Every year in the U.S., more than 56,000 people end up in the emergency room because of an acetaminophen overdose. Many of them didn’t mean to take too much. They just didn’t realize how easy it is to go over the limit-especially when mixing pills, cold medicines, and prescription painkillers. Acetaminophen is in more than 600 products, from Tylenol to Vicodin to nighttime sleep aids. And the damage it does to the liver doesn’t always show up right away. By the time you feel sick, it might already be too late.
How Acetaminophen Turns Toxic
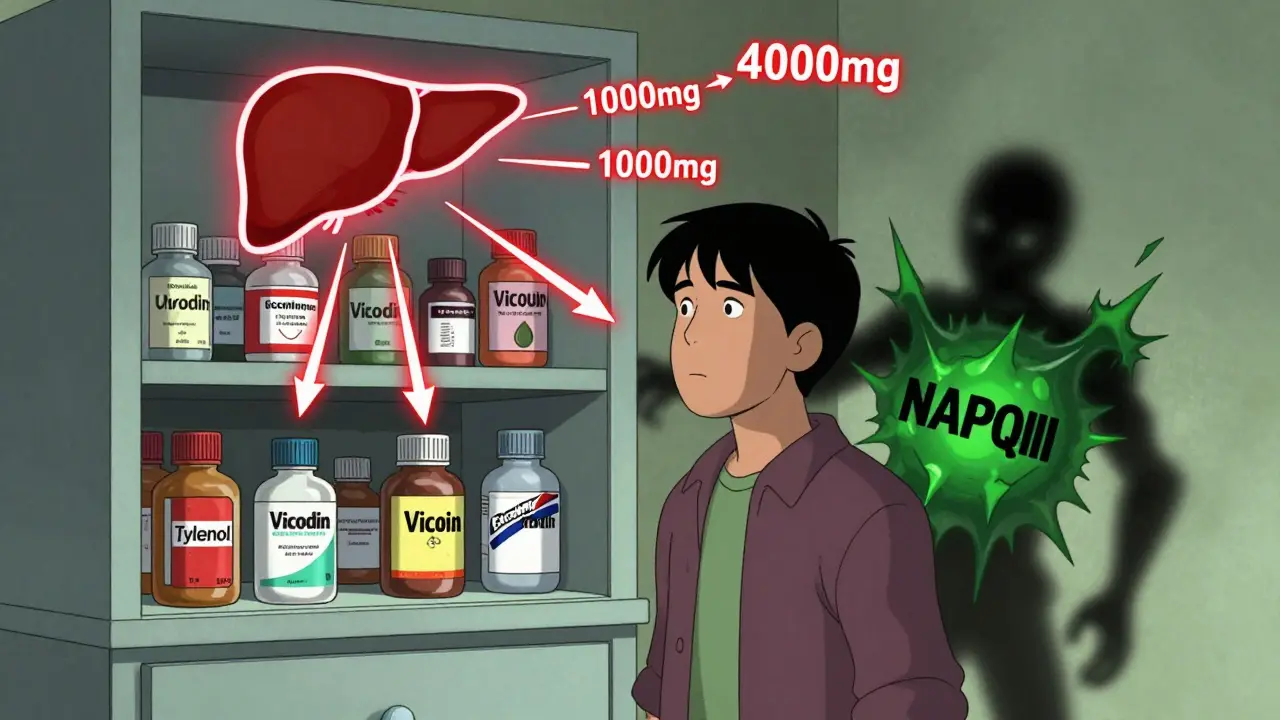
Acetaminophen is safe when taken as directed. Your liver breaks it down using enzymes and neutralizes the toxic byproduct, NAPQI, with a molecule called glutathione. But when you take too much-more than 4,000 mg in 24 hours-that system gets overwhelmed. Glutathione runs out. NAPQI starts attacking liver cells. The damage begins silently. You might not feel a thing for hours.
