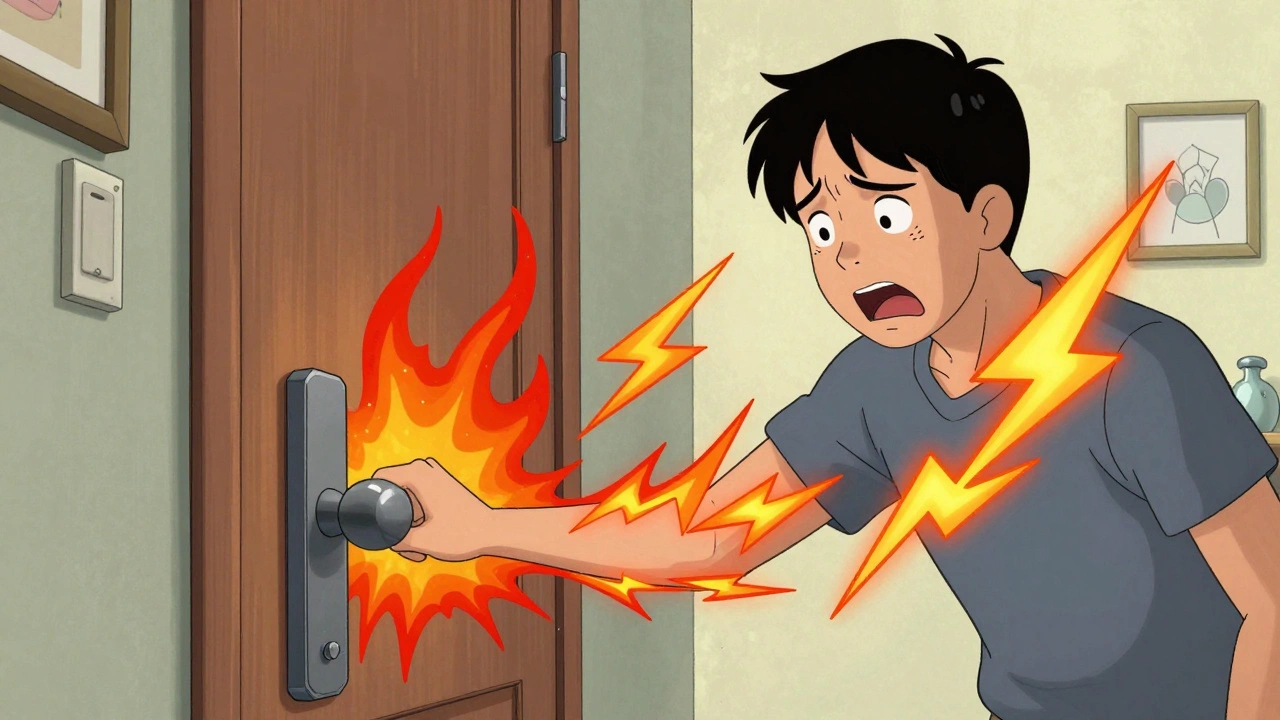
Imagine touching a doorknob and feeling like your skin is burning. Or getting a hug that feels like needles. You didn’t get hurt. There’s no swelling, no injury, no infection. But the pain is real - intense, constant, and spreading. This isn’t weakness. It’s not "all in your head." It’s central sensitization.
