RLS Medication Safety Checker
Check if your medication is safe for Restless Legs Syndrome. Many common allergy and cold medicines contain sedating antihistamines that worsen RLS symptoms. Enter any medication name below:
Antihistamines are commonly used to treat allergies, colds, and sleep issues-but for people with Restless Legs Syndrome (RLS), many of these drugs can make symptoms far worse. If you’ve ever taken Benadryl for a stuffy nose and then spent the night pacing your bedroom because your legs felt like they were on fire, you’re not alone. Thousands of RLS patients report the same experience. The problem isn’t just coincidence-it’s biology.
Why Sedating Antihistamines Make RLS Worse
Restless Legs Syndrome causes uncomfortable sensations in the legs-tingling, crawling, aching-usually at night or when sitting still. The urge to move them is overwhelming. It’s not just annoyance; it disrupts sleep, drains energy, and lowers quality of life. Research shows RLS is tied to dopamine dysfunction in the brain. Dopamine helps control movement and signals when your body is at rest. When dopamine pathways are disrupted, RLS symptoms flare up. Sedating antihistamines like diphenhydramine (Benadryl), doxylamine (in Unisom and NyQuil), chlorpheniramine, and hydroxyzine cross the blood-brain barrier easily. Once inside, they don’t just block histamine-they also interfere with dopamine receptors. This double hit worsens RLS. A 2014 study of over 16,000 kidney patients found those taking these antihistamines were nearly twice as likely to develop or worsen RLS symptoms. The effect was strong enough to be statistically significant even after adjusting for other factors like dialysis time. The Houston Methodist Movement Disorders Clinic tracked over 1,000 RLS patients and found that 78% saw symptoms spike after using sedating antihistamines. One patient, ‘RLSsurvivor’ on the RLS Foundation forum, wrote: ‘I took Benadryl for allergies and couldn’t sleep for 3 nights straight-my legs felt like they were on fire. Switched to Claritin and symptoms improved within 24 hours.’ That’s not an outlier. It’s a pattern.What’s in Your Medicine Cabinet?
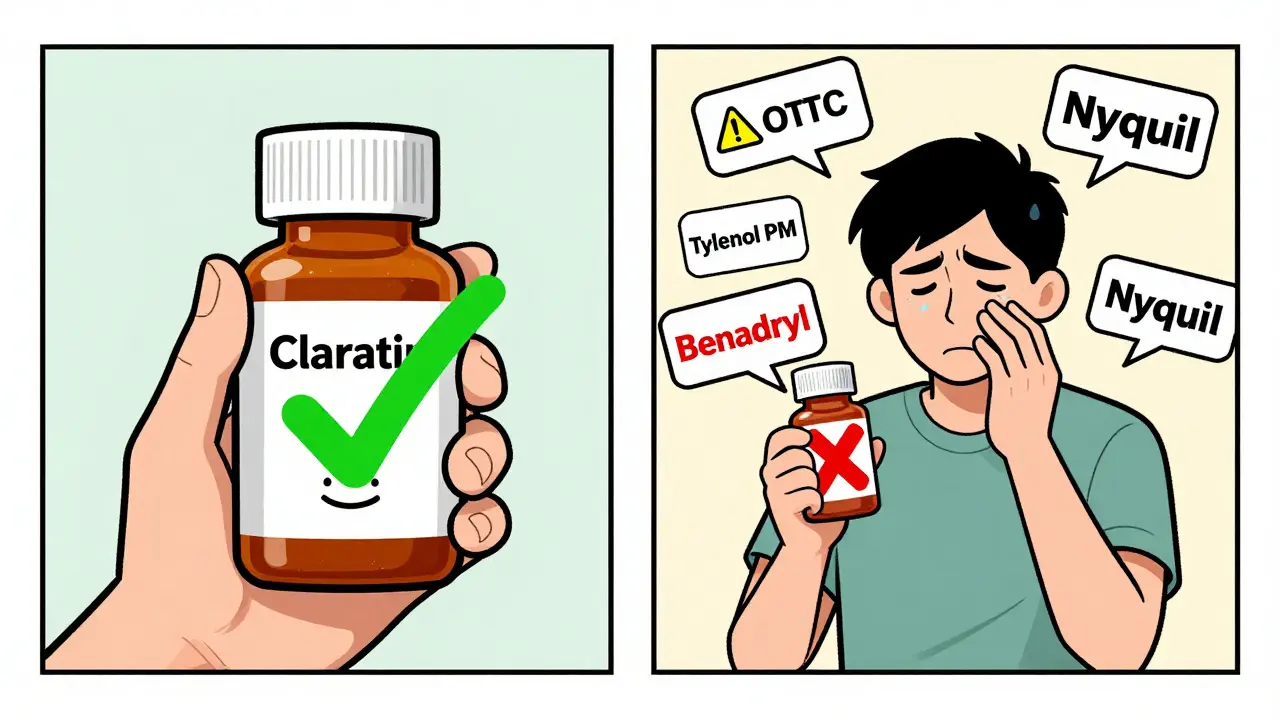
Many over-the-counter products hide sedating antihistamines under different names. You might think you’re just taking a cold remedy or a sleep aid-but you’re triggering RLS. Common culprits include:- Benadryl (diphenhydramine)
- Unisom SleepTabs (doxylamine)
- Tylenol PM (acetaminophen + diphenhydramine)
- Bayer PM (aspirin + diphenhydramine)
- Advil PM (ibuprofen + diphenhydramine)
- Comtrex, Contact, Dimetapp, TheraFlu, Triaminic, Vicks Cough and Cold Products
Non-Sedating Antihistamines: The Safer Choice
The good news? Not all antihistamines are created equal. Second-generation antihistamines like fexofenadine (Allegra), loratadine (Claritin), desloratadine (Clarinex), and cetirizine (Zyrtec) were designed to stay out of the brain. They’re filtered by a protein called P-glycoprotein that keeps them from crossing the blood-brain barrier. That means less interference with dopamine. According to RLS Foundation patient surveys from 2019:- Only 5-8% of RLS patients reported worsened symptoms with non-sedating antihistamines
- 87% of those who switched from sedating to non-sedating versions saw improvement or stability
Watch Out for Hidden Triggers