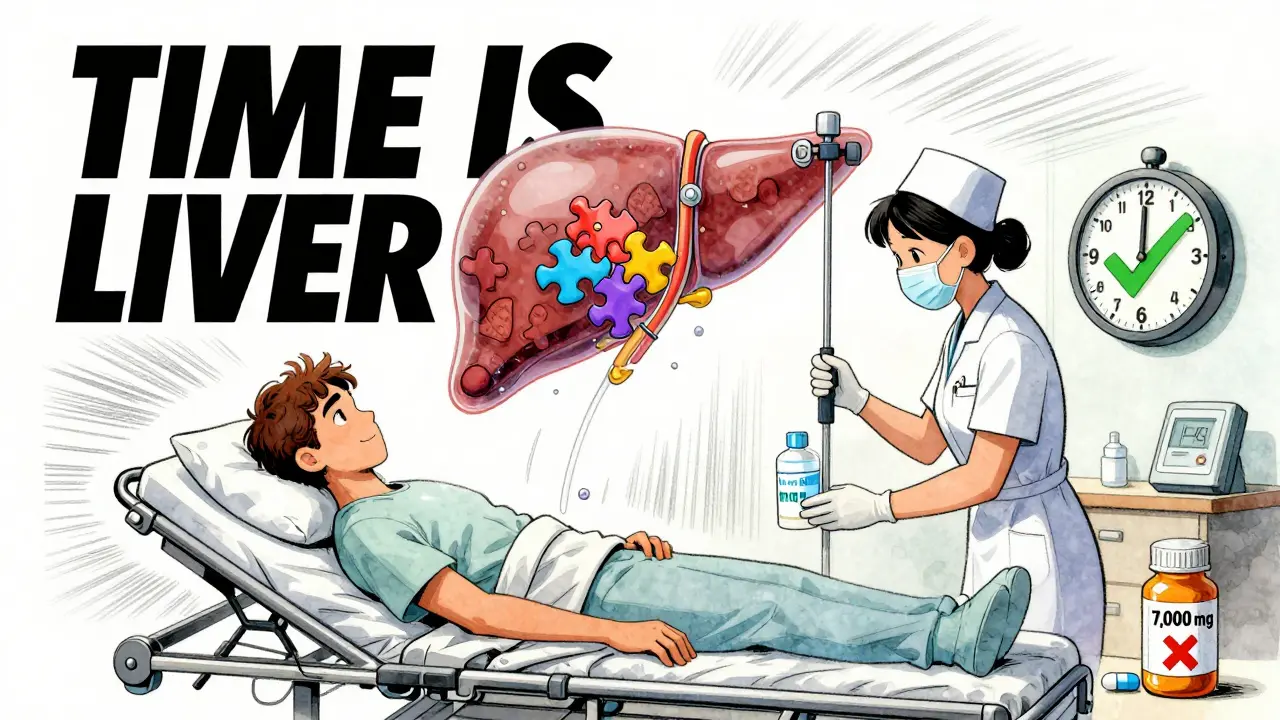
Even a single dose of 7,000 mg can be dangerous. That’s just 14 regular 500 mg pills. And if you drink alcohol regularly, your risk jumps 3 to 4 times higher. Same if you have hepatitis B or C, are malnourished, or take seizure meds like carbamazepine. These things deplete glutathione or speed up toxin production. You don’t need to take a whole bottle to overdose. Sometimes, just a few extra pills over a day or two is enough.
The Four Stages of Liver Damage
There’s a clear timeline to how acetaminophen poisoning unfolds. Knowing these stages could save your life-or someone else’s.
Stage 1: 0-24 hours - You might feel fine. Or you might have mild nausea, vomiting, or loss of appetite. About 4 in 10 people feel nothing at all. This is the most dangerous stage because you’re tempted to wait and see. Don’t. If you took too much, this is your last chance to stop the damage before it spreads.
Stage 2: 24-72 hours - Nausea and vomiting return, often worse. Pain starts in the upper right side of your abdomen, where your liver sits. Your blood tests will show rising ALT levels-sometimes over 1,000 IU/L (normal is under 56). Your liver is starting to die. But you might still feel okay enough to delay going to the hospital. Don’t.