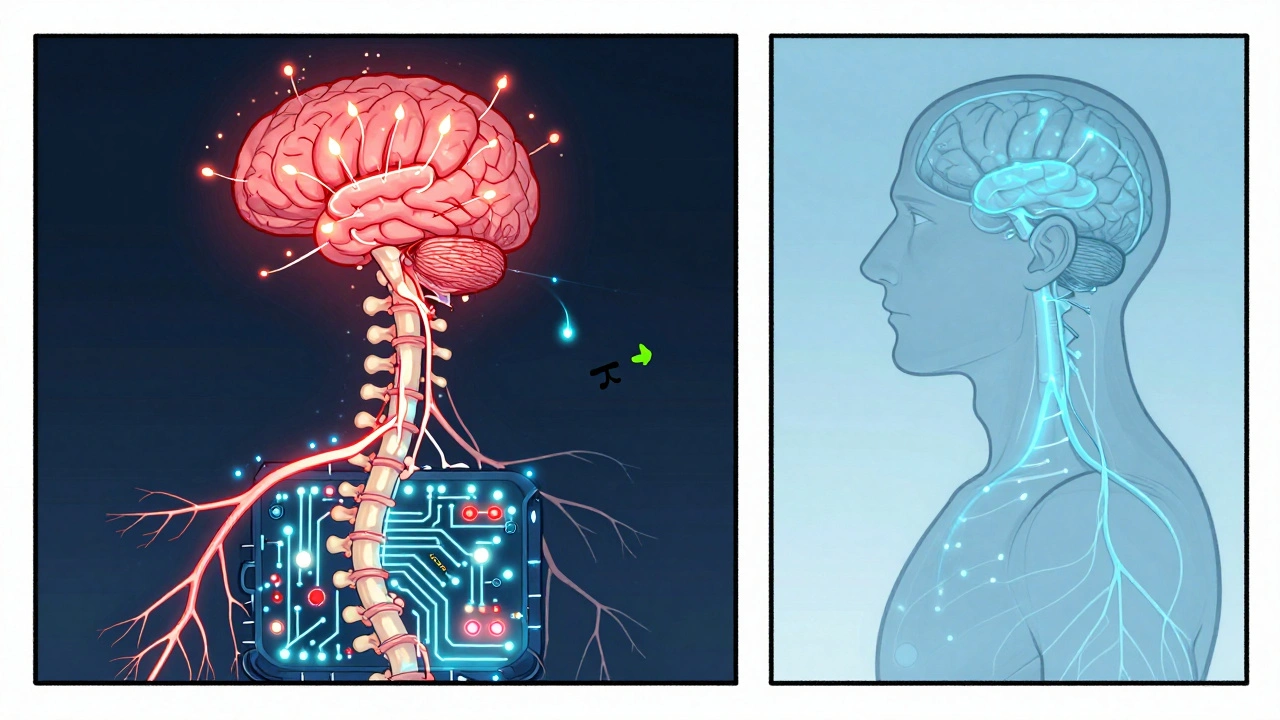
What Exactly Is Central Sensitization?
Central sensitization is when your nervous system gets stuck on high volume. Normally, your brain and spinal cord filter pain signals like a security system: only serious threats get through. But in central sensitization, that system malfunctions. Even quiet signals - a light breeze, clothes brushing your skin, a routine step - get turned up to 11.This isn’t about damaged nerves in your foot or back. It’s about the brain and spinal cord rewiring themselves. The term was first described by neuroscientist Clifford J. Woolf in 1983, who called it a "spinal cord wind-up phenomenon." Think of it like a radio that keeps turning up the volume even after you stop pressing the button. The original signal (like a sprained ankle) may have healed weeks ago, but your nervous system still thinks it’s under attack.
Studies show this happens in 2-4% of the global population. It’s the main driver behind conditions like fibromyalgia (affecting 2-8% of adults), chronic low back pain that won’t quit, and some types of post-surgical pain. In fibromyalgia, up to 90% of patients show clear signs of central sensitization. That’s not coincidence - it’s biology.
How Your Body Turns Up the Pain
Your nervous system has two main pathways for pain: the "go" signal (ascending) and the "stop" signal (descending). In central sensitization, the go signal gets stronger, and the stop signal gets weaker.Here’s what’s happening inside:
- Neurons in your spinal cord become hyper-excitable - they fire more easily and for longer.
- Chemical messengers like substance P and glutamate increase by 25-30%, overstimulating pain circuits.
- Your brain’s pain-processing areas light up 20-35% more on fMRI scans, even with mild stimuli.
- Your body’s natural painkillers (endorphins and opioids) don’t work as well - mu-opioid receptor binding drops by 15-25%.
- Immune cells in your nervous system get activated, spiking inflammation-related proteins by 30-50%.
It’s not just one change. It’s a cascade. Every time you feel pain - even if it’s small - your nervous system learns to respond more strongly. Over time, it becomes the new normal. This is why pain can spread from your lower back to your neck, your shoulder, even your scalp - even if none of those areas were ever injured.
