Why Smoking Can Make Your Clozapine Stop Working
If you’re taking clozapine for treatment-resistant schizophrenia, and you smoke cigarettes, your medication might not be working as well as you think. It’s not because you’re not taking it - it’s because smoking is changing how your body processes the drug. This isn’t a minor detail. It’s one of the most dangerous and overlooked drug-environment interactions in psychiatry.
Clozapine is powerful. It’s the last-line treatment for people who haven’t responded to other antipsychotics. But it’s also tricky. It has a narrow window where it works - too little and symptoms come back; too much and you risk seizures, heart problems, or even life-threatening drops in white blood cells. And tobacco smoke? It throws this balance completely off.
How Smoking Knocks Clozapine Out of Your System
The key player here is an enzyme in your liver called CYP1A2. This enzyme breaks down clozapine so your body can get rid of it. Normally, CYP1A2 handles about 60-70% of clozapine metabolism. But when you smoke, things change.
Tobacco smoke contains chemicals called polycyclic aromatic hydrocarbons. These don’t just harm your lungs - they send a signal to your liver: “Make more CYP1A2.” Within 48 to 72 hours of starting to smoke, your liver starts producing way more of this enzyme. The result? Clozapine gets broken down twice as fast. Studies show that smokers typically have 30-50% lower clozapine levels in their blood than non-smokers.
That means if you’re taking 300 mg a day and you start smoking, your body is clearing the drug so quickly that you’re essentially taking 150 mg. Your symptoms might return - irritability, hallucinations, paranoia - and your doctor might think the dose isn’t strong enough. So they increase it. But if you quit smoking later, that same dose becomes toxic.
What Happens When You Quit Smoking
This is where things get dangerous. Many patients don’t realize that quitting smoking doesn’t just help their lungs - it can trigger a medical emergency.
When you stop smoking, your CYP1A2 enzyme levels don’t drop overnight. They take 1 to 2 weeks to return to normal. During that time, your body is still clearing clozapine slowly, but your dose hasn’t changed. So the drug builds up. Levels that were perfectly safe while smoking can suddenly climb into the toxic range.
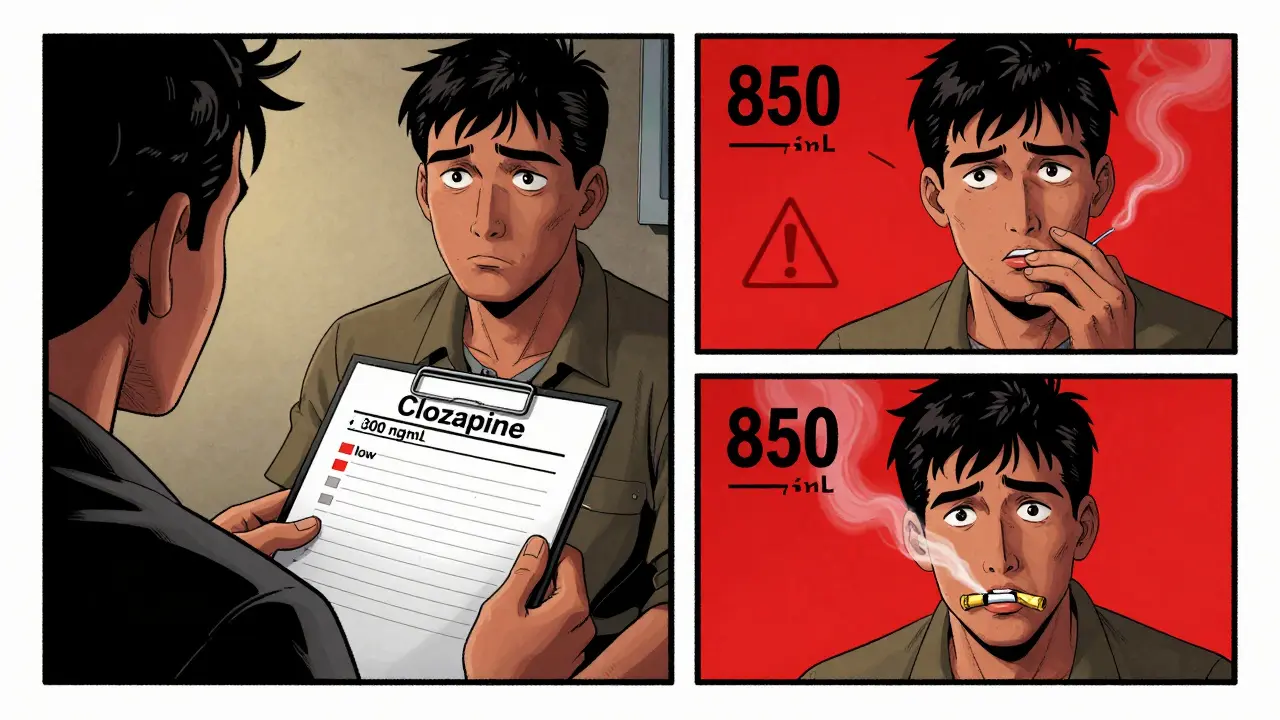
Real cases show this clearly. One woman was taking 400 mg of clozapine daily while smoking. When she quit, her levels jumped to 850 ng/mL - well above the safe upper limit of 500 ng/mL. She became extremely drowsy, her heart raced, and she nearly needed intensive care. Her dose had to be cut in half.
