Chloramphenicol Appropriateness Checker
Chloramphenicol Appropriateness Checker
Determine if chloramphenicol is appropriate for your specific situation based on infection type, patient age, allergies, and location.
Recommendation
Chloramphenicol isn’t used often these days - and for good reason. Once a go-to for serious infections, it’s now reserved for rare cases where other antibiotics fail. Why? Because it can cause life-threatening side effects, even at low doses. But in some parts of the world, or in specific infections like bacterial meningitis or typhoid fever, it still shows up. So if you’re wondering whether chloramphenicol is still worth considering, or if there’s a safer, just-as-effective alternative, you’re not alone.
What chloramphenicol actually does
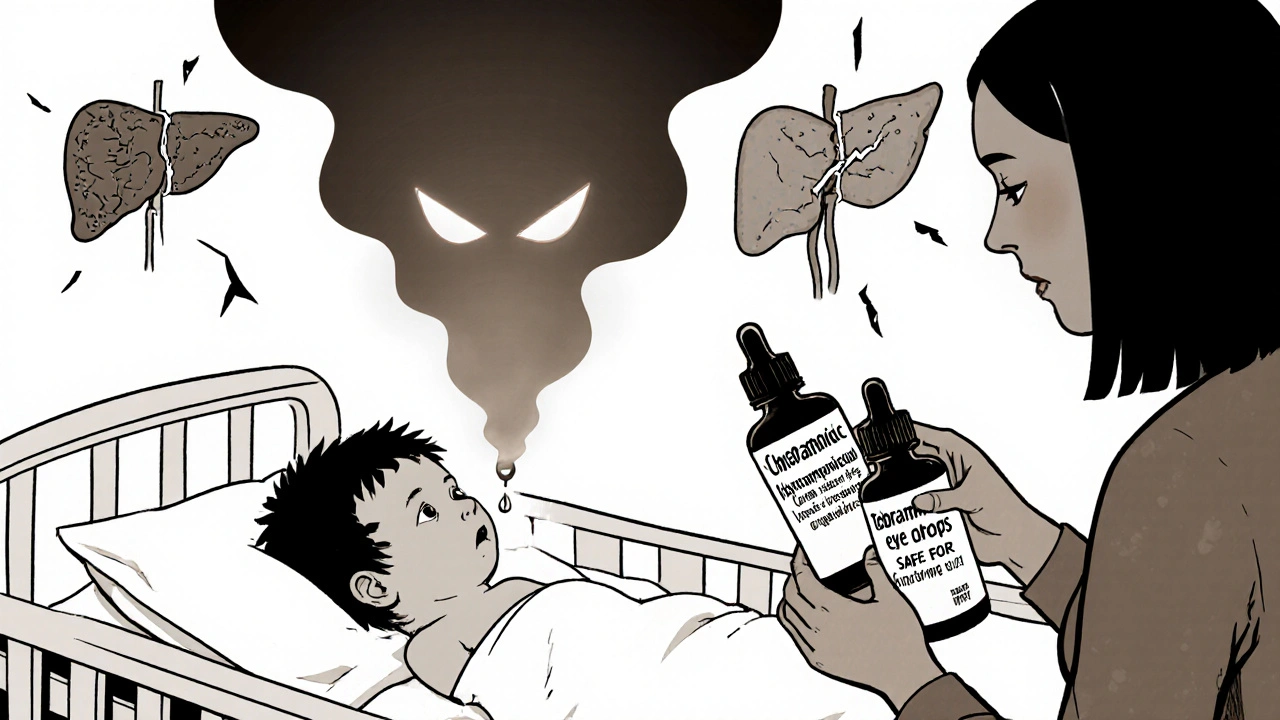
Chloramphenicol is a broad-spectrum antibiotic. That means it works against a wide range of bacteria - both Gram-positive and Gram-negative. It stops bacteria from making proteins, which they need to survive and multiply. Back in the 1940s, it was a miracle drug. It worked where penicillin didn’t. It was cheap. It came in pills, eye drops, and injections. But over time, doctors noticed something alarming: some patients developed a rare but deadly condition called aplastic anemia, where the bone marrow stops making blood cells. Even worse, it can cause gray baby syndrome in newborns, a fatal buildup of the drug due to immature liver function.
Today, the FDA and WHO only recommend chloramphenicol when no other options are available. It’s not a first-line treatment anywhere in the U.S. or Europe. In developing countries, it’s still used because it’s inexpensive and accessible. But even there, guidelines are tightening.
Why alternatives are preferred
Modern medicine has dozens of safer, equally effective antibiotics. The key difference? They don’t carry the same risk of permanent, irreversible damage. When you choose an alternative, you’re not giving up effectiveness - you’re trading risk for safety.
For example, if you’re treating a urinary tract infection, amoxicillin or ciprofloxacin work just as well without the chance of bone marrow failure. For eye infections, tobramycin or ciprofloxacin eye drops are standard. For meningitis, ceftriaxone or vancomycin are preferred. Even for typhoid fever, azithromycin or ceftriaxone are now first-line in most guidelines.