How Do You Know You Have It?
Doctors don’t use blood tests or X-rays to diagnose central sensitization. Instead, they look for patterns:- Widespread pain - affecting 3-4 body regions or more. Most patients report pain in at least 5 areas.
- Allodynia - pain from things that shouldn’t hurt. Light touch, a tag on your shirt, a shower spray. About 85-90% of people with this condition experience this.
- Hyperalgesia - pain that’s way worse than it should be. A pinprick that feels like a stab.
- Temporal summation - repeated mild stimuli (like tapping your arm) build up into intense pain. This "wind-up" effect is seen in 70% of cases.
- Non-anatomical pain - pain that doesn’t follow nerve pathways. It jumps around. It doesn’t match MRI findings.
Specialized tests help confirm it:
- Quantitative Sensory Testing (QST) - measures how much pressure or heat it takes to cause pain. People with central sensitization feel pain at 20-30% lower thresholds than normal.
- Conditioned Pain Modulation - tests your body’s ability to shut off pain. In central sensitization, this system works 40-50% worse.
- Pain drawings - patients draw where they hurt. In central sensitization, drawings are messy, scattered, and often include areas never injured.
These signs don’t show up on regular scans. That’s why so many people get dismissed. A 2023 survey found 63% of patients saw 4-6 doctors over 2-5 years before getting the right diagnosis.
It’s Not Just Pain - It’s Everything Else
People with central sensitization don’t just hurt. They feel overwhelmed. The nervous system isn’t just amplifying pain - it’s amplifying everything.Common extra symptoms include:
- Brain fog - trouble concentrating, memory lapses. Reported by 87% of patients.
- Sleep disruption - not just from pain, but from nervous system overdrive. 76% struggle with unrefreshing sleep.
- Sensory overload - bright lights, loud noises, strong smells become unbearable. Many avoid malls, restaurants, or even family gatherings.
- Anxiety and depression - not because they’re "mental," but because living in constant high-alert mode wears you down. Your nervous system is stuck in fight-or-flight.
Reddit threads from the r/Fibromyalgia community are full of stories: "I can’t wear jeans because the seam hurts," or "My partner hugged me and I cried - it felt like my bones were cracking." These aren’t exaggerations. They’re neurological realities.
How Is It Treated?
You can’t just take an NSAID and expect it to fix this. Central sensitization needs a different kind of treatment - one that targets the brain and spinal cord, not just the site of pain.Medications that work:
- Pregabalin (Lyrica) - 300-1200mg daily. Helps 55% of patients reduce pain by 30-50%.
- Duloxetine (Cymbalta) - 60mg daily. Reduces pain by 30% in 45% of users. Works by boosting serotonin and norepinephrine to calm the nervous system.
- Low-dose naltrexone (LDN) - 4.5mg at bedtime. Surprisingly effective for fibromyalgia. Reduces pain by 25-35% in 40% of users. It modulates immune activity in the brain.
- Nortriptyline - 25-50mg nightly. Helps with sleep and pain. Works better than most people expect.
Non-drug approaches:
- Graded exercise - start with 5-10 minutes of walking or swimming, increase by 10% per week. Too much too fast makes it worse. Too little does nothing. This slow build helps retrain the nervous system.
- Pain neuroscience education - learning how your nervous system works. One study showed this alone reduced pain catastrophizing scores by 20-30%. Knowing it’s not "all in your head" but a real, treatable change is powerful.
- Mindfulness and stress reduction - 8 weeks of mindfulness training improved pain interference scores by 25%. Stress fuels sensitization. Calming the mind calms the nerves.
- Therapeutic touch - gentle massage, acupuncture, or physical therapy that avoids overstimulation. The goal isn’t to "fix" the pain, but to teach the nervous system it’s safe.
Many people give up because treatments don’t work overnight. But progress is slow and steady. One woman in Seattle told me, "I didn’t get better. I got quieter. The pain didn’t vanish, but it stopped screaming. That was enough to start living again."