Another man, a heavy smoker, was on 450 mg daily but still had levels too low to control his symptoms. After increasing his dose to 650 mg, his levels stabilized. When he tried to quit smoking, his doctor had to drop his dose to 300 mg within weeks to avoid toxicity.
Why Clozapine Is Different From Other Antipsychotics
Not all antipsychotics react this way. Olanzapine is also metabolized by CYP1A2, but less so - only 30-40% of its clearance depends on it. Risperidone? Mostly handled by CYP2D6. Quetiapine? CYP3A4. None of these are as tightly tied to CYP1A2 as clozapine.
That’s why the effect is so much stronger with clozapine. A 20-30% drop in levels might be manageable with other drugs. With clozapine, a 30-50% drop can mean the difference between symptom control and hospitalization. And because clozapine’s therapeutic range is so narrow - between 350 and 500 ng/mL - even small changes matter a lot.
Genetics Make It Even More Complicated
Not everyone who smokes responds the same way. Some people have a genetic variant called CYP1A2 *1F/*1F. These individuals start with normal enzyme levels, but their bodies respond more strongly to smoking. They see bigger drops in clozapine levels than others who smoke the same amount.
On the flip side, some people naturally have low CYP1A2 activity - even without smoking. Their bodies clear clozapine slowly, so they need lower doses. If they start smoking, the increase in enzyme activity might not be enough to push them into the therapeutic range. Others might need massive dose increases just to stay stable.
This is why blanket advice like “smokers need 50% more” doesn’t always work. One person might need 20% more. Another might need 80% more. That’s why testing blood levels isn’t optional - it’s essential.
What Doctors Should Do - And What They Often Don’t
According to the American Psychiatric Association, clozapine levels should be checked within 4-7 days after any dose change. That includes after someone starts or stops smoking. But in practice? Many clinicians don’t check.
A 2023 survey of psychiatrists found that 68% ask about smoking at every visit. But only 82% adjust doses based on that info. And only 1 in 4 routinely check blood levels after a smoking change.
That’s a problem. A 2021 study found that unmanaged smoking-related clozapine changes led to 22% more hospitalizations. Each avoidable hospital stay costs about $14,500. That’s not just a health risk - it’s a financial one too.
Some hospitals now use electronic alerts in their systems. If a patient on clozapine has a smoking status change, the EHR flags it. One study showed this cut adverse events by 37%. Simple tech. Big impact.

What You Can Do If You’re on Clozapine
- If you smoke, tell your doctor - and don’t stop without talking to them.
- Ask for a blood test to check your clozapine level. Don’t wait for symptoms.
- If you’re trying to quit smoking, work with your doctor to plan a dose reduction before you quit. Don’t wait until you feel sick.
- If you start smoking again after quitting, let your doctor know immediately. You’ll likely need a dose increase.
- Don’t assume vaping is safe. E-cigarettes still contain chemicals that induce CYP1A2 - just slightly less than traditional cigarettes.
Many patients feel frustrated. They say, “I’ve tried to quit smoking three times, and each time I end up hospitalized.” That’s not their fault. It’s a system failure. This interaction is predictable, measurable, and manageable - if you know to look for it.
What’s Next for Clozapine and Smoking
Researchers are working on solutions. A new sustained-release clozapine formulation, currently in clinical trials, is designed to reduce the swings caused by CYP1A2 induction. Early results show 40% less variation in blood levels among smokers.
Genetic testing for CYP1A2 variants is also becoming more common. In 2018, only 15% of U.S. academic centers tested for it. By 2023, that number jumped to 47%. It’s still not routine - but it’s growing.
Meanwhile, the FDA and European regulators both classify this interaction as clinically significant. They require it to be addressed in prescribing guidelines. The message is clear: if you’re on clozapine, smoking status isn’t a lifestyle question - it’s a medical one.
