomfort. Even if they look clean, the material breaks down after 24 hours. Never rinse and reuse daily lenses.
Is it safe to swim with contact lenses?
No. Swimming with contacts-whether in pools, lakes, or oceans-exposes your eyes to harmful microbes like Acanthamoeba. The FDA says this increases infection risk by 10 to 15 times. If you must swim, wear waterproof goggles. If you accidentally get water on your lenses, remove and disinfect them immediately-or discard them if they’re daily disposables.
Can I use water to clean my contact lens case?
Never. Tap water contains bacteria, fungi, and parasites that can survive in your lens case and infect your eyes. Always rinse your case with fresh disinfecting solution, then air-dry it upside down. Even distilled water isn’t safe for this purpose.
Why do my eyes feel dry even when I follow all the rules?
Dryness can happen even with perfect hygiene. It’s often caused by screen use, air conditioning, or underlying conditions like meibomian gland dysfunction. Try switching to daily disposables-they retain moisture better. Use preservative-free rewetting drops. If dryness persists, talk to your eye doctor about specialty lenses or treatments like IPL therapy.
How often should I replace my contact lens case?
Replace your case every three months at minimum. But many eye care professionals recommend replacing it every month, especially if you’ve had an eye infection before. A dirty case is one of the top reasons for recurring infections, even when lenses and solutions are handled correctly.
Are hydrogen peroxide solutions better than multipurpose solutions?
Hydrogen peroxide systems kill more microbes than multipurpose solutions, making them better for people prone to infections or with sensitive eyes. But they require more steps: you must let the solution neutralize fully (4-6 hours) and never rinse lenses with it before inserting. If you’re not careful, you can burn your cornea. Multipurpose solutions are simpler but may not be as effective against certain pathogens.


All Comments
Shawn Sakura November 22, 2025
man i just started wearing contacts last year and this post saved my vision tbh. i used to rinse my case with tap water because i was lazy. now i use hydrogen peroxide and let it sit overnight. no more red eyes. thanks for the reminder that this isn't a fashion accessory.
Paula Jane Butterfield November 24, 2025
as a mom of two teens who wear contacts, i can't stress this enough: replace the case every month. i used to think three months was fine. then my daughter got a nasty infection. now we mark the date on the calendar. also, daily disposables are worth every penny. no more cleaning drama. 🙏
Simone Wood November 24, 2025
you people are being way too dramatic. i've worn contacts for 12 years, never washed my hands before touching them, reused my case for 18 months, slept in them every weekend, and rinsed them with bottled water. i'm fine. your fearmongering is why people don't trust medical advice anymore. also, tap water is fine. it's not like we're drinking it.
Debanjan Banerjee November 26, 2025
the data is clear: 85% of complications occur in 18–24-year-olds because of behavioral negligence, not biological vulnerability. this is not a hygiene issue-it’s a cultural issue. social media normalizes cutting corners. influencers post selfies with ‘week-old lenses’ and call it ‘edgy.’ the solution isn’t more warnings-it’s systemic education. schools should mandate contact lens safety modules in health class. period.
Steve Harris November 27, 2025
just want to say i switched to daily disposables last year after reading this. no case. no solution. no stress. i used to be the guy who’d ‘just wear them one more day.’ now i toss them at midnight. it’s a small habit, but it changed my life. my eyes haven’t felt this good in years. seriously, if you’re on the fence-do it. your future self will thank you.
Michael Marrale November 28, 2025
wait… have you ever wondered if the contact lens companies are hiding something? they push daily disposables because they make more money. but what if the real danger is the preservatives in the solutions? i read a forum where someone said the FDA banned a chemical in 2019 that’s still in 80% of multipurpose solutions. they’re profiting off our eye infections. i’m not paranoid. i’m informed. check the ingredient list. you’ll see.
David vaughan November 30, 2025
just wanted to add: i use rewetting drops religiously, but only the preservative-free kind. also, i keep a tiny notebook in my bathroom: date, lens type, case replacement, solution used. it’s overkill? maybe. but last month, when my eye got red, i pulled out my log and realized i’d topped off the solution two days in a row. fixed it. no infection. i’m weird. but my eyes are fine.
David Cusack December 1, 2025
the notion that 'washing hands is the single most important step' is statistically reductive. while hand hygiene is necessary, it is neither sufficient nor uniquely causal in the prevention of microbial keratitis. the literature consistently identifies biofilm formation in lens cases as the primary vector-yet this post disproportionately emphasizes handwashing, thereby misallocating public health attention. one might argue this is a deliberate simplification for mass consumption. it is not helpful. it is misleading.
Elaina Cronin December 2, 2025
I have read this entire post three times. I have printed it. I have laminated it. I have given copies to my sister, my cousin, and my yoga instructor who wears contacts. This is not an opinion. This is a public health imperative. If you are reading this and you reuse your case or sleep in your lenses-you are not being cool. You are being reckless. And if you think it won’t happen to you, you are the reason your friend lost vision. Please. Stop.
Willie Doherty December 2, 2025
the 70% reduction in infections with daily disposables is misleading. the cohort using daily disposables is inherently more health-conscious. selection bias is not accounted for. the study fails to control for socioeconomic status, education level, or baseline ocular health. correlation ≠ causation. this post is a textbook example of anecdotal evidence masquerading as evidence-based medicine. the real solution? better lens materials-not behavioral policing.
Darragh McNulty December 4, 2025
just wanna say: i used to be the guy who washed his hands under the sink for 3 seconds and called it good. then i got a corneal ulcer. 3 weeks of antibiotics. lost 2 weeks of work. paid $4k. now i sing happy birthday twice. i air-dry my case. i toss my dailies. i use hydrogen peroxide. and i never, ever swim with them. 🙏❤️👁️🗨️ if you're reading this and you're not doing these things-do it. your eyes are worth it.