It’s not just antihistamines. Many allergy and cold products combine them with decongestants like pseudoephedrine or phenylephrine. These stimulants can also make RLS worse. A 2016 RLS-UK database found that 35% of RLS patients experienced symptom flare-ups from decongestants alone. So even if a product says “non-drowsy,” check the label. If it contains pseudoephedrine, skip it. Products like Sudafed, Claritin-D, Zyrtec-D, and many store-brand cold formulas fall into this category. The RLS Foundation warns: “D” means decongestant-and decongestants are not safe for RLS.What Can You Take Instead?
You don’t have to suffer through allergies or sleepless nights. Here are safer alternatives:- Nasal corticosteroids like fluticasone (Flonase) or mometasone (Nasonex): These reduce nasal inflammation without entering the brain. A 2019 Vanderbilt study showed 82% of RLS patients had better allergy control with these sprays.
- Saline nasal irrigation: Using a neti pot or squeeze bottle with salt water clears allergens naturally. 76% of RLS patients in RLS Foundation surveys found this helpful.
- Melatonin: If you need help sleeping, melatonin (0.5-5 mg) is a safer option than antihistamines. A 2021 international guideline found 65% of RLS patients benefited without worsening symptoms.
- Prescription nasal antihistamines: Azelastine (Astelin) is a nasal spray that works locally and doesn’t affect dopamine. It’s approved for allergic rhinitis and avoids systemic side effects.
How to Check Your Medications
Reading labels is the first step. But it’s not always easy. Look for these active ingredients:- AVOID: diphenhydramine, doxylamine, chlorpheniramine, hydroxyzine, promethazine
- SAFE: fexofenadine, loratadine, desloratadine
- USE WITH CAUTION: cetirizine
- AVOID: pseudoephedrine, phenylephrine

What If You’ve Already Taken One?
If you took Benadryl or a similar drug and your legs are screaming, don’t panic. Symptoms usually improve within 24-48 hours after stopping. Stay hydrated, avoid caffeine, and try gentle stretching or a warm bath. Some patients find relief with a magnesium supplement (200-400 mg), though evidence is mixed. If symptoms persist beyond two days, talk to your doctor. You may need a short-term prescription to reset your system.Why This Matters Now
The connection between antihistamines and RLS is no longer a hidden secret. In 2019, the FDA required updated warnings on prescription antihistamines with central nervous system effects. Medicare Part D now covers second-generation antihistamines with 98% formulary inclusion-meaning they’re affordable and accessible. Sales of non-sedating antihistamines rose 12.7% between 2016 and 2022, while sedating ones dropped 4.3%. Why? Because patients are speaking up. Doctors are listening. And awareness is growing. A 2023 European study found that proper medication choices improved RLS-specific quality of life scores by over 32 points on a 100-point scale. That’s not just a number-it’s more sleep, less pain, and better days.Final Advice
If you have Restless Legs Syndrome:- Never take Benadryl, Unisom, or NyQuil without checking with your doctor.
- Switch to Claritin, Allegra, or Clarinex for allergies.
- Use Flonase or saline rinses instead of oral meds.
- Read every label-especially for “PM,” “Night,” or “Cold & Flu” products.
- Keep a symptom journal. Note when you take any new medication and how your legs feel.
Can antihistamines cause Restless Legs Syndrome?
Antihistamines don’t cause RLS in people who don’t already have it, but they can trigger or worsen symptoms in those who do. Sedating antihistamines like diphenhydramine interfere with dopamine pathways in the brain, which are already impaired in RLS. This makes symptoms more intense and harder to manage.
Is Zyrtec safe for people with Restless Legs Syndrome?