Bottom Line: This Isn’t About Willpower - It’s About Chemistry
Smoking doesn’t make you “non-compliant.” It changes your biology. Clozapine levels aren’t just about how much you take - they’re about how fast your body breaks it down. And tobacco smoke speeds that up dramatically.
Managing this interaction isn’t about telling patients to quit smoking (though that’s ideal). It’s about adjusting the dose to match their reality. Whether they smoke, quit, or vape - their treatment plan must change with them.
For the 60-70% of clozapine patients who smoke - which is most of them - this is the difference between staying out of the hospital and ending up in one. It’s not complicated. It’s just overlooked. And that’s dangerous.


All Comments
Alexandra Enns January 25, 2026
This is such a blatant example of how psychiatry ignores the real world. Smoking isn't some bad habit you punish people for-it's a biological variable that changes drug kinetics. If your doctor doesn't check levels after a smoking change, they're not a doctor, they're a lottery ticket seller. I've seen patients crash because their 'dose adjustment' was based on vibes, not blood tests. Stop treating patients like broken code and start treating them like humans with livers.
Marie-Pier D. January 26, 2026
I'm so glad someone finally put this out there 💛
My cousin was on clozapine for 8 years and smoked through it all. When she quit for her kid, she went from functional to barely able to stand up. No one warned her. No one checked her levels. She ended up in ER with a heart rate of 140 and was terrified she was dying. Turned out it was just the meds building up. Now she's on a lower dose and doing amazing. Please, if you're on clozapine and you smoke-or quit-tell your provider. And if they don't listen, find someone who will.
Shanta Blank January 28, 2026
Oh sweet jesus this is the most predictable trainwreck in psychopharmacology and yet everyone still acts like it’s a surprise. Like, wow, chemicals in smoke = liver goes full turbo mode = drug gets vaporized. Who could’ve guessed? The fact that this isn’t standard protocol is criminal. And don’t even get me started on the ‘vaping is safer’ crowd-those little vape pens are basically CYP1A2 espresso shots. You think you’re being cool? You’re just doing pharmacology roulette with your brain.
Chloe Hadland January 28, 2026
i just want to say thank you for writing this. i’ve been on clozapine for 5 years and i smoke. i didn’t realize my dose was basically half of what it should’ve been. my doc never mentioned it. i thought i was just ‘not responding well’
got my levels checked last month and boom-280 ng/mL. they bumped me up and now i’m actually sleeping at night. it’s not about quitting. it’s about being seen. thank you for seeing us.
Amelia Williams January 29, 2026
This is the kind of info that changes lives. Seriously. I’ve met so many people who think they’re failing because their meds ‘don’t work’-but it’s not them, it’s their liver. And when they quit smoking? Panic mode. No one tells them. No one prepares them. It’s like handing someone a loaded gun and saying ‘good luck’
Why isn’t this in every patient handout? Why isn’t it a mandatory checklist? We’re talking about hospitalizations, heart issues, seizures. This isn’t ‘niche’-it’s systemic. Let’s fix it.
Viola Li January 30, 2026
So let me get this straight-people are allowed to smoke, but if they do, their entire medication regimen has to be adjusted? That’s just enabling. If you’re too weak to quit smoking, why are you even on clozapine? This isn’t a ‘lifestyle accommodation’-it’s a failure of personal responsibility. Stop medicalizing addiction and start demanding accountability.
Himanshu Singh January 31, 2026
I’ve seen this play out in my clinic in Delhi. One man, 42, smoked 2 packs a day. His clozapine level was 210 ng/mL. We doubled his dose-he stabilized. Then he quit cold turkey for his daughter’s wedding. Two weeks later, he was lethargic, slurring words. His level? 720 ng/mL. We cut his dose by 40%. He cried and said, ‘I thought I was getting better.’
It’s not about blame. It’s about timing. Your body doesn’t care about your intentions. It only cares about enzymes. Be gentle with yourself and your science.
Jamie Hooper February 2, 2026
i just read this and my jaw hit the floor. i’ve been on clozapine since 2020 and i smoke. my doc says ‘keep doing what ur doing’ but i’ve been feeling off for months. guess what? i’m gonna get my levels checked next week. no more guessing games. also… vaping is NOT safe. those flavor pods? they’re sneaky little enzyme boosters. just saying.
Marlon Mentolaroc February 3, 2026
Funny how people treat smoking like a moral issue instead of a metabolic one. You wouldn’t blame a diabetic for eating sugar if their insulin was miscalibrated. But with clozapine? ‘Just quit.’ No. Just adjust the dose. The science is crystal clear. If your provider doesn’t get this, find a new one. This isn’t complicated. It’s just inconvenient for the system.