Stage 3: 72-96 hours - This is the crisis point. Jaundice (yellow skin and eyes) appears in over 90% of severe cases. Your blood can’t clot properly (INR above 1.5). Your kidneys start to fail. You might feel confused, drowsy, or disoriented. ALT levels can spike above 10,000 IU/L. At this point, you’re in acute liver failure. Without treatment, death is likely.
Stage 4: After 5 days - Recovery or death. If you got treatment early, 85-90% of people recover fully. Your liver regenerates. If you waited too long, multi-organ failure sets in. About 1-2% of cases need a liver transplant. Survival after transplant is about 85% at five years.
What to Do If You Think You Overdosed
If you took too much acetaminophen-whether it was 3 pills too many or a whole bottle-go to the ER now. Don’t wait for symptoms. Don’t call your doctor tomorrow. Don’t try to “sleep it off.”
The only antidote is N-acetylcysteine, or NAC. It works by replacing the glutathione your liver lost and mopping up the toxic NAPQI. But it only works well if given early.
- If you get NAC within 8 hours: 98% effective.
- If you get it between 8-15 hours: drops to 75%.
- If you wait past 15 hours: only 55% effective.
Every hour of delay increases your risk of liver failure by 8.5%. That’s why the first 8 hours are critical.
In the ER, they’ll check your blood acetaminophen level and plot it on the Rumack-Matthew nomogram. If it’s above 150 µg/mL at 4 hours, you’ll get NAC. They might also give you activated charcoal if you took the pills within the last 1-2 hours. IV fluids, anti-nausea meds, and vitamin K are standard too.
Even if you show up 24-48 hours later with liver damage, NAC still helps. It doesn’t reverse damage, but it can stop it from getting worse and support recovery.

When a Liver Transplant Is Needed
Some people don’t respond to NAC. Their liver keeps failing. Doctors use the King’s College Criteria to decide who needs a transplant:
- pH below 7.3
- INR above 6.5
- creatinine above 3.4 mg/dL
If all three are present, survival without a transplant is near zero. About 1-2% of acetaminophen overdose cases reach this point. Transplants save lives-but they’re not guaranteed. You’ll need to be evaluated quickly, and a donor liver must be found.
Why People Overdose Without Realizing It
The biggest reason people overdose? They don’t know how many products contain acetaminophen.
One Vicodin tablet has 300 mg. One Excedrin has 500 mg. One NyQuil has 650 mg. Take two Vicodin, one Excedrin, and a night of NyQuil? That’s 1,650 mg-nearly half the daily limit. Do that for three days? You’ve hit 5,000 mg. And you didn’t even take a single Tylenol.
Surveys show 68% of people don’t know prescription painkillers contain acetaminophen. They think they’re safe because it’s “just” a cold medicine or a pain pill. They don’t check labels. They don’t add it up.
Also, many people think “more is better.” If 500 mg helps with a headache, maybe 1,000 mg helps more. But your liver doesn’t work that way. It can’t handle extra. The dose-response curve flattens after a point. More pills don’t mean more pain relief-they mean more liver damage.
What’s New in Treatment
Research is moving fast. A 2023 study from Harvard Stem Cell Institute found that nitric oxide helps the liver regenerate on its own-even after heavy damage. In mice and zebrafish, it boosted healing without needing more NAC. That could mean longer treatment windows in the future.
Another breakthrough is a blood test for microRNA-122. It rises within 2 hours of overdose and is 94% accurate at detecting liver injury. Right now, doctors wait 4-6 hours for acetaminophen levels to show up. With this test, ERs could confirm damage within hours-even before symptoms appear. Clinical trials are underway.
How to Prevent an Overdose
Prevention is simple, but you have to be smart.
- Never exceed 4,000 mg per day. Many experts now say 3,000 mg is safer, especially if you drink alcohol or have liver issues.