Cetirizine (Zyrtec) is generally safer than Benadryl, but it’s not risk-free. About 15% of RLS patients report mild symptom worsening with Zyrtec, compared to just 5% with Claritin or Allegra. If you’re sensitive, try Claritin or Allegra first. If Zyrtec works without worsening symptoms, it may still be an option-but monitor closely.
What cold medicine is safe for Restless Legs Syndrome?
Avoid any cold medicine with diphenhydramine, doxylamine, or pseudoephedrine. Safe options include plain saline nasal spray, fluticasone (Flonase), or single-ingredient loratadine (Claritin). For fever or pain, use plain acetaminophen or ibuprofen without added antihistamines or decongestants.
Does melatonin help with RLS and allergies?
Melatonin doesn’t treat allergies, but it’s a safe sleep aid for RLS patients. Unlike sedating antihistamines, it doesn’t block dopamine. Studies show 65% of RLS patients benefit from 0.5-5 mg of melatonin without worsening symptoms. Use it for sleep, not for nasal congestion.
How long does it take for RLS symptoms to improve after stopping Benadryl?
Most people notice improvement within 24 to 48 hours after stopping a sedating antihistamine. The drug leaves the system quickly, but dopamine function takes a little longer to reset. If symptoms don’t improve after two days, consult your doctor-other factors may be involved.

All Comments
Alex Ronald December 30, 2025
Just switched from Benadryl to Claritin last month after my RLS went full nuclear for three nights. Holy hell, what a difference. No more pacing at 3 AM. I didn’t even realize how much I was suffering until it was gone. Seriously, if you’re on sedating antihistamines and have RLS-just switch. It’s the easiest win you’ll ever get.
Nicole K. December 30, 2025
You people are so lazy. Just stop taking meds altogether. My grandma never took anything for allergies and she lived to 98. You’re all just addicted to chemicals and now you want the world to cater to your ‘RLS’ like it’s a disability. Get over it.
Fabian Riewe December 31, 2025
Big shoutout to the OP for making this so clear. I used to think ‘PM’ just meant ‘good for sleep’-turns out it meant ‘good for making your legs feel like they’re being stabbed by tiny spiders.’ I switched to Flonase and now I actually sleep. Also, saline rinse? Game changer. No more nose bombs, no more leg bombs. Win-win.
Amy Cannon January 1, 2026
As a long-time resident of the American South and a devotee of traditional herbal remedies, I must say that the modern pharmacological landscape has become increasingly… disconcerting. While I appreciate the data presented, I cannot help but recall my great-aunt’s use of chamomile tea and honey for nasal congestion, which, while perhaps less efficacious in a clinical trial, carried no risk of dopaminergic interference. One must ask: are we truly better off with pills that promise convenience but steal our nights? I think not. And while I may have misspelled ‘dopaminergic’-it’s still the truth.
Himanshu Singh January 2, 2026
Man, this post saved my life. I was takin Zyrtec and thought it was fine, but my legs were actin weird. Switched to Allegra and boom-no more 3am dance party. Also, dont forget magnesium! I take 400mg before bed and it helps a lot. Thanks for the info, really!
Greg Quinn January 4, 2026
It’s funny how we treat symptoms like enemies when they’re just signals. RLS isn’t a flaw-it’s your nervous system screaming that something’s off. Antihistamines don’t ‘cause’ it, but they amplify the noise. The real question isn’t which drug to take, but why we keep treating the body like a machine we can tweak with chemicals instead of listening to what it’s trying to tell us. Maybe the answer isn’t just safer meds… but a quieter life.
Lisa Dore January 5, 2026
Hey everyone-just wanted to say thank you to the OP and everyone sharing. I’ve been dealing with RLS for 12 years and this is the first time I’ve seen a post that actually helps me feel less alone. I switched to Claritin last year and started using a neti pot. I still have bad nights, but now I know what’s triggering them. You’re not crazy. You’re not broken. You just need better info. Keep speaking up. We’re all in this together.
Sharleen Luciano January 6, 2026
How is it that the average person can’t read a label? I mean, really. If you’re taking something labeled ‘PM’ or ‘Nighttime’ and you have a neurological disorder, you’re not ‘suffering from RLS’-you’re suffering from poor decision-making. This isn’t rocket science. It’s basic pharmacology. If you can’t distinguish between ‘diphenhydramine’ and ‘loratadine,’ maybe you shouldn’t be self-medicating at all. Just sayin’.
Jim Rice January 7, 2026
Wow. So now we’re told Benadryl is evil? Next thing you know, they’ll ban caffeine because it makes people jittery. This is pure fearmongering. I’ve taken Benadryl for 20 years. My legs are fine. You’re all just hypochondriacs looking for an excuse to feel special. Maybe your RLS is just stress. Try yoga. Or better yet-stop complaining.
Henriette Barrows January 7, 2026
I had no idea Zyrtec could be a problem. I thought it was ‘non-drowsy’ so it was safe. But I’ve been having weird leg twitches lately… I’ll switch to Claritin tomorrow. Also, the melatonin tip? I’ve been taking it for sleep anyway. So glad I’m not the only one. Thank you for writing this. I feel like I finally have a roadmap.