Why So Many Doctors Miss It
Central sensitization isn’t taught well in medical school. Most doctors are trained to look for structural problems: herniated discs, torn ligaments, arthritis. If the MRI looks normal, they assume it’s psychological.But the data says otherwise:
- Rheumatologists catch it in 65% of fibromyalgia cases.
- Neurologists spot it in 55% of chronic migraine patients.
- Orthopedic surgeons? Only 25% recognize it in chronic pain cases.
It’s a gap in training. A 2023 survey found only 45% of U.S. pain clinics had formal protocols for diagnosing central sensitization. That number is rising - to 78% now - but slowly.
And it’s not just about diagnosis. Medications have side effects. Dizziness, drowsiness, weight gain. One in three people quit because they can’t tolerate them. That’s why combining meds with movement, education, and stress management is key.
What’s Next?
The future is promising. Researchers are working on:- Biomarkers - testing spinal fluid for substance P or using PET scans to see reduced opioid receptor binding. These could one day replace guesswork with lab confirmation.
- Targeted drugs - five new compounds are in Phase II trials, designed to block specific pain pathways in the spinal cord.
- Neuroplasticity training - apps and programs that use biofeedback to help patients retrain their nervous system.
Dr. Clifford Woolf predicts that within the next decade, central sensitization will be recognized as the main cause of 30-40% of chronic pain cases - up from today’s 20-25%. That’s a massive shift.
For now, the most important thing is this: if you have unexplained, widespread, amplified pain - you’re not crazy. You’re not lazy. You’re not broken. Your nervous system got stuck. And like any stuck system, it can be unstuck - with the right understanding, the right tools, and the right patience.
Is central sensitization the same as fibromyalgia?
No. Fibromyalgia is a diagnosis based on symptoms like widespread pain and fatigue. Central sensitization is the underlying neurological mechanism that explains why those symptoms happen. Most people with fibromyalgia have central sensitization, but not everyone with central sensitization has fibromyalgia. It can also be present in chronic low back pain, migraine, and post-surgical pain.
Can central sensitization be reversed?
Yes - but it takes time and consistency. The nervous system is plastic, meaning it can rewire itself. Studies show that with the right combination of medication, graded exercise, and pain education, many people experience significant improvement. Some even reach near-normal pain sensitivity. It’s not a cure, but it’s reversible in most cases.
Why does my pain spread to areas that were never injured?
Because your spinal cord and brain have become hypersensitive. Pain signals from one area (like a sprained ankle) can activate nearby nerve pathways, causing the brain to interpret pain in nearby or even distant areas. This is called "spreading sensitization." It’s not imaginary - it’s a documented neurophysiological process.
Are opioids helpful for central sensitization?
Generally, no. Central sensitization involves reduced function of your body’s natural opioid system. Adding more opioids doesn’t fix this - and can make things worse over time. Opioids are not recommended for fibromyalgia or chronic pain driven by central sensitization. Medications like pregabalin, duloxetine, or low-dose naltrexone are far more effective.
Can stress make central sensitization worse?
Absolutely. Stress activates the sympathetic nervous system, which increases norepinephrine and inflammation in the spinal cord - both of which fuel central sensitization. Managing stress isn’t optional - it’s part of treatment. Techniques like mindfulness, breathing exercises, and pacing activities can reduce nervous system overdrive.
Why do some doctors say it’s "all in my head"?
Because they don’t understand it. Central sensitization doesn’t show up on X-rays or blood tests. But that doesn’t mean it’s not real. It’s a real change in how your brain and spinal cord process signals. Major medical organizations like the International Association for the Study of Pain and the American Academy of Family Physicians confirm it’s a physiological condition, not psychological. You’re not imagining it - your nervous system is misfiring.
How long does it take to see improvement?
Most people start noticing small changes in 4-8 weeks with consistent treatment. Significant improvement often takes 3-6 months. Progress isn’t linear - some days are better than others. But the goal isn’t to eliminate pain overnight. It’s to reduce its intensity, stop it from spreading, and regain function. Many people find they can return to work, hobbies, or family life even if some pain remains.