- Check every medicine label. Look for “acetaminophen,” “APAP,” or “paracetamol.”
- Don’t mix painkillers. If you’re taking a prescription opioid, assume it has acetaminophen unless it says otherwise.
- Know your limits. If you drink alcohol daily, cut your acetaminophen dose in half-or avoid it entirely.
- Keep track. Write down what you take and when. Use a phone app if you need to.
The FDA made changes in 2011 to help: prescription combo pills now max out at 325 mg acetaminophen per tablet instead of 750 mg. That cut overdose-related liver failure by 21% between 2005 and 2016. But OTC products still allow up to 1,000 mg per pill. That’s why education matters.
Recovery and Long-Term Outlook
If you survive an overdose and get treated in time, your liver will heal. Most people recover fully within 3 months. Blood tests return to normal. No scarring. No long-term issues.
But 8% of survivors have mild, ongoing liver enzyme elevations. They need to be monitored. They should avoid alcohol and high-dose acetaminophen forever.
And yes, the cost is high. The average hospital stay for an acetaminophen overdose costs $38,500. That’s not counting lost wages or follow-up care. Prevention isn’t just about health-it’s about money too.
Acetaminophen is one of the safest drugs when used right. But it’s also one of the deadliest when misused. You don’t need to be suicidal to overdose. You just need to be unaware. Know the signs. Know the limits. Know what’s in your medicine cabinet.
Can you overdose on acetaminophen by taking too many cold medicines?
Yes, absolutely. Many cold, flu, and sleep medicines contain acetaminophen. Taking Tylenol plus NyQuil plus a prescription painkiller can easily push you over 4,000 mg in a day. Always check the active ingredients on every bottle. If acetaminophen (or APAP) is listed, don’t take another product with it.
Is it safe to take acetaminophen if I drink alcohol?
If you drink alcohol regularly-even just a few drinks a week-your risk of liver damage from acetaminophen triples. The liver uses the same enzymes to break down both. Alcohol depletes glutathione, making it harder for your body to detoxify acetaminophen. If you drink, stick to no more than 2,000-3,000 mg per day, or avoid it entirely. If you binge drink, don’t take any acetaminophen for at least 24 hours after.
What if I took too much but don’t feel sick yet?
Go to the ER immediately. The first 24 hours are often symptom-free, but liver damage is already starting. Waiting until you feel bad means it’s too late for the most effective treatment. NAC works best within 8 hours. Don’t rely on how you feel. Get tested.
Can NAC be taken at home instead of going to the hospital?
No. Oral NAC is not a substitute for emergency care. It takes 72 hours to complete the full oral course, and you need medical monitoring for side effects like vomiting, low blood pressure, or allergic reactions. IV NAC in the hospital is faster, safer, and more effective. Even if you have NAC at home, call 911 or go to the ER. This is a medical emergency.
How do I know if a painkiller contains acetaminophen?
Look for “acetaminophen,” “APAP,” or “paracetamol” on the label. Common brand-name combo pills include Vicodin (hydrocodone + acetaminophen), Percocet (oxycodone + acetaminophen), and Tylenol #3 (codeine + acetaminophen). Even some non-prescription products like Excedrin and Midol contain it. If you’re unsure, ask your pharmacist or check the drug’s FDA-approved label online.
Is acetaminophen safer than ibuprofen for the liver?
Acetaminophen is easier on the stomach and kidneys than ibuprofen, but it’s far more dangerous for the liver. Ibuprofen can cause stomach bleeding or kidney issues with long-term use, but it doesn’t cause acute liver failure like acetaminophen does. If you have liver disease, avoid acetaminophen entirely. Ibuprofen may be safer-but still use it sparingly and under medical guidance.
What to Do Next
If you’ve ever taken more than one painkiller at once, check your medicine cabinet right now. Look at every bottle. Write down how much acetaminophen is in each. Add it up. If you’re close to 4,000 mg, you’re at risk.