Chloramphenicol’s biggest advantage - low cost - is becoming less relevant. Generic versions of safer antibiotics are now cheaper than ever. A 10-day course of azithromycin for typhoid costs less than $10 in many places. Ceftriaxone injections, while more expensive upfront, prevent hospitalization and long-term complications that chloramphenicol can cause.
Top alternatives and when to use them
Not all antibiotics are the same. Choosing the right one depends on the infection, the patient’s age, allergies, and local resistance patterns. Here’s what’s used today instead of chloramphenicol:
- Amoxicillin - First choice for ear infections, sinusitis, and mild pneumonia. Safe for kids and pregnant women. Doesn’t affect bone marrow.
- Ciprofloxacin - Used for urinary tract infections, typhoid, and some gastrointestinal infections. Works fast. Avoid in children under 18 unless absolutely necessary due to tendon risks.
- Ceftriaxone - The gold standard for bacterial meningitis and severe infections. Given as an injection. No risk of aplastic anemia.
- Azithromycin - Great for typhoid fever, respiratory infections, and chlamydia. Single-dose options make it easy to use. Fewer side effects than chloramphenicol.
- Tobramycin (eye drops) - Standard for bacterial conjunctivitis. No systemic absorption, so no risk of bone marrow suppression.
- Metronidazole - Used for anaerobic infections like abdominal abscesses or bacterial vaginosis. Works differently than chloramphenicol but just as effectively in those cases.
Each of these has been studied in large clinical trials. In 2023, a Cochrane review of typhoid fever treatments found azithromycin had a 97% cure rate with zero cases of aplastic anemia. Chloramphenicol’s cure rate was similar - but the risk of death from side effects was 1 in 24,000 patients. That’s not a trade-off most doctors will accept.
When chloramphenicol might still be used
There are a few exceptions where chloramphenicol remains in play. One is in resource-limited settings where ceftriaxone or azithromycin aren’t available. Another is for patients with severe allergies to all other antibiotics - though this is extremely rare.
It’s also still used in some eye infections, especially in developing countries, because chloramphenicol eye drops are cheap and stable at room temperature. But even here, alternatives like tobramycin or fluoroquinolone drops are preferred in hospitals and clinics with better resources.
Another niche use: Rocky Mountain spotted fever in patients allergic to doxycycline. In those cases, chloramphenicol can be a backup. But again, it’s not the first choice - it’s the last resort.
The hidden dangers you won’t hear about
Most people know chloramphenicol can cause serious side effects. But few realize how unpredictable they are. Aplastic anemia doesn’t show up after a week of use. It can appear months later, even after you’ve stopped taking it. There’s no way to test for it beforehand. No blood test can predict who’s at risk. That’s why doctors avoid it entirely when possible.
Gray baby syndrome affects newborns because their livers can’t break down the drug. Even a single dose can be dangerous. That’s why chloramphenicol is banned for use in infants under 2 weeks old in most developed countries.
And here’s something else: chloramphenicol can interact with other drugs. It can make blood thinners like warfarin stronger, increasing bleeding risk. It can interfere with seizure medications. It can reduce the effectiveness of vaccines. These interactions are rarely discussed in patient leaflets - but they’re real.
What patients should ask their doctor
If your doctor suggests chloramphenicol, here are three questions to ask:
- Is this the only option? Are there FDA-approved alternatives?
- What’s the risk of serious side effects compared to other antibiotics?
- Can you explain why you’re choosing this over something safer?
Most of the time, the answer will be: yes, there are better choices. If the answer is no - and you’re in the U.S. or Europe - get a second opinion. There’s almost always a safer alternative.
For parents: never use leftover chloramphenicol eye drops on your child without a prescription. Even a single drop can be risky in infants. Always check expiration dates. If it’s older than 30 days after opening, throw it out.
Final takeaway: Safety beats cost
Chloramphenicol isn’t evil. It saved lives in the 1940s. But medicine has moved on. Today, we have antibiotics that work just as well - without the risk of killing you in the long run. Choosing chloramphenicol isn’t a cost-saving move. It’s a gamble with your bone marrow, your liver, or your child’s life.
When you’re facing an infection, ask for the safest option - not the oldest one. Your body will thank you.
Is chloramphenicol still used today?
Yes, but only in very limited cases. It’s rarely used in the U.S. and Europe due to serious side effects. It may still be used in developing countries for typhoid fever or meningitis when better antibiotics aren’t available. Eye drops are the most common form today, but even those are being replaced by safer options like tobramycin.
What are the most dangerous side effects of chloramphenicol?
The two most dangerous side effects are aplastic anemia - a rare but often fatal condition where the bone marrow stops producing blood cells - and gray baby syndrome, which occurs in newborns and can be fatal due to the body’s inability to process the drug. Both can happen even after short-term use, and there’s no way to predict who’s at risk.