All Comments
Suzanne Johnston December 9, 2025
Central sensitization isn't just a medical condition-it's a revolution in how we understand pain. It's not broken hardware, it's corrupted software. Your nervous system learned to scream when it should whisper, and now it can't unlearn it. But here's the beautiful part: because it learned it, it can unlearn it too. Neuroplasticity isn't a buzzword-it's your lifeline. You're not broken. You're rewiring.
Graham Abbas December 10, 2025
OMG YES. I’ve been telling my GP this for years and he kept saying ‘it’s stress’ like I’m making it up. Then I read Woolf’s papers and cried because finally someone had the words. It’s not anxiety-it’s biology on fire. I had a 30% drop in pain after LDN and 10 mins of daily walking. Not cured. But quieter. That’s enough.
Elliot Barrett December 10, 2025
Literally just read this and I’m confused why we’re even discussing this. If your MRI is clean and you’re still in pain, you’re either malingering or you need a therapist. Pain is subjective, sure, but this sounds like pseudoscience dressed up with big words.
Shubham Mathur December 11, 2025
Bro this is real I lived it for 7 years no joke. I used to cry when my wife hugged me. I couldn't wear socks. My brain was stuck on 11. Then I found pain neuroscience education. Took 6 months. Now I can walk my dog without screaming. You don't need a miracle. You need consistency. And a doctor who doesn't think you're crazy. I'm not even on meds anymore. Just walking. And breathing. And knowing it's not my fault.
Ryan Brady December 13, 2025
So basically you're saying if you're not tough enough to handle pain you get a medal? 😂 We got real injuries in this country. People with torn ACLs and broken spines. This sounds like woke medicine for people who can't handle life. Just suck it up. 💪
Delaine Kiara December 14, 2025
Okay but have you considered that maybe it's not the nervous system? Maybe it's your aura? Or your chakras? Or maybe you're just holding onto trauma from your childhood? I mean, I read this whole thing and I'm like-what if it's not about biology at all? What if it's about your spirit? I had a similar thing after my divorce and I did sound baths and crystal grids and now I'm fine. Just saying. 🌈✨
Gilbert Lacasandile December 14, 2025
I just wanted to say thank you for writing this. I’ve been suffering for 9 years. My neurologist didn’t even know the term. I felt alone. Reading this made me feel seen. I’m trying LDN and graded exercise. It’s slow. But I’m trying. And that’s something.
Haley P Law December 15, 2025
My mom called me a hypochondriac for 12 years. Then I had a QST test and the tech said, ‘I’ve never seen a response like this.’ I screamed in the waiting room. Not from pain-from relief. I’m not crazy. I’m not weak. I’m just wired differently. And I’m not sorry for needing help.
Andrea DeWinter December 16, 2025
For anyone reading this and thinking 'I don't have fibromyalgia so this doesn't apply'-it does. I had chronic low back pain after a car accident. MRI showed nothing. Then I learned about central sensitization. I started graded exercise. Started with 5 minutes of water walking. Now I hike. The key is not pushing through pain but staying just under it. Slow. Steady. Safe. You don't need a miracle. You need a plan.
Angela R. Cartes December 16, 2025
Ugh. Another ‘pain is real’ post from the wellness cult. You people treat pain like a sacred mystery. It’s biology. If you can’t fix it with opioids or surgery, you’re just lazy. I’ve seen 30-year-olds on disability because they ‘can’t handle touch.’ Get a job. Get strong. Stop coddling yourself.
Andrea Beilstein December 17, 2025
Interesting how this mirrors ancient Ayurvedic concepts of vata imbalance-when the nervous system is too agitated, everything amplifies. The West just gives it fancy names and MRI scans. The solution? Still the same: calm the mind, move gently, eat clean. We knew this for 5,000 years. We just forgot.
Lisa Whitesel December 18, 2025
This is the exact reason medicine is collapsing. People are being told their pain is ‘real’ so they never have to take responsibility. No one wants to admit they’re depressed. So they invent neurological disorders. You’re not sensitized. You’re avoiding life. Get therapy. Stop blaming your brain.
Larry Lieberman December 19, 2025
Just got diagnosed last month. Started LDN. Took 3 weeks. First night I slept 7 hours. No meds. No screaming. Just… quiet. I’m not fixed. But I’m not drowning anymore. 🙏