Set a reminder on your phone: “Check labels before taking meds.” Keep a log. Talk to your pharmacist. If you’re on long-term pain meds, ask your doctor if you can switch to ones without acetaminophen.
And if you ever suspect an overdose-no matter how small it seems-don’t wait. Call 911 or go to the nearest ER. Your liver can’t wait. Neither should you.

All Comments
Lori Anne Franklin December 27, 2025
I had no idea so many cold meds had acetaminophen in them... I take NyQuil when I'm sick and sometimes Tylenol if my head kills me. Guess I'm lucky I never went over. 😅 Thanks for the wake-up call!
Bryan Woods December 28, 2025
This is an exceptionally well-researched and clearly articulated summary of acetaminophen toxicity. The staging system is particularly valuable for clinical awareness, and the inclusion of the Rumack-Matthew nomogram demonstrates a high level of medical literacy in public communication.
Zina Constantin December 30, 2025
If you're reading this and you've ever mixed painkillers without checking labels-you're not alone. I did it too. But now I have a sticky note on my medicine cabinet that says 'APAP = DANGER ZONE'. Spread this info. Save someone's liver. 💪
Angela Spagnolo December 30, 2025
I... I didn't realize... I mean, I knew acetaminophen was in a lot of stuff, but I never thought about adding it up... I take Excedrin for migraines, and sometimes NyQuil when I'm congested... oh my god. I think I might have crossed the line before... I'm checking my cabinet right now.
Sarah Holmes January 1, 2026
This post is a textbook example of how pharmaceutical companies exploit public ignorance. They market acetaminophen as 'safe' while burying it in 600+ products, knowing full well that the average person cannot track cumulative dosages. This isn't negligence-it's systemic malfeasance. And now we're supposed to be grateful for a 'warning'?
christian ebongue January 1, 2026
NAC works best in 8 hrs? So if you take 14 pills at 2am, don't wait till morning. Go now. Or just... don't take 14 pills. 🤦♂️
jesse chen January 2, 2026
I used to think 'natural remedies' were safer... until I learned my grandma was taking 3 different OTC meds every night, all with APAP. She never felt sick until she was in ICU. I wish I'd known sooner. This info could have saved her.
Joanne Smith January 3, 2026
So basically, acetaminophen is the silent assassin of the medicine cabinet. One minute you're popping pills like Skittles to get through a bad week, the next you're begging for a liver transplant. And the worst part? You won’t even feel it coming. It’s like a vampire... but with a pharmacy receipt.
Prasanthi Kontemukkala January 3, 2026
In India, many people use paracetamol without knowing it’s the same as acetaminophen. I’ve seen families give it to kids for fever and then add more because 'it’s not working'. This post should be translated and shared everywhere. Knowledge saves lives.
Alex Ragen January 3, 2026
The fact that we need a 2,000-word essay to explain that 'more pills ≠ better pain relief' speaks volumes about the erosion of basic pharmacological literacy in modern society. One wonders if the FDA’s 325mg cap was merely performative reform, designed to placate the public while allowing the same toxicity to persist under different packaging.
wendy parrales fong January 4, 2026
I used to think if I didn't feel sick, I was fine. But now I know that’s how your liver dies. Quiet. Alone. No warning. I’m gonna start writing down everything I take. It’s not that hard. Just a little notebook. Maybe it’ll save me one day.
Jeanette Jeffrey January 6, 2026
Lol. You people think you’re so smart because you read a medical article. Meanwhile, your cousin is still taking Tylenol with whiskey because 'it helps me sleep'. This isn't about knowledge-it's about people refusing to change. You can give them facts, but you can't give them common sense.
Shreyash Gupta January 6, 2026
I think the real problem is that we’re taught to 'treat symptoms' not 'listen to our body'. Why do we pop pills for every little ache? Maybe we should just rest. Or drink water. Or go outside. 🌿 But nope, we want a quick fix. So now we’re poisoning our livers. 😔💊