Can chloramphenicol be replaced with amoxicillin?
In most cases, yes. Amoxicillin is safer and just as effective for common infections like ear infections, sinusitis, and pneumonia. It doesn’t affect bone marrow and is safe for children and pregnant women. Chloramphenicol is only considered when amoxicillin and other antibiotics have failed or aren’t suitable due to allergies.
Why is chloramphenicol cheaper than other antibiotics?
Chloramphenicol is cheap because it’s an old, off-patent drug with simple manufacturing. But its low cost doesn’t make it a better value. Safer alternatives like azithromycin and ceftriaxone are now available as generics, often costing the same or less. When you factor in hospitalization costs from side effects, chloramphenicol ends up being far more expensive overall.
Is chloramphenicol safe for children?
No, it’s not considered safe for children under 2 weeks old due to the risk of gray baby syndrome. Even in older children, it’s avoided unless there are no other options. For ear infections, strep throat, or pneumonia, amoxicillin, azithromycin, or cefdinir are standard and much safer.


All Comments
Brittney Lopez October 31, 2025
Really appreciate this breakdown - I’m a nurse and I’ve seen firsthand how scary it is when someone gets prescribed chloramphenicol out of habit instead of choice. So glad we’ve moved past it in most cases. Safety first, always.
Jens Petersen October 31, 2025
Oh please. Let’s not pretend modern medicine is some saintly oracle. Chloramphenicol was banned not because it was dangerous - but because Big Pharma pushed cheaper, patentable alternatives. The real tragedy? Patients in the Global South are being told their lives are less worth protecting. This isn’t progress - it’s pharmaceutical colonialism.
Keerthi Kumar November 2, 2025
Thank you for this - truly. In India, we still see chloramphenicol in rural clinics, often as the only option. But I’ve watched families lose children to gray baby syndrome… and then lose their savings paying for ICU care that should’ve been avoided. We need better access to generics - not just more lectures about ‘safety.’ Compassion without access is just guilt.
Dade Hughston November 4, 2025
so like i was reading this and i thought wow this is so detailed but then i realized like... wait why are we even talking about this drug like its still a thing i mean like my cousin took it in 2018 and her bone marrow just... stopped like one day she was fine then she was in the hospital for months and now she needs transfusions every two weeks and i just... i dont know what to say
Jim Peddle November 4, 2025
Let’s not romanticize the past. The fact that chloramphenicol is still available in some regions isn’t a testament to its utility - it’s evidence of systemic failure. Regulatory capture, corruption, and lack of infrastructure make alternatives inaccessible. This isn’t about cost. It’s about power.
S Love November 4, 2025
This is exactly the kind of clear, evidence-based breakdown we need more of. For parents, especially - please, don’t let nostalgia or convenience override science. Amoxicillin isn’t just ‘safer’ - it’s better. Period.
Pritesh Mehta November 5, 2025
Western medicine always thinks it knows best. Chloramphenicol has been used in our villages for 70 years. People survive. Children recover. You speak of ‘risk’ like it’s a luxury we can afford. We don’t have ceftriaxone refrigerators. We don’t have specialists. We have mothers who walk 15 kilometers for a bottle of medicine. Don’t lecture us about safety when you’ve never had to choose between a child’s life and a hospital bill.
Billy Tiger November 6, 2025
Chloramphenicol is a relic. And so are the people who defend it. If you're still using it you're either a quack or a criminal. End of story. No exceptions. No ‘but in my country’ excuses. Medicine isn't a free-for-all
Katie Ring November 6, 2025
It’s not just about the drug - it’s about who gets to decide what’s ‘safe.’ Who gets to say that a mother in Bihar doesn’t deserve the same standard of care as a mother in Boston? The answer? The same people who profit from the system that denies it.
Adarsha Foundation November 8, 2025
I understand the frustration on both sides - the need for affordable care, and the need for safety. But perhaps the real solution isn’t choosing between chloramphenicol and ceftriaxone - it’s building systems that make ceftriaxone affordable everywhere. Let’s not pit lives against each other. Let’s lift the ladder for all.
Alex Sherman November 9, 2025
Of course the FDA banned it. They’re just protecting Big Pharma’s bottom line. The real danger? The fact that you’re being told what to believe. Question authority. Question ‘evidence.’ The truth is buried under layers of corporate PR.
Oliver Myers November 10, 2025
This was so helpful - thank you so much for writing it. I’m a med student, and I’ve only ever heard chloramphenicol mentioned in textbooks as ‘the scary one.’ Reading this made me feel more confident about explaining why we avoid it to patients. It’s not about fear - it’s about responsibility.
John Concepcion November 11, 2025
LMAO you people act like chloramphenicol is some ancient poison. It’s just a drug. People used to take aspirin for everything and no one cried about it. You’re all just scared of anything that doesn’t come with a 10-page insert. Chill out. It’s not magic. It’s not evil. It’s just medicine.